Primary Mediastinal (Thymic) Large B-cell Lymphoma
Francisco Vega, MD, PhD
Key Facts
Terminology
Diffuse large B-cell lymphoma (DLBCL) arising in mediastinum of putative thymic B-cell origin
Clinical Issues
Most frequent from 20-35 years
M:F ratio = 1:2
Enlarging mass in anterior-superior mediastinum
Frequent infiltration of mediastinal structures and organs
Prognosis is similar to patients with other types of DLBCL
60-70% chance of cure with appropriate therapy
Microscopic Pathology
Diffuse to vaguely nodular growth pattern usually associated with variable degrees of sclerosis
Interstitial sclerosis with compartmentalization of tumor cells
Hodgkin-like or Reed-Sternberg-like cells can be present
Ancillary Tests
CD20(+), CD45/LCA(+), IRF-4/MUM1(+/−)
CD30(+) ˜ 75%, usually weak &/or focal
CD10(−), CD15(−), Cyclin-E(−)
Monoclonal Ig gene rearrangements
Top Differential Diagnoses
Nodular sclerosis Hodgkin lymphoma
B-cell lymphoma, unclassifiable, with features intermediate between DLBCL and CHL
Diffuse large B-cell lymphoma
T-lymphoblastic leukemia/lymphoma
TERMINOLOGY
Abbreviations
Primary mediastinal (thymic) large B-cell lymphoma (PMLBCL)
Synonyms
Mediastinal large B-cell lymphoma
Thymic large B-cell lymphoma
Definitions
Diffuse large B-cell lymphoma (DLBCL) arising in mediastinum of putative thymic B-cell origin
ETIOLOGY/PATHOGENESIS
Cell of Origin
Thymic B cell is presumed
CLINICAL ISSUES
Epidemiology
Incidence
2% of all non-Hodgkin lymphomas
Age
Most frequent from 20-35 years
Gender
M:F ratio = 1:2
Presentation
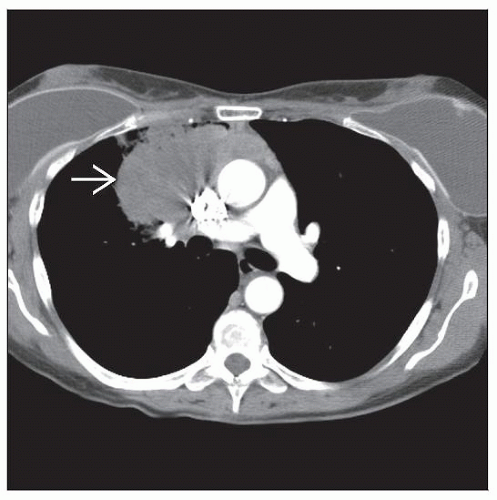
Enlarging mass in anterior-superior mediastinum
Often manifests as bulky disease defined as > 10 cm in diameter
˜ 75% of patients
B symptoms in 20-30%
PMLBCL patients have distinctive serum chemistry profile
Low serum β2 microglobulin and high lactate dehydrogenase (LDH) levels
Locally aggressive with compression of contiguous organs
Superior vena cava syndrome occurs in up to 30% of patients
Frequent infiltration of local structures and organs
Lung parenchyma, chest wall, pleura, and pericardium
Extrathoracic disease at diagnosis is rare
Bone marrow infiltration at presentation is also rare
Extrathoracic sites are often involved at relapse
Central nervous system, liver, adrenals, ovaries, and kidneys
Treatment
Drugs
Systemic chemotherapy is required; many regimens can be used
R-CHOP, rituximab, cyclophosphamide, hydroxydaunorubicin (doxorubicin), Oncovin (vincristine), prednisone
MACOPB, methotrexate, leucovorin, doxorubicin, cyclophosphamide, vincristine, prednisone, bleomycin
DA-EPOCH+R, etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin plus rituximab
HyperCVAD-R, high-dose cyclophosphamide, vincristine, doxorubicin, cytarabine, methotrexate, rituximab
If risk factors are present, central nervous system prophylaxis is recommended
High-dose methotrexate therapy
Radiation
Involved field therapy can be used for patients with bulky disease
IMAGE FINDINGS
Radiographic Findings
Large mass in anterior-superior mediastinum
Often FDG-PET scan positive
MACROSCOPIC FEATURES
General Features
Unusual for mass to be resected based on size and location
In resection specimens, residual thymus gland may be identified
Currently, diagnosis is often established by needle biopsy
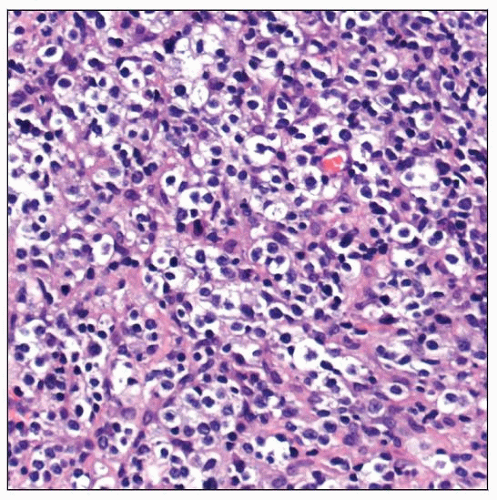
MICROSCOPIC PATHOLOGY
Histologic Features
Diffuse to vaguely nodular growth pattern usually associated with variable degrees of sclerosis
Interstitial sclerosis surrounds and compartmentalizes small groups of tumor cells
Broad collagenous bands divide tumor into large nodules
Intermediate to large lymphoid cells
Pale cytoplasm, often result of retraction artifact
HRS-like cells can be present
Reactive infiltrate of small T lymphocytes and histiocytes
± plasma cells and eosinophils
Thymic components, such as Hassall corpuscles, may be identified
If present, supports thymic involvement and diagnosis of PMLBCL
Cytologic Features
Large lymphoma cells are present in fine needle aspiration smears
Not readily distinguishable from other types of large B-cell lymphoma
Extensive sclerosis can reduce yield of neoplastic cells aspirated
ANCILLARY TESTS
Immunohistochemistry
Positive for common pan-B-cell markers
CD19, CD20, CD22, CD79a
Positive for B-cell transcription factors
BOB1, OCT2, PU.1, pax-5
CD45/LCA(+), p63(+) in ˜ 95%
CD30(+/−), in ˜ 75% of cases
Expression is usually weak &/or focal
IRF-4/MUM-1(+) in ˜ 75%
CD23(+/−), MAL(+/−)
Bcl-2(+/−), Bcl-6(+/−); staining intensity can be variable
CD10(−), CD15(−)
T-cell antigens(−)
EBV LMP is usually negative
Cyclin-D1(−), Cyclin-E(−)
Flow Cytometry
B-cell immunophenotype
Discordance in B-cell receptor expression is common in PMLBCL
Surface Ig(−) and CD79a(+)
Variable loss of HLA class I and II (HLA-DR) molecules
Cytogenetics
Comparative genomic hybridization
Common regions of gain
Gains in 9p24 ˜ 75% and 2p15 ˜ 50%
Gains in chromosome X and in 12q31
JAK2 at 9p24 is not mutated
Common regions of loss
1p, 3p, 13q, 15q, and 17p
Well-characterized chromosomal translocations are rare/absent in PMLBCL
CCND1, BCL2, BCL6, and MYC
In Situ Hybridization
EBER(−)
Molecular Genetics
Monoclonal Ig gene rearrangements
No monoclonal T-cell receptor gene rearrangements
High frequency of BCL6 gene mutations
SOCS1 mutations in subset of cases
High levels of expression of
IL-13 receptor
JAK2 and STAT1
Gene Expression Profiling
Studies have shown overlap in gene expression profile between PMLBCL and classical Hodgkin lymphoma
Signature is distinct from nodal DLBCLs
Either germinal center B-cell or activated B-cell types
Activation of NF-κB
Nuclear location of c-REL
Cytoplasmic expression of TRAF1
Combination of nuclear c-REL with expression of TRAF1 is highly specific for PMLBCL
DIFFERENTIAL DIAGNOSIS
Nodular Sclerosis (NS) Classical Hodgkin Lymphoma (CHL)
Usually young patients
Slight female predominance
Mediastinal involvement in ˜ 80%
Histologic features
Nodular growth pattern with fibrosis
Dense collagenous bands surround nodules
Collagenous bands are polarizable
Variable numbers of large Hodgkin/lacunar and Reed-Sternberg (HRS) cells
Many inflammatory cells present
Eosinophils, neutrophils, plasma cells
Many histologic variants of nodular sclerosis CHL have been described
Based on number of neoplastic cells, extent and nature of fibrosis, and inflammatory background
Syncytial variant is most relevant
Sheets of large HRS cells can mimic DLBCL
Often large areas of necrosis
Immunophenotype typical of CHL
Immunophenotype of CHL
CD30(+), CD15(+/−)
pax-5 (+) with characteristic weaker (dim) expression than reactive B cells
CD20(−/+), CD79a(−/+)
Weakly &/or variably positive in 20% of cases
Other B-cell transcription factors absent or dimly expressed
CD45/LCA(−), EMA usually negative
Small subset (˜ 5%) of CHL can express T-cell antigens
Molecular genetic features
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree