Patient Story
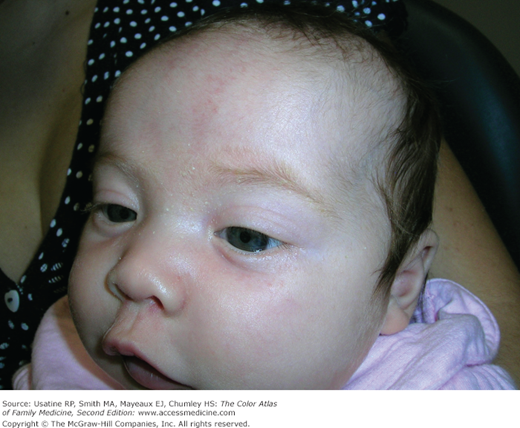
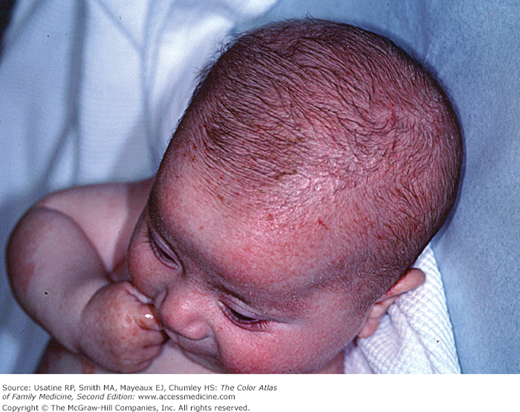
A 59-year-old man presents with a 3-month history of an itchy rash on his face (Figures 151-1 and 151-2). He states that he has had this rash intermittently for many years, but that it had recently worsened. He denies any major risk factors for HIV and does not have Parkinson disease. He has been under more stress lately and has noticed that this rash flares when under increased stress. Note the scale visible on the forehead and under the eyebrows and beard. There is also some mild erythema on the cheeks and around the nasolabial folds. The diagnosis of seborrheic dermatitis is made and treatment is begun with appropriate topical agents to treat the inflammation and the Malassezia. On the following visit, the patient has complete clearance of his seborrheic dermatitis.
Introduction
Seborrheic dermatitis is a common, chronic, relapsing dermatitis affecting sebum-rich areas of the body. Infants and adults, men and women may be affected. Presentation may vary from mild erythema to greasy scales, and, rarely, as erythroderma. Treatment is targeted to reduce inflammation and irritation, as well as to eliminate Malassezia fungus, whose exact role is not completely understood.
Epidemiology
- Seborrheic dermatitis is most commonly seen in male patients ages 20 to 50 years. The prevalence is approximately 3% to 5% in healthy young adults who are HIV-negative.1 More people may be affected, but many do not seek medical attention for mild cases.
- The prevalence is higher in immunocompromised persons (e.g. HIV-positive/AIDS); however, the vast majority of affected persons have a normal immune system.
- More common in persons with Parkinson disease.
- Infants can have seborrhea of the scalp (cradle cap), face, and diaper area.
Etiology and Pathophysiology
- Seborrheic dermatitis is a chronic, superficial, localized inflammatory dermatitis that is found in sebum-producing areas of the body.
- The actual cause of seborrheic dermatitis is not well-understood. It appears to be related to the interplay between host susceptibility, environmental factors, and local immune response to antigens.2–4
- Patients with seborrheic dermatitis may be colonized with certain species of lipophilic yeast of the genus Malassezia (also called Pityrosporum). However, Malassezia is considered normal skin flora and unaffected persons also may be colonized.
- Recent evidence suggests that Malassezia may produce different irritants or metabolites on affected skin.4
Risk Factors
Diagnosis
The clinical diagnosis is made by history and physical examination. Figures 151-1 and 151-2 reveal erythema and scale across the eyebrows, cheeks, and under beard. Biopsy is not generally indicated unless ruling out other possibilities (see Differential Diagnosis below).
- Chronic skin condition characterized by remissions and exacerbations.
- Poorly demarcated, erythematous plaques of greasy, yellow scale (Figure 151-3), in the characteristic seborrheic distribution (see description below).
- Common precipitating factors are stress, immunosuppression, and cold weather.
- Face, scalp, and ears may be very pruritic.
- May be the presenting sign of HIV seropositivity
- In dark-skinned individuals, the involved skin and scale may become hyperpigmented (Figure 151-4).
Scalp (i.e., dandruff), eyebrows (Figures 151-5 and 151-6), nasolabial creases, forehead, cheeks, around the nose, behind the ears (Figure 151-7), external auditory meatus, and under facial hair (Figure 151-8). Seborrhea can also occur over the sternum and in the axillae, submammary folds, umbilicus, groin, and gluteal creases.
Infants may develop scales on the scalp, known as cradle cap (Figure 151-9). The eyebrows may also be affected (Figure 151-5). Some infants have a wider distribution involving the neck creases, armpits, or groin.