Schwannoma
Amitabh Srivastava, MD
Key Facts
Terminology
Encapsulated, benign peripheral nerve sheath tumor composed predominantly of Schwann cells
Clinical Issues
Common between 20-50 years of age
Affects males and females equally
Surgical excision is curative
Macroscopic Features
Typically presents as eccentric mass loosely attached to underlying nerve
Microscopic Pathology
Hallmark: Variable amounts of hypercellular Antoni A and hypocellular Antoni B areas
Spindle cells in short fascicles in Antoni A areas
Loose matrix with cystic change and inflammatory cells in Antoni B areas
Bland nuclear features in most instances; degenerative nuclear atypia in “ancient” schwannoma
Cellular schwannoma may mimic MPNST
Plexiform schwannoma usually seen in children
Epithelioid schwannoma may be mistaken for smooth muscle tumor
Melanotic/psammomatous schwannoma often associated with Carney syndrome
Schwannomas in NF2 and schwannomatosis similar to sporadic tumors
Microcystic/reticular schwannoma has predilection for visceral location
Ancillary Tests
Diffuse, strong S100 positivity is characteristic
TERMINOLOGY
Definitions
Encapsulated, benign peripheral nerve sheath tumor composed predominantly of Schwann cells
ETIOLOGY/PATHOGENESIS
Molecular Aberrations
Somatic NF2 gene mutations present in most tumors
Bilateral vestibular schwannomas occur in setting of germline NF2 gene mutations
CLINICAL ISSUES
Epidemiology
Incidence
90% are sporadic
10% are syndromic
About 3% with neurofibromatosis type 2 (NF2)
2% with schwannomatosis
5% with multiple meningiomas
Rarely in association with neurofibromatosis type 1 (NF1)
Age
All ages
Common between 20-50 years of age
Gender
Affects males and females equally
Site
Head & neck
Upper and lower extremities
Deep-seated tumors occur in mediastinum and retroperitoneum
Presentation
Slow growing
Painless mass
Large tumors may be painful
Cystic tumors may show fluctuation in size
Treatment
Surgical excision is curative
Prognosis
Excellent
Multiple Schwannoma Syndromes
Neurofibromatosis type 2
Autosomal dominant condition
Incidence around 1:30,000-40,000
Inactivating germline mutations of NF2 gene on chromosome 22
Bilateral vestibular schwannomas are characteristic
Schwannomas involving other cranial nerves may be present
CNS tumors like meningioma, ependymoma, and gliomas are also part of disease spectrum
Schwannomas in NF2 resemble their sporadic counterparts
Schwannomatosis
Not associated with germline mutations in NF1 or NF2 genes
Autosomal dominant inheritance with incomplete penetrance
Both sexes affected equally
Patients do not develop bilateral vestibular schwannomas or CNS tumors seen in NF2
Locus of disease mapped to chromosome 22 proximal to NF2 gene
Morphology similar to sporadic schwannomas
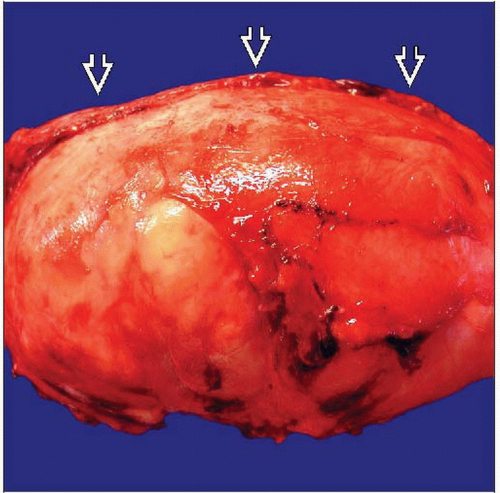
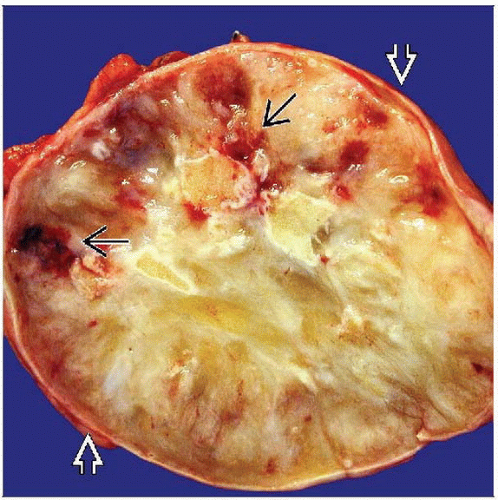
MACROSCOPIC FEATURES
General Features
Surrounded by true capsule consisting of epineurium
Eccentric mass loosely attached to underlying nerve
Small tumors may be fusiform in shape and mimic neurofibroma
Dumbbell-shaped tumors occur in vertebral canal usually in posterior mediastinum
Cut surface is pink, white-yellow
Large tumors may show cystic change, hemorrhage, or calcification
Size
Variable
MICROSCOPIC PATHOLOGY
Histologic Features
Uninodular mass with fibrous capsule
Hallmark: Variable amounts of hypercellular Antoni A and hypocellular Antoni B areas
Antoni A
Spindle cells in short fascicles
Plump nuclei, indistinct cytoplasmic borders
Intranuclear vacuoles in some tumors
Nuclear palisading or whorling
Verocay bodies
Compact rows of palisaded nuclei separated by fibrillary processes
Antoni B
Spindle or oval cells
Loose matrix with cystic change and inflammatory cells
Large vessels with thick hyalinized walls and luminal thrombi
Benign epithelial structures and glands may be present in rare instances
Cytologic Features
Bland nuclear features in most instances
Variants
“Ancient” schwannoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree