Radical Cholecystectomy
Richard J. Bold
DEFINITION
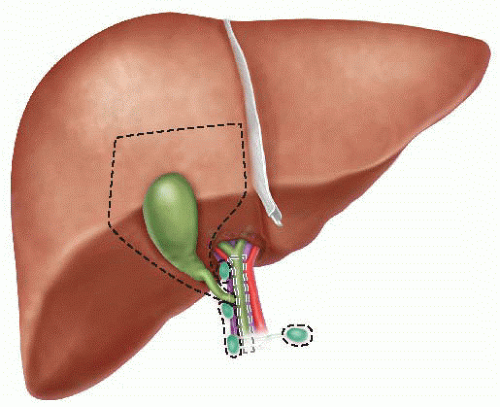
Radical cholecystectomy is defined as the resection of the gallbladder and gallbladder fossa and is usually combined with a supraduodenal lymphadenectomy for the treatment of gallbladder cancer.1 The extent of the hepatic resection may include nonanatomic parenchymal resection of the gallbladder fossa to a standard segment IVb/V resection (FIG 1), with data suggesting superior survival from segment IVb/V resection over standard cholecystectomy.2 The goal of the resection is complete resection of all histopathologic disease, which may necessitate resection of the common hepatic duct/common bile duct if clearance of all disease cannot be obtained by division at the cystic duct/common hepatic duct junction.
DIFFERENTIAL DIAGNOSIS
A variety of other conditions may mimic adenocarcinoma of the gallbladder. These include benign intraluminal polyps (due to the mass appearance on imaging), chronic cholecystitis (due to collapse of the lumen and associated mural thickening due to chronic inflammation), or hepatic masses within the gallbladder fossa (due to presence of a hepatic mass adjacent to the gallbladder).3
PATIENT HISTORY AND PHYSICAL FINDINGS
The majority of early-stage gallbladder cancers are clinically silent and will not be diagnosed preoperatively but instead will be recognized on final pathology following cholecystectomy performed for other conditions, such as symptomatic cholelithiasis or cholecystitis.4,5
Occasionally, polypoid gallbladder cancers will present with right upper quadrant pain similar to cholecystitis, presumably from the intraluminal mass effect or the obstruction of the fundus/cystic duct. In addition, should the tumor extend down the cystic duct to the common hepatic duct, patients may present with painless jaundice.
Symptoms of abdominal bloating and/or weight loss should be concerning for the presence of malignant ascites due to peritoneal metastasis, a common site of spread. The liver is the most other common site of metastasis.
The incidence of gallbladder cancer is three times higher in women than in men.6
Hispanics, American Indians, and Mexican Indians have been identified as high-risk groups for gallbladder cancer.6
Large, multiple gallstones have an increased association with gallbladder cancer; gallstones are present in 60% to 80% of patients with gallbladder cancer.3
Obesity is a risk factor for both gallstones and gallbladder cancer; furthermore, obesity increases the risk for the development of nonalcoholic liver disease, particularly nonalcoholic steatohepatitis (NASH), which may impact the suitability for radical cholecystectomy.7
Radical cholecystectomy involves a partial hepatic resection, and therefore, risk factors for cirrhosis (e.g., alcohol abuse, chronic hepatitis virus infection) are important aspects of the patient’s history and evaluation for tolerability of hepatic resection.8
Early-stage gallbladder cancer is usually not apparent on physical examination. Physical findings suggesting advanced disease include the presence of ascites (peritoneal metastasis); painless jaundice (either direct extension into the common hepatic duct or bulky portal adenopathy causing external biliary dilation); and a nontender, palpable gallbladder (concerning for extensive mural involvement). In addition, physical findings of end-stage liver disease raise the suspicion of underlying cirrhosis and therefore preclude radical cholecystectomy.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Radical cholecystectomy is appropriate only for those patients with T1b, T2, or T3 (primary tumor thickness) or N0 or N1 gallbladder cancer (FIG 2 and Table 1).9, 10, 11, 12, 13, 14
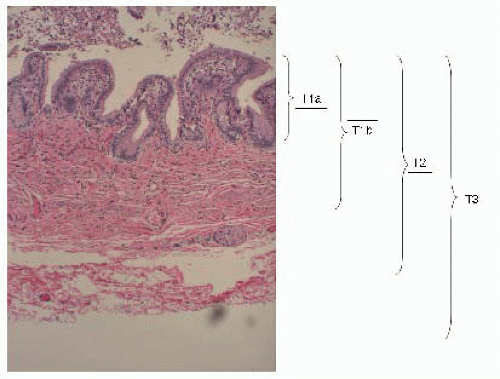
FIG 2 • Histology of the gallbladder wall with corresponding extent of T1a, T1b, T2, and T3 carcinoma of the gallbladder.
Table 1: American Joint Commission on Cancer Staging System for Gallbladder Cancer
Primary Tumor (T)
Histopathologic Characteristic
TX
Primary tumor cannot be assessed
T0
No evidence of primary tumor
Tis
Carcinoma in situ
T1a
Tumor invades lamina propria
T1b
Tumor invades muscle layer
T2
Tumor invades perimuscular connective tissue; no extension beyond serosa or into liver
T3
Tumor perforates serosa and/or directly invades into the liver and/or one other adjacent organ or structure
T4
Tumor invades main portal vein or hepatic artery or involves multiple extrahepatic structures
Regional Lymph Nodes (N)
NX
Regional lymph nodes cannot be assessed
N0
No regional lymph node metastasis
N1
Regional lymph node metastasis
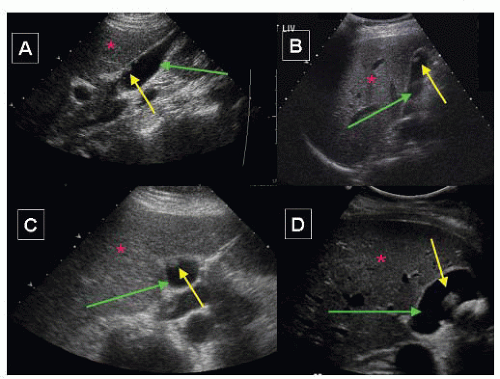
The majority of patients will undergo an initial ultrasound for evaluation of right upper quadrant pain and suspected cholelithiasis. The presence of a gallbladder polyp within the lumen raises the suspicion for gallbladder cancer (FIG 3). Given the intraluminal aspect of any polyp, percutaneous biopsy is not usually feasible in the absence of any invasive features beyond the gallbladder wall.15
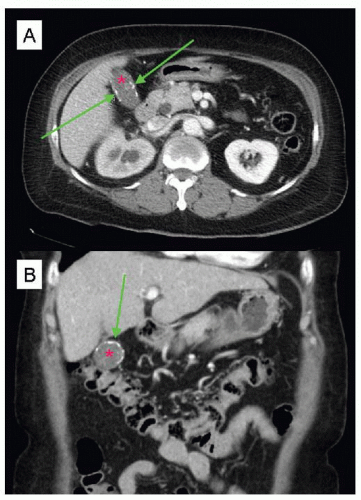
There is only a weak association between patients with a calcified gallbladder (“porcelain gallbladder”) and an underlying gallbladder cancer, such that prophylactic cholecystectomy may no longer be routinely advocated.16 The calcification of the gallbladder wall may not be readily visible on ultrasound but is clearly seen on contrast-enhanced computed tomography (CT) scans (FIG 4). This radiologic finding should prompt concern for gallbladder cancer, even in the absence of any symptoms or associated findings on radiologic imaging.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree