Patient Story
A 32-year-old man was diagnosed with Crohn disease 10 years prior to his visit for these nonhealing leg ulcers (Figure 174-1). The patient experienced minor trauma to his lower leg 1 year ago and these ulcers developed (pathergy). Multiple treatments have been tried with partial success, but the ulcers persist.
Introduction
Epidemiology
- PG occurs in approximately 1 person per 100,000 people each year.1
- No racial predilection is apparent.
- A slight female predominance may exist.
- Predominately occurs in fourth and fifth decade, but all ages may be affected.
Etiology and Pathophysiology
- Etiology is poorly understood.
- Pathergy (initiation at the site of trauma or injury) is a common process and it is estimated that 30% of patients with PG experienced pathergy.1
- Up to 50% of cases are idiopathic.2
- At least 50% of cases are associated with systemic diseases such as inflammatory bowel disease, hematologic malignancy, and arthritis.2
- It occurs in up to 5% of patients with ulcerative colitis and 2% of those with Crohn disease (Figures 174-2 and 174-3).3,4
- Biopsies usually show a polymorphonuclear cell infiltrate with features of ulceration, infarction, and abscess formation.
Risk Factors
- Ulcerative colitis.2,5
- Crohn disease.
- Polyarthritis (seronegative or seropositive).
- Hematologic diseases/disorders such as leukemia (predominantly myelocytic).
- Monoclonal gammopathies (primarily immunoglobulin A).
- Psoriatic arthritis and rheumatoid arthritis (Figure 174-4).
- Hepatic diseases (hepatitis and primary biliary cirrhosis).
- Immunologic diseases (lupus erythematosus and Sjögren syndrome).
Diagnosis
- Typically PG presents with deep painful ulcer with a well-defined border, which is usually violet or blue. The color has also been described as the color of gun metal. The ulcer edge is often undermined and the surrounding skin is erythematous and indurated. It usually starts as a pustule with an inflammatory base, an erythematous nodule, or a hemorrhagic bulla on a violaceous base. The central area then undergoes necrosis to form a single ulcer.5
- The lesions are painful and the pain can be severe.2 Patients may have malaise, arthralgia, and myalgia.
- Two main variants of PG exist: classic and atypical.2
- Classic PG is characterized by a deep ulceration with a violaceous border that overhangs the ulcer bed.2 These lesions of PG most commonly occur on the legs (Figures 174-1 and 174-3, 174-4, and 174-5).2
- Atypical PG has a vesiculopustular wet component (Figures 174-8 and 174-9). This is usually only at the border, is erosive or superficially ulcerated, and most often occurs on the dorsal surface of the hands, the extensor parts of the forearms, or the face.2
- Classic PG is characterized by a deep ulceration with a violaceous border that overhangs the ulcer bed.2 These lesions of PG most commonly occur on the legs (Figures 174-1 and 174-3, 174-4, and 174-5).2
- Other variants:
- Peristomal PG may occur around stoma sites. This form is often mistaken for a wound infection or irritation from the appliance.6
- Vulvar or penile PG occurs on the genitalia and must be differentiated from ulcerative sexually transmitted diseases (STDs) such as chancroid and syphilis.2
- Intraoral PG is known as pyostomatitis vegetans. Occurs primarily in patients with inflammatory bowel disease.2
- Peristomal PG may occur around stoma sites. This form is often mistaken for a wound infection or irritation from the appliance.6
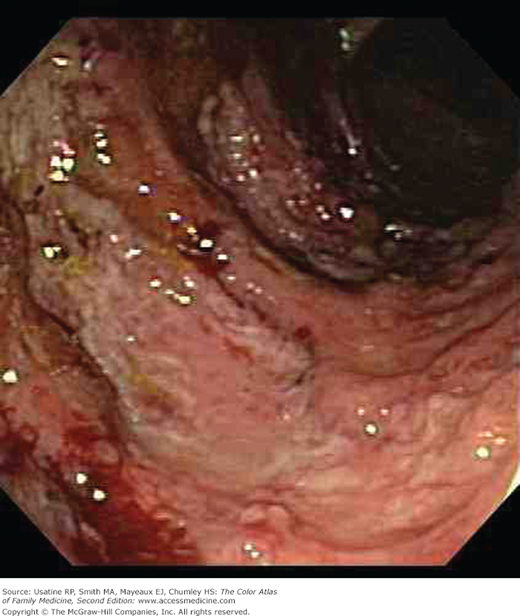
Figure 174-7
Partially healed pyoderma gangrenosum on the leg of a 29-year-old Hispanic woman. Note the areas of healed ulcerations and the dusky elevated borders. There remain 2 areas of active disease (arrows) with pain, erythema, swelling, and purulent discharge. The patient improved with dapsone. (Courtesy of Richard P. Usatine, MD.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree