Primary Cutaneous Follicle Center Lymphoma
Roberto N. Miranda, MD
Key Facts
Terminology
Lymphoma arising in skin composed of follicular center cells
Subset of cases appear to be clinically and genetically distinct from nodal FL
Clinical Issues
Usually solitary, erythematous lesion in head and neck
Therapy with local radiation or surgical excision
Prognosis favorable, even in patients with multiple skin lesions
5-year survival rate is 95%
Microscopic Pathology
Dermal lymphoid follicular infiltrate that spares epidermis
Ancillary Tests
CD10(+) in cases with follicular pattern
Bcl-6(+); Bcl-2(+/-) in up to 60% of cases
PCFCL that is CD10(+), Bcl-2(+) likely carries t(14;18) (q32;q21)
˜ 30% of PCFCL cases have t(14;18) by FISH
Top Differential Diagnoses
Secondary follicular lymphoma of skin
Usually strongly CD10(+) and Bcl-2(+)
BCL2 gene rearrangements in ˜ 80-90% of cases
Cutaneous marginal zone B-cell lymphoma
Primary cutaneous diffuse large B-cell lymphoma (PCLBCL), leg type
PCLBCL, other (non-leg type)
Cutaneous follicular hyperplasia
TERMINOLOGY
Abbreviations
Primary cutaneous follicle center lymphoma (PCFCL)
Synonyms
Follicular lymphoma (FL) of skin
Follicular center cell lymphoma
Centroblastic/centrocytic lymphoma
PCFCL on back previously referred to as
Reticulohistiocytoma of the dorsum
Crosti disease
Definitions
Lymphoma arising in skin composed of follicular center cells
Confined to skin for at least 6 months upon staging
Mainly centrocytes (small cleaved cells); less frequently centroblasts (large cleaved and noncleaved cells)
Follicular or diffuse growth pattern
Recently defined as entity; diagnostic criteria may require further refinement
Some published cases with diagnosis based on clinicopathologic findings; lack evidence of clonality
Subset of cases appear to be clinically and genetically distinct from nodal FL
BCL2 gene rearrangements less frequent than in nodal FL
ETIOLOGY/PATHOGENESIS
Etiology
Unknown
Cell of Origin
Mature germinal center B lymphocyte
CLINICAL ISSUES
Epidemiology
Incidence
2nd most common extranodal B-cell lymphoma after gastrointestinal lymphomas
0.1-0.2 per 100,000 persons per year
Age
Affects adults; median 60 years (range 33-88 years)
Gender
Male to female ratio is 1.5:1
Site
Usually in head and neck
Affects mainly scalp and forehead
Less frequent on trunk
Legs affected in 5% of cases
Presentation
Usually solitary, firm, and erythematous to violaceous lesion
May be plaques, nodules, or tumor masses of variable size
Lesions range from < 1 cm to large, confluent nodules > 40 cm in diameter
Multifocal in 15% of patients
Presentation on trunk is usually preceded by erythematous papules or figurate plaques
This form was designated in past as “reticulohistiocytoma of the dorsum”
Natural History
Lesions gradually increase in size if left untreated
Dissemination to extracutaneous sites is uncommon (˜ 10%)
Recurrences occur at proximal site compared with initial site of presentation
Recurrences occur in 30-40% of patients
Treatment
Local radiation or surgical excision of lesions
Systemic therapy required for patients with
Extensive disease, very thick skin tumors, or extracutaneous disease
Prognosis
Favorable, even in patients with multiple skin lesions
Most patients achieve complete remission with therapy
Survival is 95% at 5 years; not affected by presence of
Follicular or diffuse growth pattern or cytologic grade
t(14;18) or BCL2 gene rearrangements
Extent or relapse of disease
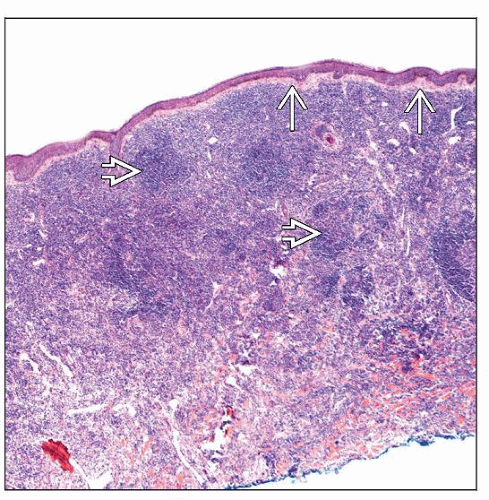
MICROSCOPIC PATHOLOGY
Histologic Features
Dermal infiltrate that spares epidermis (grenz zone)
Growth patterns
Pure follicular
Mixed follicular and diffuse
Pure diffuse
Cell composition
Small- to intermediate-sized centrocytes admixed with variable amount of large centroblasts
Grading is not recommended for PCFCL
Amount of large cells in follicles does not influence prognosis in patients with PCFCL
Lymphoid follicles and germinal centers are better appreciated in small or incipient lesions
Follicles are ill defined and composed of rather monotonous lymphoid population
Usually, tingible body macrophages are absent
Attenuated or absent mantle zones
Variable amounts of sclerosis
Infiltrate may reach subcutaneous tissue in ˜ 75% of cases
Most follicles in deep dermis (‘bottom heavy”)
Advanced lesions show less conspicuous follicles, if present
Usually composed of multilobated, cleaved, or spindle-shaped lymphocytes
Remnants of follicular dendritic cells (FDCs)
Extreme cases with many centroblasts simulate DLBCL
Should be considered as PCFCL if follicular component
Considered to share excellent prognosis of other, more typical PCFCL
DLBCL is diagnosed when large cells grow in pure diffuse pattern
ANCILLARY TESTS
Immunohistochemistry
Pan-B-cell antigens(+), pax-5(+)
CD10 is typically positive but can be negative in cases with diffuse pattern
CD10(+) cell clusters may be found in interfollicular areas
Bcl-6(+) consistently found in follicles
Bcl-2(+/−) in up to 60% of cases
When positive, Bcl-2 is often dim
(+) more frequently in cases with follicular pattern
PCFCL that are CD10(+) and Bcl-2(+) likely carry t(14;18)(q32;q21)
Monotypic B lymphocytes can be detected in fixed, paraffin-embedded tissue sections
˜ 1-20% using routine immunohistochemistry
Role of mRNA expression of κ and λ in cutaneous infiltrates not established
IRF-4/MUM1 and FOXP1 are usually (−)
Cytoplasmic IgM(−), IgD(−)
Underlying FDC network: CD21(+), CD23(+), &/or CD35(+)
T-cell antigens(−)
Variable number of reactive small T-lymphocytes
Flow Cytometry
In Situ Hybridization
˜ 30% of PCFCL cases have t(14;18) by FISH
Array CGH
Chromosomal imbalances in minority of cases
Molecular Genetics
Monoclonal Ig gene rearrangements
Detected by PCR in 40-50% of cases
Somatic hypermutation of Ig genes is common
IgH-BCL2 fusion occurs at variable frequency in PCFCL
Gene Expression Profiling
Gene expression profile similar to germinal center-like large B-cell lymphoma
REL gene amplification is common
DIFFERENTIAL DIAGNOSIS
Secondary Follicular Lymphoma (FL) of Skin
Evidence of systemic FL elsewhere
Head and neck are most frequent sites
Immunophenotype
Bcl-6(+), CD10(+), Bcl-2(+)
IgH-BCL2/t(14;18)(q32;q21) in ˜ 80-90% of cases
Marginal Zone B-cell Lymphoma of Skin
Usually multifocal
Previous nomenclature included
B-cell lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma)
Cutaneous immunocytoma
Cutaneous follicular lymphoid hyperplasia with monotypic plasma cells
Indolent low-grade lymphoma, 99% 5-year survival
Association with Borrelia burgdorferi, mostly in Europe
Marginal zone and interfollicular distribution
Mixed cell composition
Marginal zone (centrocyte-like) cells
Monocytoid cells or small round lymphocytes
Scattered large cells, centroblast-like
± plasma cell differentiation
Subepidermal or at advancing edge of tumor
Immunophenotype
B-cell antigens(+), CD10(−), Bcl-6(−)
Monotypic cytoplasmic Ig in cases with plasmacytoid differentiation
Clusters of reactive CD123(+) plasmacytoid dendritic cells are common
Underlying disrupted and colonized germinal centers highlighted by FDC markers
