1. The mainstay of therapy for bronchospasm, wheezing, and airflow obstruction is β-adrenergic agonists (typically delivered via inhalers or nebulizers).
2. Short-acting β2 agonists such as albuterol, levalbuterol, metaproterenol, and pirbuterol are prescribed for the rapid relief (rescue therapy) of wheezing, bronchospasm, and airflow obstruction. Clinical effect is seen in a matter of minutes and lasts up to 4 to 6 hours.
3. Long-acting β2 agonists are prescribed for control of symptoms when rescue therapies are used more than two times per week.
4. Systemic absorption of inhaled β2 agonists is responsible for a myriad of side effects (tremors, tachycardia), most of which are not serious. Hyperglycemia, hypokalemia, and hypomagnesemia also can occur with β2-agonist therapy but the severity of these side effects tends to diminish with regular use.
5. Tolerance to β2 agonists can occur with regular use over a period of weeks and, while not affecting peak bronchodilation, can be evidenced by a decrease in the duration of bronchodilation and the magnitude of side effects.
C. Systemic Adrenergic Agonists. Oral, intravenous (IV), or subcutaneous administration of β-specific or nonspecific adrenergic agonists is now reserved for rescue therapy.
1. Terbutaline can be given orally, subcutaneously, or intravenously; albuterol (salbutamol) can be given intravenously; and epinephrine is usually given subcutaneously or intravenously. Regardless of the route of administration, all three will produce bronchodilation.
2. The side effect profile of systemic adrenergic agonists is similar to the side effect profile for inhalational adrenergic agonists (tremor, tachycardia).
D. Inhaled Cholinergic Antagonists (see Table 25-1)
1. The use of inhaled anticholinergics in chronic obstructive pulmonary disease (COPD) as maintenance and rescue therapy is considered standard treatment.
2. Anticholinergics are not used for maintenance therapy in asthma and are only recommended for use in acute exacerbations.
3. Ipratropium is classified as a short-acting anticholinergic and is commonly used as maintenance therapy for COPD and as rescue therapy for both COPD and asthmatic exacerbations. It is not indicated for the routine management of asthma.
4. Tiotropium is the only long-acting anticholinergic available for COPD maintenance therapy.
5. Inhaled anticholinergics are poorly absorbed and therefore serious side effects are uncommon (dry mouth, urinary retention, pupillary dilation, blurred vision).
E. Systemic Cholinergic Antagonists
1. The systemically administered anticholinergics atropine and glycopyrrolate act via the same mechanisms as inhaled anticholinergics, but their use is generally limited by side effects.
2. Atropine, because of its tertiary ammonium structure, has a tendency to cause tachycardia, gastrointestinal upset, blurred vision, dry mouth, and central nervous system effects secondary to its ability to cross the blood–brain barrier.
3. Glycopyrrolate has a quaternary ammonium structure and is insoluble in lipids, similar to ipratropium and tiotropium, and has fewer systemic side effects than atropine.
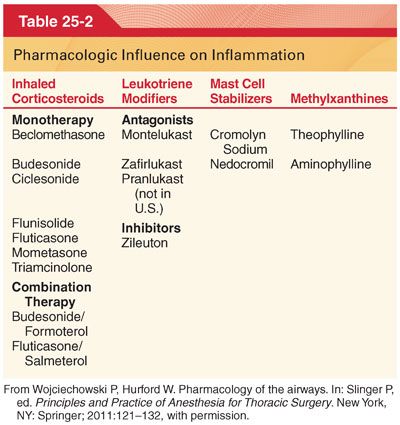
II. Influence of Inflammation on the Airway. Asthma and COPD, the most common obstructive airway diseases, have a component of inflammation as part of their pathogenesis. Patients presenting to the operating room with obstructive airway diseases have a high likelihood of taking antiinflammatory therapies for control of their disease (Table 25-2).
A. Inhaled Corticosteroids
1. Inhaled corticosteroids (ICS) reduce the inflammatory changes associated with asthma, thereby improving lung function and reducing exacerbations, whereas the use of ICS as monotherapy in COPD is discouraged.
2. In COPD, ICS are used as a part of combination therapy along with long-acting β-adrenergic agonists (LABA).
3. Side effects with the use of ICS in asthma and COPD include an increase in pneumonia but not deaths, oropharyngeal candidiasis, pharyngitis, osteoporosis, dysphonia, and cough.
B. Systemic Corticosteroids
1. Systemic corticosteroids given in IV or oral form are used for treatment of asthma and COPD exacerbations.
2. Patients who are hospitalized with a COPD exacerbation will typically receive IV corticosteroids to suppress any inflammatory component that may be contributing.
3. In asthma, corticosteroids are recommended for exacerbations that are either severe, with a peak expiratory flow of less than 40% of baseline, or a mild to moderate exacerbation with no immediate response to short-acting β-adrenergic agonists.
4. The recommended duration of therapy is 3 to 10 days without tapering (some patients with difficult to manage asthma and COPD will be receiving long-term oral corticosteroid therapy).
C. Leukotriene modifiers for the treatment of asthma are usually prescribed for long-term control in addition to short-acting β-adrenergic agonists or in conjunction with ICS and short-acting β agonists.
D. Mast Cell Stabilizers. Cromolyn sodium and nedocromil are used in the treatment of asthma (delivered by powder inhaler and are not first-line therapy).
E. Methylxanthines. Currently, theophylline is recommended only as an alternative therapy and is not a first-line choice for asthma or COPD (significant side effect profile and the need for monitoring of blood level).
III. Influence of Anesthetics on the Airways
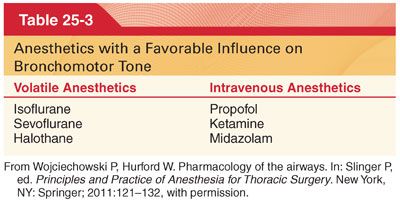
A. Volatile Anesthetics (Table 25-3). Volatile anesthetics reduce bronchomotor tone and all commonly used volatile anesthetics, except desflurane, produce a degree of bronchodilatation (may be helpful in patients with obstructive lung disease or in patients that experience any degree of bronchoconstriction).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


