1. The Glomerulus
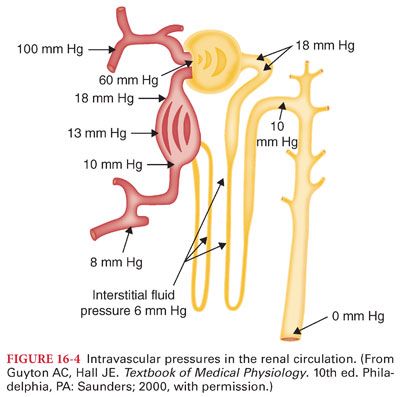
a. Glomeruli are found in the renal cortex and consist of a tuft of capillaries surrounded by Bowman’s capsule, the dilated blind end of the renal tubule. Glomerular capillaries are uniquely interposed between two sets of arterioles. Blood flows from the afferent arterioles through the glomerular capillaries and then on to the efferent arterioles. Glomerular capillary pressure causes water and low-molecular-weight substances to be filtered into Bowman’s capsule and the renal tubule system.
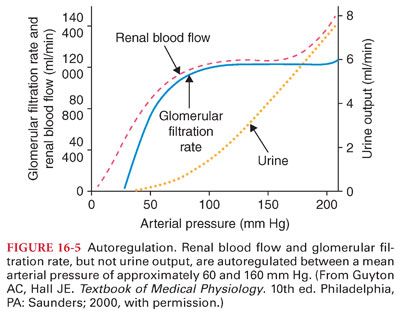
b. Glomerular filtration rate (GFR) is the volume of collective glomerular filtrate formed over time. Because 99% of this 180 L of glomerular filtrate is reabsorbed, daily urine output is 1 to 2 L. The kidneys have an autoregulatory mechanism to modulate the effect of mean arterial pressure on the GFR (a nearly constant filtration pressure leads to a consistent GFR across a range of mean arterial pressure, remaining relatively constant between mean arterial pressures of 60 and 160 mm Hg).
2. The renal tubule (see Fig. 16-1)
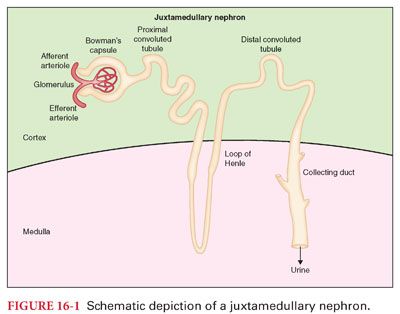
B. Glomerular filtrate is converted into urine along the course of the renal tubule (Table 16-1).
1. The process of reabsorption determines the volume of urine formed, whereas secretion is particularly important in determining the nature of the urine, such as concentration of potassium and hydrogen ions. The most important factors influencing the reabsorption of sodium and water are aldosterone, arginine vasopressin (AVP), renal prostaglandins, and atrial natriuretic factor (ANP).
2. Reabsorption of sodium involves moving this ion against a concentration gradient from the lumen of the proximal tubule into peritubular capillaries (requires energy, supplied by the sodium-potassium adenosine triphosphatase [ATPase] system). The proximal convoluted renal tubules, driving the ATPase enzyme for sodium reabsorption, consume approximately 80% of renal oxygen consumption.
3. More than 99% of the water in the glomerular filtrate is reabsorbed into peritubular capillaries as it passes through renal tubules. The distal tubules are almost completely impermeable to water, allowing for control of the specific gravity of the urine. The permeability of the collecting ducts is variable and determined by the action of AVP. Increased AVP leads to reabsorption of water from the collecting ducts, resulting in highly concentrated urine. Decreased AVP results in little water reabsorption and large amounts of dilute urine.
C. Countercurrent System
1. The ability of the kidneys to produce either dilute or concentrated urine depends on the gradient in osmolarity between the renal cortex and renal medulla that is created by the loop of Henle (Fig. 16-2).
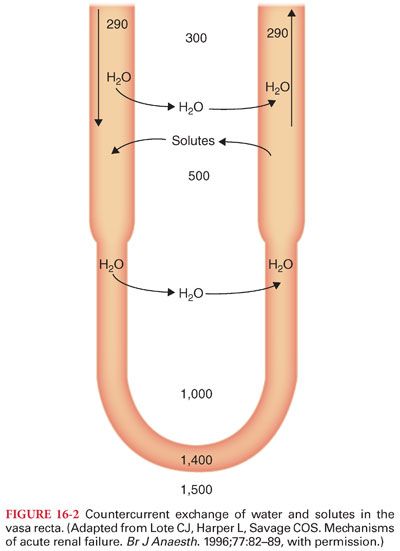
2. The U-shaped arrangement of peritubular capillaries, known as the vasa recta, parallels the loops of Henle. This forms a countercurrent system, in which capillary inflow runs parallel and in an opposite direction to capillary outflow.
D. Aquaporins (tetramer protein structures and are found in the kidneys, brain, salivary and lacrimal glands, and respiratory tract) are channels that facilitate rapid passage of water across lipid cell membranes.
E. Tubular transport maximum (Tm or Tmax) is the maximum amount of a substance that can be actively reabsorbed from the lumens of renal tubules each minute.
1. The Tm for glucose is approximately 220 mg per minute. When the amount of glucose that filters through the glomerular capillary exceeds this amount, the excess glucose cannot be reabsorbed and passes into urine (Fig. 16-3).
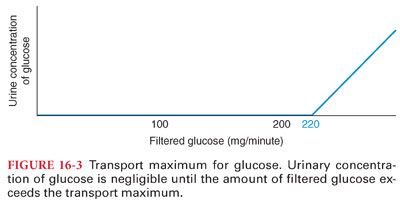
2. The presence of large amounts of unreabsorbed solutes in the urine such as glucose (or mannitol) produces osmotic diuresis by retaining water in the collecting system.
F. Transport of Urine to the Bladder
1. From the collecting ducts, urine travels into the renal pelvis. A ureter arises from the pelvis of each kidney. At its distal end, the ureter penetrates the bladder obliquely such that pressure in the bladder compresses the ureter, thereby preventing reflux of urine into the ureter when bladder pressure increases during micturition.
2. Each ureter is innervated by the sympathetic and parasympathetic nervous system (parasympathetic nervous system stimulation increases the frequency of peristalsis, whereas sympathetic nervous system stimulation decreases peristalsis).
a. Obstruction of a ureter by a stone causes intense reflex constriction and pain.
b. Spinal cord damage above the sacral region leaves the micturition reflex intact but is no longer controlled by the brain.
III. Renal Blood Flow. Although the kidneys represent about 0.5% of total body weight, their blood flow is disproportionately large at 20% to 25% of the cardiac output. The ability to autoregulate keeps renal blood flow relatively constant across a range of systemic mean arterial pressures. Approximately 90% of the renal blood flow is distributed to the renal cortex, with less than 10% of renal blood flow going to the medulla. The generous delivery of blood to the cortex supports flow-dependent functions such as glomerular filtration and tubular reabsorption processes of the cortex. Low blood flow also makes the medulla more susceptible to ischemia than the cortex.
A. Renal Cortex Blood Flow: Glomerular and Peritubular Capillaries (Figs. 16-1 and 16-4)
B. Autoregulation of Renal Blood Flow
1. Renal blood flow and GFR are kept relatively constant within a range of mean arterial pressure between approximately 60 and 160 mm Hg (Fig. 16-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