Residual germinal center cells are CD10(+) and Bcl-6(+)
Primary Cutaneous Diffuse Large B-cell Lymphoma (PCLBCL), Leg Type
Disease of elderly
Rapidly growing tumors with 50% 5-year survival
Primarily affects lower extremities; occasionally occurs at other body sites
Diffuse and monotonous infiltrate composed of large centroblasts or immunoblasts
Absence of neoplastic follicles and small or large centrocytes
Distinct from DLBCL with centrocytes or neoplastic follicles
Non-germinal center cell (activated B-cell) immunophenotype
B-cell antigens(+), cytoplasmic IgM(+), Bcl-6(+)
Bcl-2(+), IRF-4/MUM1(+), FOXP1(+)
CD10(−), CD138(−)
Primary Cutaneous Diffuse Large B-cell Lymphoma (PCLBCL), Other (Non-Leg Type)
Includes DLBCL that does not fit with
PCLBCL leg type
PCFCL with diffuse large cells
Also encompasses T cell-rich large B-cell lymphoma and plasmablastic lymphoma
Large neoplastic cells are admixed with inflammatory reactive infiltrate
Phenotype may be germinal and non-germinal center type
Lymphoma of adults with slightly better prognosis than PCLBCL leg type
Cutaneous Follicular Hyperplasia
Lesions of variable ages; may be associated with
Insect or tick bites
Hair follicle inflammation
Well-defined follicles with distinct germinal centers and mantle zones
Most follicles are in superficial dermis (‘top heavy”)
Frequent tingible body macrophages
Immunophenotype
Mixture of B cells and T cells; often in compartments
Germinal centers are Bcl-6(+), Bcl-2(−)
No evidence of monoclonal Ig gene rearrangements
DIAGNOSTIC CHECKLIST
Clinically Relevant Pathologic Features
FL confined to skin for at least 6 months upon staging
Pathologic Interpretation Pearls
Grading is not recommended for PCFCL
Lower frequency of t(14;18)/IgH-BCL2 than in nodal FL
SELECTED REFERENCES
1. Koens L et al: IgM expression on paraffin sections distinguishes primary cutaneous large B-cell lymphoma, leg type from primary cutaneous follicle center lymphoma. Am J Surg Pathol. 34(7):1043-8, 2010
2. Dijkman R et al: Array-based comparative genomic hybridization analysis reveals recurrent chromosomal alterations and prognostic parameters in primary cutaneous large B-cell lymphoma. J Clin Oncol. 24(2):296-305, 2006
3. Hoefnagel JJ et al: Distinct types of primary cutaneous large B-cell lymphoma identified by gene expression profiling. Blood. 105(9):3671-8, 2005
4. Kim BK et al: Clinicopathologic, immunophenotypic, and molecular cytogenetic fluorescence in situ hybridization analysis of primary and secondary cutaneous follicular lymphomas. Am J Surg Pathol. 29(1):69-82, 2005
5. Kodama K et al: Primary cutaneous large B-cell lymphomas: clinicopathologic features, classification, and prognostic factors in a large series of patients. Blood. 106(7):2491-7, 2005
6. Willemze R et al: WHO-EORTC classification for cutaneous lymphomas. Blood. 105(10):3768-85, 2005
7. Goodlad JR et al: Primary cutaneous diffuse large B-cell lymphoma: prognostic significance of clinicopathological subtypes. Am J Surg Pathol. 27(12):1538-45, 2003
8. Goodlad JR et al: Primary cutaneous follicular lymphoma: a clinicopathologic and molecular study of 16 cases in support of a distinct entity. Am J Surg Pathol. 26(6):733-41, 2002
9. Mirza I et al: Primary cutaneous follicular lymphoma: an assessment of clinical, histopathologic, immunophenotypic, and molecular features. J Clin Oncol. 20(3):647-55, 2002
10. Aguilera NS et al: Cutaneous follicle center lymphoma: a clinicopathologic study of 19 cases. Mod Pathol. 14(9):828-35, 2001
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree