7
Chapter Outline
| Web Toolkit available at www.ashp.org/ambulatorypractice |
Chapter Objectives
1. Describe the rationale for developing a robust ambulatory clinical patient services quality improvement program.
2. Apply key quality principles to the structure of your clinic or service in order to provide quality services.
3. Implement the PDSA method for quality improvement in your practice.
4. List the skills desired for an ambulatory clinical patient-care pharmacist.
Introduction
Over the past 20 years, attention to quality in health care services has escalated due to limited and shrinking resources, fueling a demand for quality at the best value/cost ratio tied to improved patient outcomes. Incorporating measurements of quality into health care work flow and relating them to patient outcomes has proven to be a daunting challenge. As an industry, health care is just beginning to understand how to measure quality, evaluate which measures provide meaningful information, and determine how well the measures reflect optimal patient outcomes. We as ambulatory clinical pharmacists are not immune from the process and will need to understand how to assess the quality of services we provide and embed quality measurement into our daily practices. As ambulatory pharmacists, we are under greater pressure to show quality and value because clinical ambulatory pharmacy services are relatively new and do not currently enjoy stable or established revenue sources. Whether you are starting your ambulatory program, or currently have a program, the time to think about building quality measurement into your processes is now. Being proactive in this process not only will save you time and resources down the line, but it will allow you to have timely data when the demand inevitably arrives. This chapter will help you establish a framework for your ambulatory clinical care pharmacy quality improvement program, recommend a process for improvement for you to incorporate in your practice, and discuss how to ensure your staff is adequately skilled to provide quality patient care.
If you need to be convinced or need to convince someone regarding the importance of quality measurement, start with the report To Err Is Human: Building a Safer Health System released by the Institute of Medicine (IOM) Committee on Quality in America in 1999. This defining event elevated quality to priority status in health care because it brought to everyone’s attention the extent of harm being done to patients in our current health care system by reporting approximately 100,000 patient deaths in hospitals yearly due to medical error.1,2 The importance for pharmacy clinicians is the fact that medications were found to be the source of a significant portion of medical errors. Although data from the ambulatory setting was not included in the report, there is little doubt similar if not greater numbers of medication-related problems exist in this setting.3,4 The United Sates spends the most money to provide health care yet rates poorly in quality of care when compared to other industrialized countries.5,6 Compared with other industries concerned with public safety and quality, health care lags far behind.7 We enjoy the benefit of a safe airline industry, where the quality gap for safety between the highest performing airline and an airline performing in the middle of the industry’s quality range is less than 1%. Contrast that with data on the U.S. health care system reported by the National Committee on Quality Assurance (NCQA), where the quality gap is 20% or greater for a number of health care measures.8
Consequently, quality improvement and measurement programs are moving forward at a feverish pace. Multiple organizations, including accreditation organizations, are developing a whole host of quality measures for health care performance. Health care reform, and in particular The Patient Protection and Affordable Care Act enacted into law in 2010, has as major themes improved health care quality and affordable health care.9 Payers are increasing their reliance on attainment of quality measures for health care provider reimbursement in pay-for-performance models.10,11
What Is Quality?
