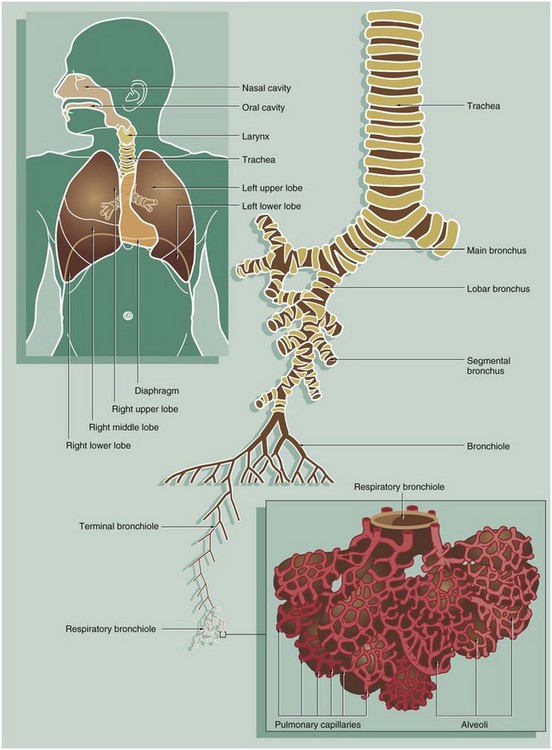
12 Respiration is a term used to describe two different but interrelated processes: cellular respiration and mechanical respiration. Cellular respiration is the series of intracellular biochemical processes by which the cell produces energy by metabolism of organic molecules (see Ch. 1). This chapter is concerned with mechanical respiration, which involves the following steps: • Air is drawn into the body (to the lungs) from the atmosphere by inhalation. • Before it reaches the furthest parts of the lungs, the air is cleaned by removal of particulate matter, warmed so that its temperature equals that of the body and is also moistened. • In the lung parenchyma, oxygen is extracted from the air and transferred into the blood vascular system where it bonds tightly with haemoglobin in the red cells for transport in the systemic arterial circulation. • At the same time that oxygen is passing from air into the blood, carbon dioxide (a by-product of cellular metabolic activity) is transferred from the blood to the air. • After gaseous exchange, the air is returned to the atmosphere by exhalation. The respiratory tract also contains two further elements with separate functions: • The roof of the nasal cavity contains areas of highly specialised mucosa, the olfactory mucosa, responsible for the detection of smell and the more complex aspects of taste (see Fig. 21.2). • The larynx is a specialised structure located at the upper end of the trachea. This utilises forcibly expired air from the respiratory tract below it to generate sound by vibrating the true vocal cords. FIG. 12.2 Nasal cavity, kitten FIG. 12.3 Nasal mucosa FIG. 12.4 Nasopharynx FIG. 12.5 Larynx FIG. 12.6 Trachea FIG. 12.7 Trachea • Tall pseudostratified columnar cells with cilia • Serous cells identical to the cells of the submucosal serous glands • Basal cells which are part of the diffuse neuroendocrine system • Basal stem cells which are able to divide and differentiate to replace other cell types The various cell types are present in different proportions in different parts of the trachea. Ciliated columnar cells are more plentiful in the lower trachea whilst goblet and basal cells are more common in the upper trachea. Beneath the basement membrane, the lamina propria LP consists of loose, highly vascular supporting tissue which becomes more condensed at its deeper aspect to form a band of fibroelastic tissue. FIG. 12.8 Primary bronchus • The respiratory epithelium RE is less tall and contains fewer goblet cells. • The upper lamina propria LP contains more elastin. • The submucosa contains fewer seromucinous glands G. • The cartilage support C is in flattened interconnected plates rather than distinct rings.
Respiratory system
Introduction
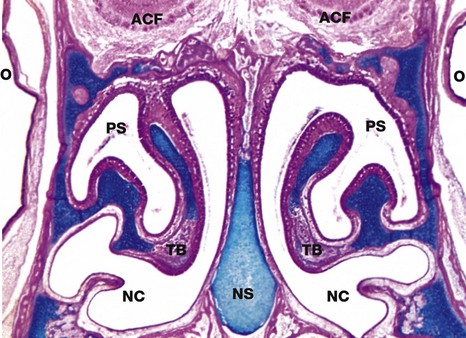
Coronal slice, H&E/Alcian blue (LP)
The nose is subdivided into two nasal cavities NC by the nasal septum NS. The cartilage stains blue using this method.
The nasal cavities and paranasal sinuses PS are lined by respiratory mucosa, the major function of which is to adjust the temperature and humidity of inspired air. Particulate matter entering the nares is usually trapped by the hairs at that site, but some smaller particles are caught on the respiratory mucosa. These functions are enhanced by a large surface area provided by the turbinate bones TB which project into the nasal cavities.
Part of the nasal mucosa, the olfactory mucosa, contains receptors for the sense of smell (see Fig. 21.2). Olfactory mucosa is extensive in lower mammals, but in man it is confined to a small area in the roof of the nasal cavity. Note the close proximity of the nasal cavities to the orbital cavities O and the anterior cranial fossa ACF.
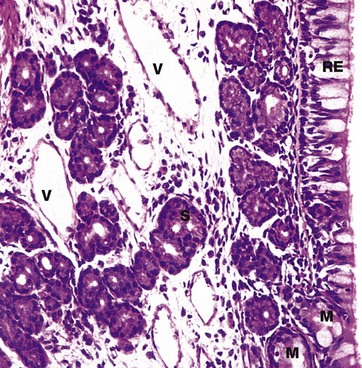
H&E (HP)
The mucosa of the nasal cavities (and paranasal sinuses) consists of a pseudostratified ciliated columnar epithelium RE containing numerous mucin-secreting goblet cells. This is called respiratory epithelium and is found elsewhere in the conducting part of the respiratory tract. The respiratory epithelium has an unusually thick basement membrane (not seen at this magnification).
It is supported by a lamina propria rich in blood vessels V and serous S and mucous M glands. The secretions of these glands and epithelial goblet cells trap small particles in the inspired air in a thin layer of surface mucous. This mucous layer is propelled towards the pharynx by the coordinated movement of the cilia. This is sometimes described as the muco-ciliary escalator. From the pharynx, most of the mucus is swallowed and gastric acid destroys any trapped bacteria.
The temperature of the inspired air is adjusted close to that of the body as a result of warming by the rich plexus of blood vessels (mainly thin-walled vessels). The air is also humidified by contact with the gland secretions, particularly those of the serous glands.
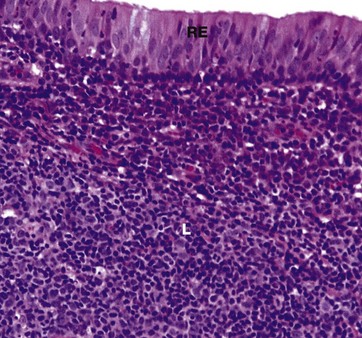
H&E (HP)
The nasopharynx is lined by pseudostratified ciliated columnar (respiratory) epithelium RE similar to that seen in Fig. 12.3, but patches of squamous epithelium occur with increasing age, particularly near the lower end and most extensively in smokers.
The lamina propria contains some serous and mucous glands, but the dominant feature of the mucosa at this site is the presence of large masses of lymphoid tissue L which forms a component of Waldeyer ring of lymphoid tissue, protecting the entry portals of the respiratory and gastrointestinal systems.
This lymphoid tissue is particularly prominent in children and young adults and usually bulges outwards into the lumen of the nasopharynx, producing an appearance similar to that seen in the lingual tonsil (see Fig. 13.13) with epithelial crypts. This is called the nasopharyngeal tonsil or adenoid.
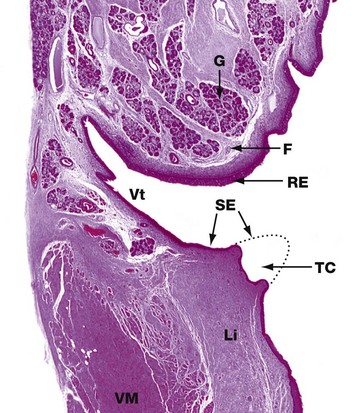
H&E (LP)
This low-power photomicrograph shows the constituents of one half of the larynx. It comprises two folds which protrude into the airway. The upper fold is the false vocal cord F which is covered by columnar ciliated respiratory-type epithelium RE and contains seromucous glands G.
The lower fold is the true vocal cord TC. In this surgically removed human larynx, the sharp tip of the true cord has been removed by diathermy in the distant past and a dotted line shows its normal outline. The true cord contains the vocalis muscle VM and vocalis ligament Li which are responsible for moving the true cord so that it moves towards or away from the true cord on the other side, thus controlling the pitch of the sound made. The true cords are covered by stratified squamous epithelium SE which is more resistant to the effects of physical trauma caused by the free margins of the true cords contacting each other during speech.
Between the true and false cords, there is a narrow cleft, the ventricle Vt, which terminates in a blind-ending saccule (not shown). The ventricle and saccule are lined by respiratory-type columnar epithelium and also contain seromucous glands.
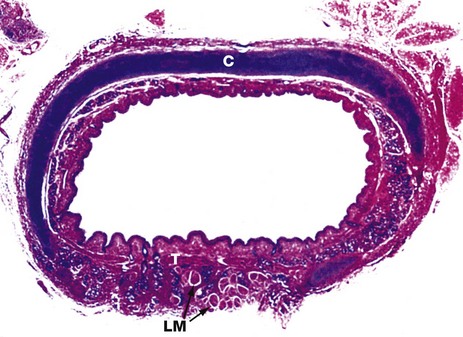
H&E/Alcian blue (LP)
This specimen from a newborn child shows the general structure of the trachea. This is a flexible tube of fibroelastic tissue and cartilage which permits expansion in diameter and extension in length during inspiration, and passive recoil during expiration. A series of C-shaped rings of hyaline cartilage C (stained blue) support the tracheal mucosa and prevent its collapse during inspiration.
Bands of smooth muscle called the trachealis muscle T join the free ends of the rings posteriorly. Contraction of the trachealis reduces tracheal diameter and thereby assists in raising intrathoracic pressure during coughing. A few strands of longitudinal muscle LM can be seen disposed behind the trachealis muscle.
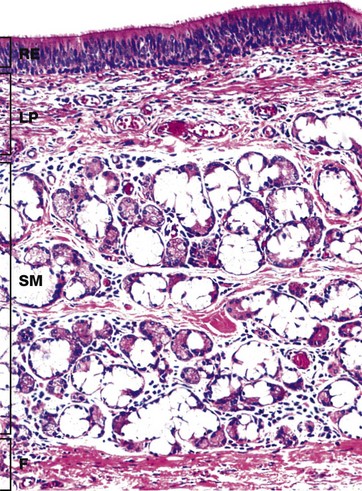
H&E (MP)
The inner layers of the tracheal wall are shown in this specimen from a young adult. The respiratory epithelium RE of the trachea is similar to the rest of the bronchial tree and nasal epithelium. A variety of cell types is found in the epithelium, including:
Underlying the lamina propria is the loose submucosa SM containing numerous mixed seromucinous glands which decrease in number in the lower trachea. The serous cells stain strongly and the mucous cells poorly with H&E. The submucosa merges with the perichondrium of the underlying hyaline cartilage rings (not seen here) or, as here, with the dense fibroelastic tissue F between the cartilage rings.
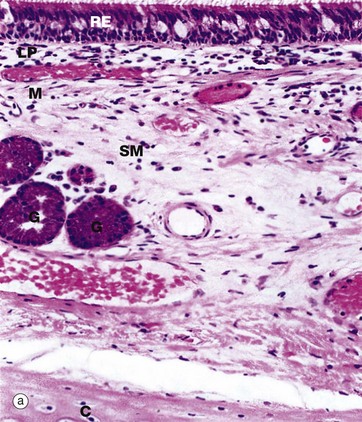
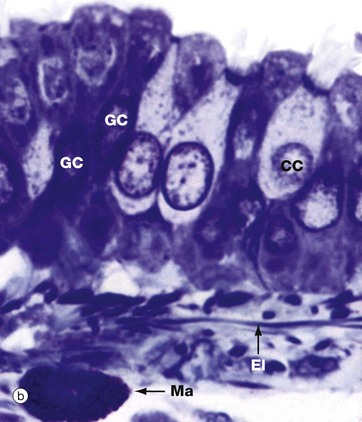
(a) H&E (MP) (b) Thin resin section, toluidine blue (HP)
The basic structure of the wall of a main bronchus (a) is similar to that of the trachea but differs in several details:
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Respiratory system