Patient Story
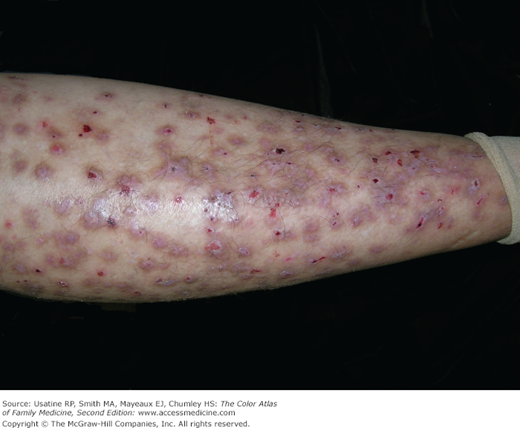
A 55-year-old woman presents with severe itching on her arms and legs. The itching disrupts her sleep and she sometimes scratches her arms and legs until exhaustion (Figures 149-1 and 149-2).1 She had used moisturizers, emollients, and topical corticosteroids, but they only alleviated the itching temporarily. The itching began 10 months earlier after finalizing the divorce from her husband of 20 years. The patient’s right leg had been amputated above the knee after a car accident, and she now wore a prosthetic leg. The patient readily admitted to a great deal of psychological distress. She described feeling depressed since her divorce, and the loss of her leg further aggravated her situation. She has had difficulty securing a job and had high anxiety about being able to pay for rent and bills. The diagnosis made was neurotic excoriations (neurodermatitis) and the patient understood that she was doing this to her own skin. The patient improved with nail cutting, acknowledging the self-inflicted nature of her excoriations and topical clobetasol. One year later, the patient was working in the hospital laboratory with a tremendous improvement in her skin condition (Figure 149-3).
Introduction
The self-inflicted dermatoses (sometimes referred to as psychogenic dermatoses) include neurotic excoriations, lichen simplex chronicus, and prurigo nodularis. These conditions are caused by pruritus for which no medical cause is apparent, which initiates an itch-scratch cycle. The self-inflicted dermatoses can present a challenge to the clinician, as multiple underlying medical etiologies must be ruled out to arrive at their diagnosis and the pathophysiology of these diseases is not well understood. In addition, they may be difficult to treat successfully. There is no clear standard of care for treatment, although a vast array of treatments targeting different etiologies has been tried clinically, and many have some amount of research to support them. As with other psychosomatic conditions, non-pharmacologic interventions, including the physician-patient relationship itself, can be important to treatment.
Synonyms
Epidemiology
- Studies show that neurotic excoriations primarily affect females, with a mean onset between the ages of 30 and 45 years1 (Figures 149-1, 149-2, 149-3, 149-4, and 149-5).
- Neurotic excoriations are present in 2% of patients seen in dermatologic clinics.1
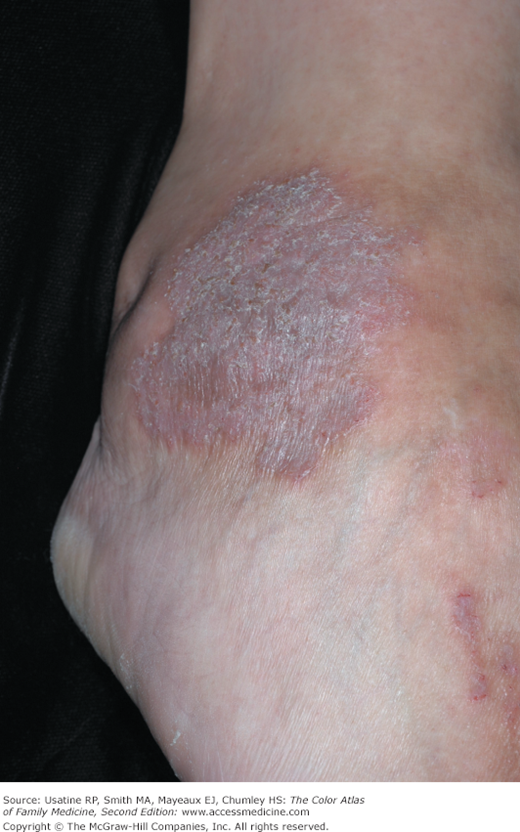
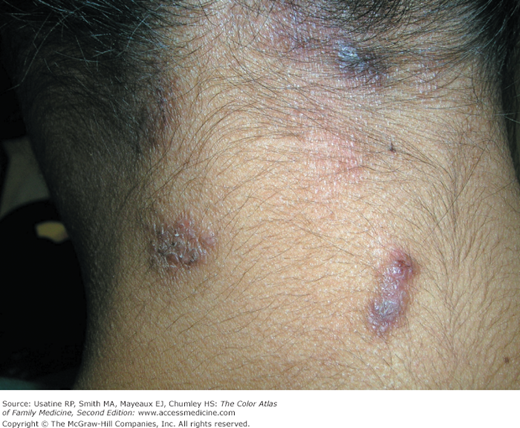
- Lichen simplex chronicus (LSC) is observed more commonly in females than in males (Figures 149-6, 149-7, 149-8, and 149-9). Lichen nuchae is a form of lichen simplex that occurs on the midposterior neck (Figures 149-8 and 149-9).
- LSC occurs mostly in mid-to-late adulthood, with highest prevalence in persons ages 30 to 50 years.2
- For prurigo nodularis (PN) there is no documented difference in frequency between males and females. PN most often occurs in middle-aged and older persons3 (Figures 149-10, 149-11, 149-12, 149-13, 149-14, and 149-15).
Figure 149-11
Prurigo nodularis on the arms and legs after 9 months of unsuccessful treatment in the patient in Figure 149-10. (Courtesy of Richard P. Usatine, MD.)