Exactly what is meant by quality health care services, let alone quality clinical pharmacy services, and who is defining it? Thus far, the definition has been elusive, as a consensus definition does not currently exist.12-15 The IOM defines quality of care as the degree to which health services for individuals or populations increase the likelihood of desired health outcomes and are consistent with current professional knowledge.16 This definition connects quality to the experiences of patients and their outcomes, but it also broadens its scope to the general population level, which may provide a more significant impact for the entire health system. This definition implies that sound evidence-based research should direct services and the efforts to measure them. Less clear is exactly what the desired health outcomes are for any individual or population and who should define them: the patient, the provider, the payer, or a governmental agency.15 Approaching quality from each of these perspectives may result in very different sets of desired health outcomes. The patient-centered care movement and health care quality leaders advocate that quality efforts focus on the needs, desires, and circumstances of the individual patient. When patient-centered quality care is justly provided in this manner, quality will apply to larger populations and the entire health care system.14,17
 | The ambulatory patient-care pharmacists will experience pressures from a variety of sources when establishing their quality program. Improving the care and experience of patients served should always be the mission of any quality program. |
Understanding Your System of Care and Opportunities for Quality Improvement and Measurement
Today, providing care for illness and improving health for any particular patient or population group is exceedingly complex. Numerous points of interaction occur not only between one patient and one provider but also between one patient, multiple providers, health care-related organizations and payers, and subsequent countless interaction points with each additional patient served. An intricate layer of varying interdependence between these points creates a multitude of opportunity for cracks, flaws, and subsequent error, danger, and poor outcomes. Ambulatory care pharmacists must understand how their patient-care services interact with each patient’s unique system of care. Using the guidelines for a practice framework discussed in this book, your own focus on quality in your practice, as well as recommendations to follow in this chapter, will help you overcome this barrier.
 | Failure to recognize the complex connections can result in changes in care made with good intentions but that result in unexpected or untoward effects in another part of the patient’s system of care. |
Eighteen months after their initial report, the IOM released a follow-up report, Crossing the Quality Chasm, which described a framework of four levels of care where opportunities for quality improvement may occur.18 The first level is the experience of the patient and the patient’s community, or satisfaction with the health care provided. The components of care at this level focus on professionalism, which includes compassion, empathy, judgment, responsibility, fostering relationships, and communication. Patient satisfaction surveys are a useful means of measuring goals within this section. The second level constitutes the microsystems of care, or the small units (i.e., pharmacist-pharmacy technician, pharmacist-physician-nurse-office staff, etc.) that directly provide the care to the patient (Table 7-1). The IOM believes focusing on this level will provide the most meaningful and sizeable quality improvement. This is the level at which the majority of ambulatory patient-care pharmacists practice, and it is an ideal area to concentrate your quality improvement program. The third level is the health care organization. This level is responsible for health care resources and the supportive infrastructure that allows the microsystem to efficiently and effectively care for patients. The final level, the health care environment, focuses on financing, regulating, accrediting, and litigating the system; educating the workforce; and social policy.
Table 7-1. Examples of What May Constitute Ambulatory Microsystems with an Ambulatory Patient-Care Pharmacist
- Anticoagulation Clinic: Clinical pharmacist, registered nurse, medical physician, front desk appointment clerk, biller
- Medication Therapy Management Clinic: Clinical pharmacists, pharmacy technician, dispensing pharmacist, pharmacy manager
- Diabetes Clinic: Clinical pharmacist, diabetes nurse educator, dietician, endocrinologist, clinic support personnel, biller
- Patient-centered Medical Home: Primary care physician, nurse practitioner, pharmacist, physical therapist, certain specialists, dietician, office staff
 | In order for your clinic or service to work well and achieve the highest possible levels of quality care, each level must work in tandem and provide an acceptable level of quality. |
The first two levels of care are under your control and therefore areas where you can demonstrate quality and improve the care of your patients. For your service or microsystem to be successful, however, health care organizations and policy and rule makers need to provide a framework within which you perform improved care. Elements of quality at the third and fourth level are less within the control of practitioners in the microsystem.
 | As an ambulatory practitioner, you should understand what elements of quality are needed at the higher levels of care in order for you to accomplish your goals and actively work with your administrators at level three and your policy makers and pharmacy associations at level four so they understand what you need to achieve those goals. |
Before embarking on the details of your quality program, there are some principles for quality measurement that you should consider.17 Establishing principles for your program by which you choose your quality goals and measures will keep you focused and assist you in defining quality for your particular practice. It will help prevent goals and measures “gone wild,” where you may succumb to a significant amount of work collection data on measures that result in little meaningful improvement or quality in patient care. The principles are as follows:
- Knowledge-based care: The care you provide in your service is and continues to be based on current evidence and current standards of care. The service you provide and the quality measures you choose to evaluate your service should stem from the best known science and practice.
- Patient-centered care: The patient care you provide honors individuality, values, and ethnicity, and is sensitive to disparities and information needs for each patient. Your improvement plans and measures of quality embrace this principle.
- Systems-minded care: Your service is part of a complex matrix of patient care, and therefore you place a high value on cooperation and coordination of care across organizations, disciplines, and roles. When creating and interpreting your quality measures, you understand and consider this interplay.
- Measure what is important: Measure what will result in direct improvement to your patient population and what is high priority to you, your patients, and your organization. Measure what you can directly impact. For example, medication adherence may be problematic in your organization, so choose adherence as a measure with an associated clinical measure such as blood pressure or CD4 count, which will reflect a patient outcome related to improved adherence.
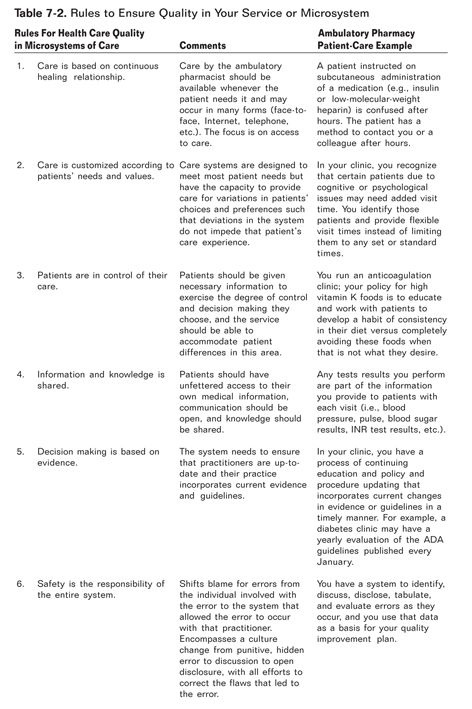
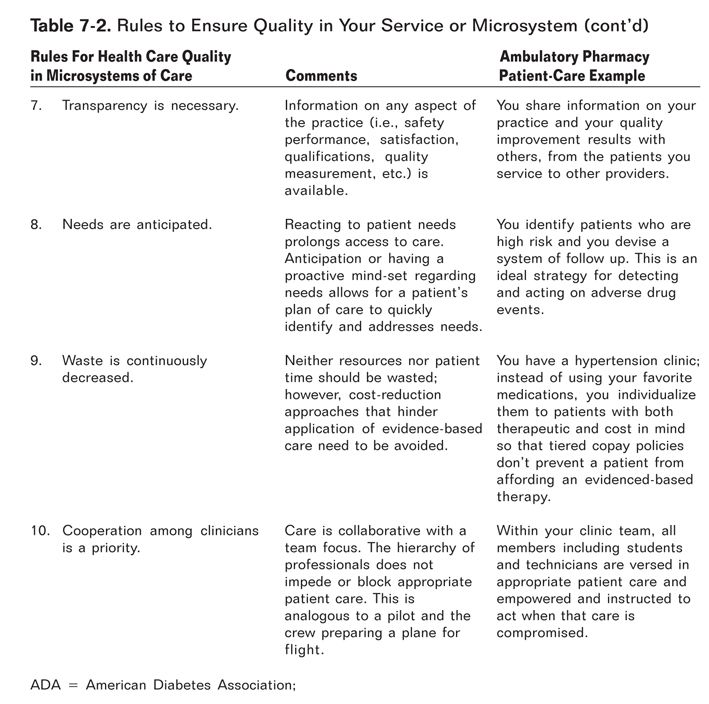
In addition you should examine the underlying framework of your system or services. If you lack a solid infrastructure, your aims of improvement may be sabotaged by an unexpected weak link. We know lapses in performing care or the system of patient-care process leads to lapses in quality and subsequent medical errors that affect patient safety and create poor outcomes and unnecessary costs.19 The IOM provides a simple set of 10 rules for a microsystem (i.e., your system or service) to use to evaluate the design of services (Table 7-2). Adopting these rules will increase the odds of your progress toward improvement and quality.
 | Measuring and ensuring an acceptable quality standard and patient centeredness within the structure, process, and direct provision of patient care in your system is critical to improving patient outcomes. |
Establishing a Quality Improvement Program
As you get started in your quality improvement program, it is helpful to start with three simple but extremely useful questions that will set in motion your plan. This approach is based on a well-established quality process used by many industries, referred to as the plan-do-study-act (PDSA) cycle.20 As stated by Glasgow, the PDSA cycle is akin to the scientific method in that it provides an overlying framework for approaching a problem, but does not explicitly proscribe the best methods for solving a problem.21 This allows you to customize your organization. Consider the first question:
· What are we trying to accomplish?
The answer to this question stems from the mission and vision of your particular clinic or program. You may be an anticoagulation clinic whose purpose is the safe use of anticoagulants, or a medication therapy management clinic (MTM) whose mission is to improve medication adherence and decrease adverse drug events. You may be planning to establish a diabetes service to address a large number of poorly controlled diabetes cases in your patient population or a heart failure clinic to address frequent hospitalizations noted in your health system’s population. In the first two examples, your next step will be to collect a sufficient sample of key data to determine if indeed you are meeting the goals that you are trying to accomplish. For example, in the anticoagulation clinic or the MTM clinic you may want to look at hospitalizations due to warfarin complications or medications problems. In the latter two examples, your institution or payer source may have already collected and provided you with the number of HgA1c readings greater than 8 or the number of yearly hospitalizations for patients with a heart failure diagnosis. If not, you may need to collect that baseline information.
This brings you to the next question:
· What change can we make that will result in improvement?
With this question, you critically evaluate and adjust your current services or proposed services, using the best scientific evidence and standards of practice, to create a solution that will accomplish your goal. Review similar pharmacy-run (or other provider-run) clinics that have published what they did to improve outcomes of their patient population. For example, you know your medication adherence program population is elderly, with low health literacy and declining cognition. In a review of the literature, you find a study by Lee et al., who provided comprehensive pharmacy services similar to yours, but they also used a “pill box” concept and had impressive adherence rates with improved clinical markers as their outcome. The change you decide to propose is to add the use of pill boxes to your services. The best way to approach this is through the microsystem team. Including the entire team will provide the unique perspective from each member when devising the plan for change and therefore strengthen the plan by reducing unanticipated barriers. Being inclusive will also gain you “buy in” from the team so that members personally care about the change, improving your chances of successes.
· How will we know that a change is an improvement?
This final question stresses the importance of carefully choosing your quality measures. If available, you may want to use measures already published in the health care quality literature that have been tested, and are known to reflect a level of improvement. Reviewing the literature on similar clinics or services and evaluating what they used as measures may provide you some benchmarks as well as identify barriers. However, a measure important to your particular practice may not have such scientific validation. A good strategy in this situation is to run a small pilot of the measure to assure it is providing you the information that reflects what you have implemented.
The essential steps to the PDSA model are outlined below. We will take a closer look at each step. ![]() You may wish to use the PDSA work sheet (Figure 7-1) to begin to formulate your particular project as you go through the remainder of the chapter.22
You may wish to use the PDSA work sheet (Figure 7-1) to begin to formulate your particular project as you go through the remainder of the chapter.22
The Planning Phase
1. Set aims: Define what you are trying to fix or accomplish.
2. Find promising strategies for change: Use your team, literature review, innovation, and problem-solving skills to reengineer the patient-care system and services.
3. Define measurements: Choose tools that measure the level of achievement of the aims.
The Do Phase
| 4. | Implement the change: As a team, inform all involved (patients, other providers, etc.) of the change and implement it in an organized manner. |
The Study Phase
| 5. | Test those ideas: Determine if the new ideas for change result in improvement. |
The Act Phase
| 6. |