Patient Story
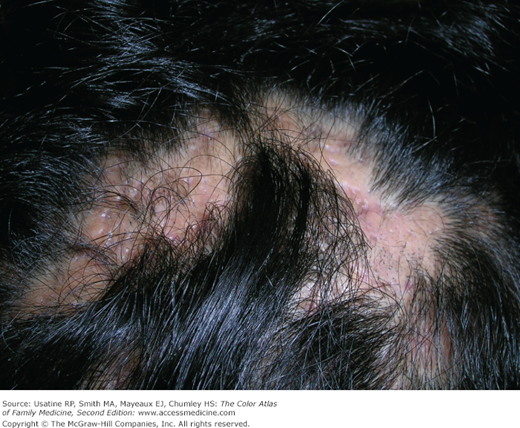
A 32-year-old man presents with hair loss along with chronic pustular eruptions of his scalp. Previous biopsy has shown folliculitis decalvans. He has had many courses of antibiotics, but the hair loss continues to progress. The active pustular lesions are cultured and grow out methicillin-resistant Staphylococcus aureus. The patient is treated with trimethoprim-sulfamethoxazole twice daily and mupirocin to the nasal mucosa, twice daily for 5 days. Two weeks later, the pustular lesions are less prominent although the alopecia is permanent (Figures 189-1 and 189-2).
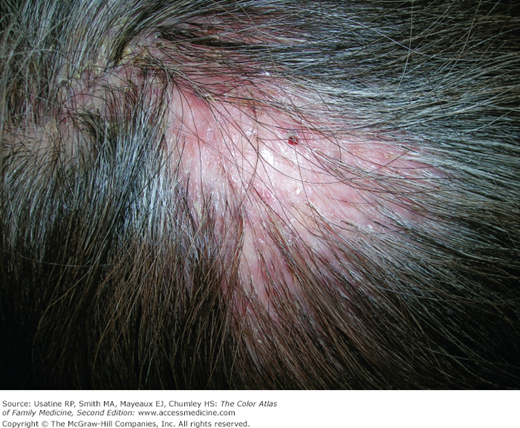
Figure 189-2
Same patient (Figure 189-1) showing permanent hair loss on the top of the head with some small active pustular lesions. (Courtesy of Richard P. Usatine, MD.)
Introduction
Epidemiology
The annual incidence rate of lichen planopilaris (LPP) in 4 hair loss centers in the United States varied from 1.15% to 7.59% as defined by new biopsy-proven LPP—all new patients with hair loss seen over a 1-year period.1
Pathophysiology
Scarring alopecia occurs when there is inflammation and destruction of the hair follicles leading to fibrous tissue formation.2
Hair loss in scarring alopecia is irreversible because the inflammatory infiltrate results in destruction of the hair follicle stem cells and the sebaceous glands.3
The inflammatory infiltrates are either predominantly lymphocytic, neutrophilic, or mixed. These differences are used to classify the scarring alopecias. See Table 189-1.
Lymphocytic | Lichen planopilaris (LPP) Frontal fibrosing alopecia (FFA) Central centrifugal cicatricial alopecia (CCCA) Discoid lupus erythematosus (DLE)* |
Neutrophilic | Folliculitis decalvans Tufted folliculitis |
Mixed | Dissecting cellulitis* Acne keloidalis nuchae* |
End-stage | Nonspecific |
Diagnosis
Scarring alopecias can vary by distribution and appearance. Most patients will need a biopsy to confirm the clinical impression and determine the specific type of alopecia.
The “pull test” is used to see how active the hair loss is in general and in specific areas of the scalp. Always ask the patient if you can pull on the hair as part of your diagnosis.
- With the thumb and forefinger grasp approximately 30 to 40 hairs close to the scalp.
- Gently, but firmly, slide the fingers away from the scalp at a 90-degree angle along the entire length of the hair swatch. Do not tug or jerk.
Interpreting the pull test results:
- Negative pull test = 1 to 4 telogen hairs (small bulbs at bottom).
- Positive pull test = 5 or more hairs (including anagen hairs that have longer follicle sheath at the bottom of the hair).5
Forms of primary cicatricial alopecia include:
- LPP most commonly affects middle-age women. It mostly occurs on the frontal and parietal scalp and causes follicular hyperkeratosis, pruritus, perifollicular erythema, violaceous color of scalp, and scalp pain (Figure 189-3).2 It may also affect other hair-bearing sites such as the groin and axilla.2 Most patients with LPP do not have lichen planus even though the names are very similar.
- Central centrifugal scarring alopecia (CCCA) is a slowly progressive alopecia that begins in the vertex and advances to surrounding areas. It may be related to chemicals used on the hair, heat from hot combs, or chronic tension on the hair.2 It is seen more commonly in African American women (Figure 189-4).
- Frontal fibrosing alopecia (FFA) presents with a progressive recession of the frontal hairline affecting particularly postmenopausal women. It is considered to be a variant of LPP on the basis of its clinical, histologic, and immunohistochemical features (Figure 189-5).6
- Folliculitis decalvans is a chronic painful neutrophilic bacterial folliculitis characterized by bogginess or induration of the scalp with pustules, erosions, crusts, and scale.2 It is postulated that this results from an abnormal host response to S. aureus, which is often cultured from the lesions (Figures 189-1 and 189-2). In one case series, the disease ran a protracted course with temporary improvement while on antibiotic and flare-up of disease when antibiotics were stopped.7
- Tufted folliculitis can be considered to be a milder version of folliculitis decalvans with less surface area of the scalp involved and a better prognosis (Figure 189-6). However, these hair tufts can be seen in other types of scarring alopecias.