pT0: No evidence of primary tumor
pTa: Noninvasive papillary carcinoma
pTis: Carcinoma in situ
pT1: Tumor invades subepithelial connective tissue ( lamina propria)
pT2:Tumor invades muscularis propria
pT2a: Inner half
pT2b: Outer half
pT3: Tumor invades perivesical tissue
pT3a: Microscopically
pT3b: Macroscopically
pT4: Tumor invades any of the following: prostate (does NOT include invasion from the prostatic urethra), uterus, vagina, pelvic wall, abdominal wall
Reporting Stage in Transurethral Resection of Bladder Tumor (TURBT) Specimens
Invasive Carcinomas
In transurethral resection of bladder tumor (TURBT) specimens, the reporting of invasive urothelial carcinomas is critical to subsequent clinical management. It is recommended that bladder biopsy staging evaluation be restricted to pT1 and pT2 disease; pT3 and pT4 disease can only be diagnosed at cystectomy. Adipose tissue is commonly present within the muscularis propria and may even be seen in the lamina propria ; therefore, the presence of tumor within adipose tissue does not signify a pT3 tumor. At biopsy evaluation, the most important histologic distinction for invasive urothelial carcinoma is lamina propria invasion versus muscularis propria invasion (i.e., pT1 vs. pT2 disease). Urologists typically favor conservative management with intravesical treatment regimens for high-grade pTa and any pT1 disease. The diagnosis of pT2 carcinoma is generally the threshold for surgical management (e.g., radical cystectomy) and/or radiation therapy. The histologic parameters included in the pathology report should allow the urologist to easily assign a T stage to the patient, and to select the appropriate treatment plan.
Studies suggest that stage is the most important prognostic factor in invasive urothelial carcinoma, independent of grade [3]. This is supported by additional studies documenting the capability of deeply invasive, cytologically bland carcinomas to produce metastases and cause patient mortality [4–6]. In our opinion, invasive urothelial carcinomas are biologically high grade.
Some authors have suggested the utility of substaging lamina propria invasion based on depth measurements or relation to the muscularis mucosae (see Chap. 12). This substaging is difficult in practice because bladder biopsies are frequently sectioned in a tangential plane making orientation difficult to assess. Because of these difficulties and lack of an accepted reproducible method, substaging has not been adopted under the current systems of staging and classification (WHO 2004; 7th edition AJCC).
A simple diagnostic template is shown in Table 14.2 that includes the relevant diagnostic findings needed for patient management. We avoid the use of the term “muscle invasion” because it does not distinguish between carcinomas invading muscularis propria (detrusor muscle) (pT2) from those invading only muscularis mucosae (pT1). It is best to use the more specific anatomic terms “lamina propria” (Fig. 14.1a, b) or “muscularis propria” (Fig. 14.2) to describe depth of invasion. Including the pT stage in the line diagnosis can also help to avoid any misunderstanding with regard to anatomic terms. In a subset of cases, it may be difficult to definitively classify a carcinoma as pT1 or pT2 if fragments of smooth muscle are involved in which the distinction of muscularis propria from muscularis mucosae is problematic. In those cases, we use a diagnostic term such as “invasive urothelial carcinoma, indeterminate depth (see comment regarding stage)” with an appropriate comment section.
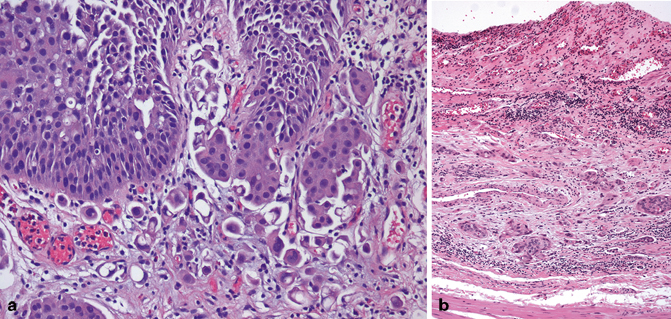
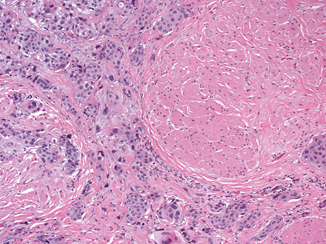
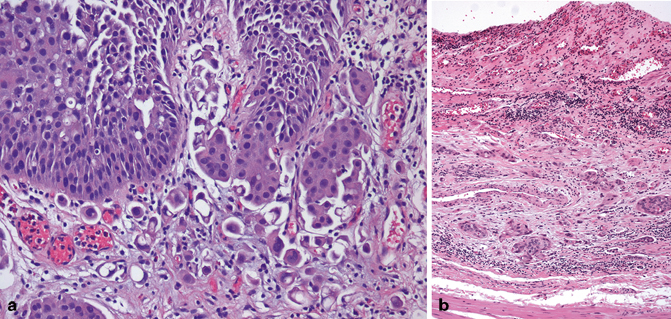
Fig. 14.1
Invasive high-grade urothelial carcinoma with lamina propria invasion (pT1): individual carcinoma cells (a) or nests of urothelial carcinoma (b) are present within the lamina propria. Notice the presence of stromal retraction surrounding some of the nests of invasive carcinoma (b)
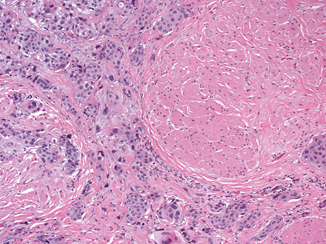
Fig. 14.2




Invasive high-grade urothelial carcinoma with muscularis propria invasion (pT2)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


