Chapter Eighteen. Respiration
Anatomy of the respiratory system
The respiratory system consists of the airways from the nasal passages to the pharynx and larynx as well as the bronchi, bronchioles and alveoli of the lungs (Fig. 18.1). The chest structures necessary for moving air in and out of the lungs are part of the system. It is usual to divide the respiratory system into the upper and lower airways at the level of the cricoid cartilage.
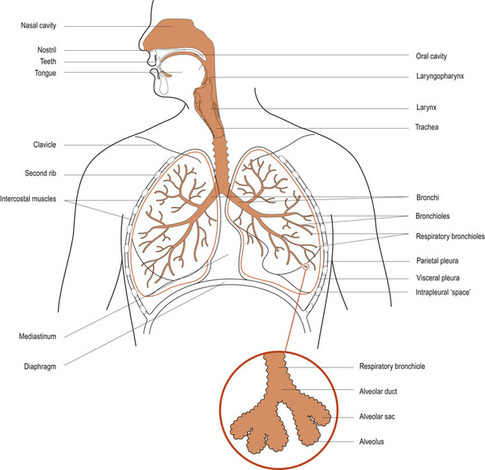 |
| Figure 18.1 Organisation of the respiratory system. (From Hinchliff S M, Montague S E 1990, with permission.) |
The upper airways
The nasal cavity is a large, irregular-shaped cavity divided into two by a septum. Bony structures, called the turbinates, increase the surface area of the cavity and it is lined with ciliated epithelium which warms, filters and moistens the incoming air. The air now enters the upper pharynx through two internal nares.
The pharynx is a common passageway for water and food as well as air. It is a funnel-shaped tube extending from the internal nares to the level of the cricoid cartilage. The auditory or Eustachian tubes open into the upper pharynx and the mouth opens into the central portion or oropharynx. The tonsils and adenoids, which are organs of the lymphatic system, are found in the larynx. The oropharynx divides into the oesophagus, transporting food and water into the stomach, and the trachea, transporting air into the lungs.
The larynx, commonly called the voice box, is composed of pieces of cartilage connected by ligaments and moved by muscles. It is lined with mucous membrane continuous with the pharynx and trachea. In the larynx are the vocal cords, responsible for the production of sound, and between the vocal cords is the glottis, through which air passes. The epiglottis is a leaf-shaped piece of cartilage anchored to the thyroid cartilage. It moves up and down during swallowing to act as a cover for the glottis and prevent food and water from being inhaled into the larynx and lungs.
The lower respiratory tract
The lower part of the airway is also called the bronchial tree because of its resemblance to a trunk and branches (Fig. 18.2). The trachea is a cylindrical tube, 10–12 cm long, made up of 16–20 C-shaped cartilaginous rings joined together by fibrous and muscular tissue. This gives the trachea a firm structure to prevent collapse of the airway during inspiration. The posterior aspect of the cartilaginous rings is absent, facilitating the passage of food down the oesophagus, which lies immediately behind the trachea. The trachea extends from the larynx to the level of the fifth vertebra, where it divides into the two primary bronchi. The right primary bronchus is wider and shorter and more vertical than the left so that inhaled objects tend to enter the right lung rather than the left. The primary bronchi enter the lungs at the hilum, where the right bronchus goes on to divide into three: the right upper, middle and lower bronchi, to serve three lobes of the right lung. The left primary bronchus divides into two: the left upper and lower bronchi, to serve the two lobes of the left lung.
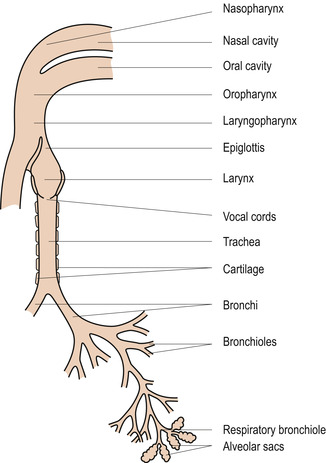 |
| Figure 18.2 Organisation of the airways. (From Hinchliff S M, Montague S E 1990, with permission.) |
The lower branches of the airway, known as bronchi, still have cartilage in their structure. After this they are known as bronchioles and have smooth muscle in their walls. The smooth muscle is able to respond to stimuli by causing dilatation or constriction of the lumen of the bronchioles. This function is mainly under the control of the autonomic nervous system, with sympathetic impulses causing bronchodilation and parasympathetic impulses causing bronchoconstriction. There are about 8–13 divisions from the trachea to the smallest bronchi and another 3–4 before the terminal bronchioles are reached. Each terminal bronchiole divides into about 50 respiratory bronchioles. About 200 sac-like alveoli are supplied with air by each respiratory bronchiole. Alveoli do not form part of the conducting zone of the respiratory system.
The thoracic cage
The thoracic cage forms the cavity and contains the two conical lungs and the heart. The organs are separated from each other by the mediastinum and its contents. Each lung is surrounded by a double-layered fluid-filled sac called the pleura, which also attaches them to the inner surface of the thorax. The inner, or visceral, pleura covers the outer surface of the lung and is reflected back to become the outer or parietal pleura which is attached to the inner surface of the thoracic cavity.
Physiology of the respiratory tract
The epithelial lining
The upper airway protects the alveolar tissues by warming, filtering and moistening the air. The structure of the epithelial lining is particularly good as a filter. It contains glands that secrete thick sticky mucus to trap particles and is ciliated to waft excess mucus and foreign particles towards the pharynx where they can be swallowed. The cilia beat about 600–1000 times per minute. Large numbers of phagocytic cells will engulf and destroy debris and bacteria trapped by the mucus.
Reflex mechanisms
Coughing is a forceful expiration reflex under the control of the respiratory centre in the medulla, which will expel irritant particles from the larynx. Air rushes out at a speed of 500 miles per hour! It is instigated by messages from a sensitive part of the airway at the bifurcation of the trachea, called the carina. Sneezing is a similar reflex, instigated by irritation of the nasal mucosa. The swallowing reflex is extremely important for respiration. Absence of this reflex, as is seen in uncon-scious or anaesthetised patients, may result in inhalation of particles of food or water into the larynx or lung. The airway may be obstructed or infection and pneumonia may occur.
Structure and function of the alveoli
The terminal bronchioles feed into respiratory bronchioles which branch into the alveolar ducts. These lead into alveolar sacs and the alveoli, where most of the gas exchange occurs (Fig. 18.3). The alveoli are expansions off the alveolar sacs, making the latter resemble bunches of grapes. Alveoli open into a common chamber called the atrium at the terminus of the alveolar duct. There are about 300 million alveoli in the lungs, providing an enormous area for gas exchange.
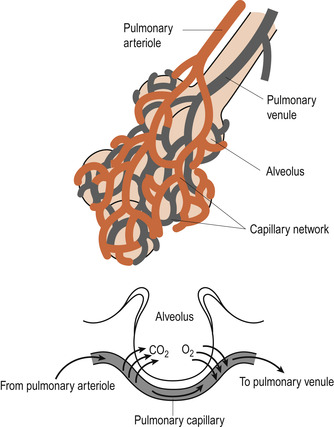 |
| Figure 18.3 Relationship between alveoli and blood vessels. Gas exchange can occur across the vast surface area provided by the dense network of capillaries. (From Hinchliff S M, Montague S E 1990, with permission.) |
The alveolar wall (Fig. 18.4) consists of a single layer of flattened squamous epithelial cells called type I cells. The external surface of an alveolus has a few elastic fibres around the opening. There is a dense network of pulmonary capillaries surrounding each alveolus, providing a continuous encircling sheet of blood. Each capillary wall is also only one cell thick so that the interstitial space between the alveolus and its capillary network, forming the air–blood interface, is extremely thin (0.2 μm, compared with the 7 μm diameter of an average red blood cell). This interface is called the respiratory membrane and has blood flowing on one side and gas on the other. Gas exchange occurs by simple diffusion across the respiratory membrane and depends on the existence of pressure gradients between the lungs and the atmosphere. The total surface area of alveoli in contact with capillaries is roughly the size of a tennis court. This extensive area and the thinness of the barrier permit the rapid exchange of large quantities of oxygen and carbon dioxide for diffusion.
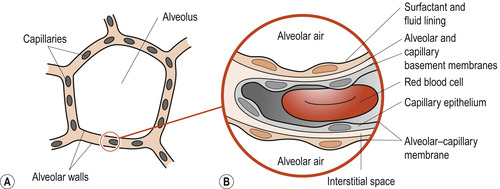 |
| Figure 18.4 (A) Cross-section through an alveolus. (B) Higher magnification showing histology of part of the alveolar–capillary membrane. The dense network of capillaries forms an almost continuous sheet of blood in the alveolar walls, providing a very efficient arrangement for gas exchange. (From Hinchliff S M, Montague S E 1990, with permission.) |
Surfactant
In addition to the type I cells forming the alveolar wall, the alveolar epithelium contains cuboidal type II alveolar cells which secrete pulmonary surfactant. This is a phospholipid that helps to keep the membrane moist and also maintains the patency of the alveolus. Macrophages called dust cells, part of the defence system of the body, are also present in the lumen of the alveoli, mopping up bacteria, dust and other inhaled particles. The alveolar surface is usually sterile. There are minute pores of Kohn present in the alveolar walls, allowing air flow between adjacent alveoli ( collateral ventilation), which is useful if the terminal airways are blocked by disease.
Blood supply to the lungs
The lungs act to oxygenate the blood but they also need their own blood supply to maintain healthy tissue. The blood to be oxygenated reaches the lungs by branches of the pulmonary arteries, is re-oxygenated in the pulmonary capillary network surrounding the alveoli and returns to the heart via the pulmonary veins. The two left and one right bronchial arteries arising from the aorta provide the blood supplying the lung tissue with oxygen. Venous return is by both bronchial veins and the pulmonary veins.
Nerve supply to the respiratory muscles
The phrenic nerve to the diaphragm (originating in cervical nerves 3, 4 and 5) and the intercostal nerves to the intercostal muscles (originating in the thoracic nerves 1–12) innervate the respiratory muscles. This is why severance of the spine above C3 results in total respiratory paralysis but, below that, diaphragmatic breathing can occur although the intercostal muscles will be paralysed.
The physiology of pulmonary ventilation (breathing)
The major function of the respiratory system is to supply the body with oxygen and dispose of carbon dioxide. Four distinct events, collectively called respiration, must occur to perform this function:
1. Pulmonary ventilation—This process is called breathing and includes the movement of air in and out of the lungs.
2. External respiration—This involves the exchange of gases (oxygen loading and carbon dioxide unloading) between the pulmonary blood and alveoli.
3. Respiratory gas transport—Oxygen and carbon dioxide must be transported to and from the lungs and body tissues via the bloodstream.
4. Internal respiration—This involves the process of gas exchange between the blood and the tissue cells in the body.
There are two phases to breathing: inspiration or breathing in and expiration or breathing out. Mechanical factors and neural factors are involved in the control of respiratory rate. Atmospheric air contains about 21% oxygen and 79% nitrogen with traces of inert gases, carbon dioxide and water vapour. Alveolar air exchanges oxygen for carbon dioxide and water vapour. By the time alveolar air reaches the point of expiration it will be mixed with the atmospheric air in the dead space so that the content of expired air will be between the two extremes of atmospheric and alveolar air.
Mechanical factors
Under normal conditions and pressure gradients, oxygen passes from the alveolus into the blood and carbon dioxide from the blood into the alveolus. The movement of gases flowing from a high to a lower pressure down a gradient is said to occur by bulk flow. Air flows in and out of the lungs during breathing by bulk flow. Expansion of the thoracic cage, by contraction of the respiratory muscles during inspiration, increases lung volume and causes a temporary drop in the pressure in the alveoli. Atmospheric air flows in until pressure inside the lung is equal to the atmospheric pressure. Relaxation of the respiratory muscles causes expiration, by reducing the volume of the thoracic cage, creating a temporary rise in pressure within the lung to above atmospheric pressure.
Inspiration
The diaphragm, the most important muscle of inspiration, is a strong dome-shaped sheet of muscle separating the thoracic and abdominal cavities from each other. The diaphragm flattens when it contracts. This change in shape presses down the abdominal contents and lifts the rib cage, enlarging the thoracic cavity both from top to bottom and from front to back. Normally the external intercostal muscles, which are accessory muscles of respiration lying between the ribs, play little part in this expansion of the rib cage but do help to stabilise it. However, during any need for extra oxygen, such as in exercise and in upper airway obstruction, the upper intercostal muscles as well as other accessory muscles of respiration help to enlarge the rib cage and so enhance lung expansion.
Expiration
Under resting conditions, expiration is a passive process brought about by the relaxation and elastic recoil of the diaphragm and intercostal muscles at the end of inspiration. The elastic lung returns to its original volume as air is pushed out of the lung (the functional residual capacity), because the reduction in volume makes the alveolar pressure temporarily exceed atmospheric pressure. Active expiration may occur when the need for gas exchange increases under certain conditions such as during exercise or constriction of the airways.
Pulmonary ventilation
Respiratory parameters
Respiratory volumes and respiratory capacities can be described and measured using a spirograph. The measurements below are given for the average healthy adult (Marieb & Hoehn 2008).
Respiratory volumes
• Tidal volume (TV) is the volume of air entering and leaving the lungs during a single breath. The tidal volume during normal quiet breathing averages 500 ml for both males and females.
• Inspiratory reserve volume (IRV) is the maximum amount of air that can be increased above the tidal volume value during the deepest inspiration. Volumes differ significantly by gender: males average 3200 ml and females average 1900 ml.
• Expiratory reserve volume




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


