Primary Cutaneous Anaplastic Large Cell Lymphoma
C. Cameron Yin, MD, PhD
Key Facts
Terminology
Cutaneous lymphoma composed of large T cells that express CD30 (> 75%)
Clinical Issues
Common sites: Face, trunk, and extremities
Solitary nodule or localized nodules/papules; ± ulceration
Multifocal lesions occur in ˜ 20% of patients
Extracutaneous dissemination in ˜ 10% of patients
Spontaneous regression can occur; relapse is common
Favorable prognosis with 10-year survival of ˜ 90%
Microscopic Pathology
Diffuse infiltrates of large neoplastic cells mainly located in dermis; can extend into subcutaneous tissue
Variable inflammatory cell infiltrate in background
Anaplastic cells in most cases; ˜ 20% nonanaplastic
Ancillary Tests
> 75% of neoplastic large cells CD30(+)
CD4(+), cytotoxic proteins(+), cutaneous lymphocyte antigen (+/-)
CD56(-/+), EMA(-), CD15(-), ALK(-)
No specific cytogenetic abnormalities identified
Monoclonal T-cell receptor rearrangements
Top Differential Diagnoses
Systemic ALK(-) ALCL with cutaneous involvement
Large cell transformation of mycosis fungoides
Lymphomatoid papulosis, type C
Peripheral T-cell lymphoma, NOS
TERMINOLOGY
Abbreviations
Primary cutaneous anaplastic large cell lymphoma (C-ALCL)
Synonyms
Primary cutaneous CD30(+) T-cell lymphoproliferative disorder
This term also includes lymphomatoid papulosis
Definitions
Cutaneous lymphoma composed of large T cells that express CD30 (> 75%)
ETIOLOGY/PATHOGENESIS
Unknown
CD30/TRAF1/IRF-4 activation induced upregulation of NF-κB is implicated
Other suggested factors
Viral infection, reduced immunosurveillance
Chronic antigenic stimulation, direct oncogenic effect of immunosuppressive drugs
Gene expression profiling has failed to show genes that clearly distinguish C-ALCL from ALK(-) systemic ALCL
Increased expression of skin-homing chemokine receptors may play a role in confining C-ALCL to skin
CLINICAL ISSUES
Epidemiology
Age
Median: 60 years
Gender
M:F = 2-3:1
Site
Common sites: Face, trunk, and extremities
Presentation
Solitary nodule or localized nodules or papules; ± ulceration
Multifocal lesions occur in ˜ 20% of patients
Extracutaneous dissemination in ˜ 10% of patients
Regional lymph nodes; rarely viscera
Partial or complete spontaneous regression can occur; relapse is common
Treatment
Irradiation for localized nodules
Low-dose methotrexate for multifocal lesions
Extracutaneous tumors require systemic chemotherapy
Prognosis
Favorable, with 10-year survival of ˜ 90%
Similar prognosis for patients with localized vs. multifocal skin lesions
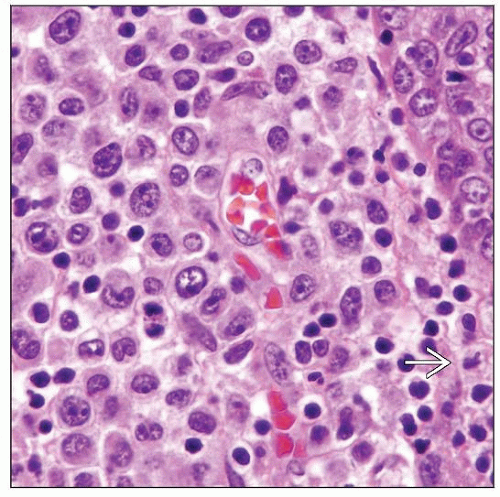
MICROSCOPIC PATHOLOGY
Histologic Features
Diffuse infiltrates of large neoplastic cells mainly located in dermis; can extend into subcutaneous tissue
Epidermal involvement ± ulcer
Variable degree of inflammatory infiltrate consisting of reactive T-cells, histiocytes, eosinophils, and neutrophils
Biopsy lesions can be eosinophil-rich or neutrophilrich (pyogenic)
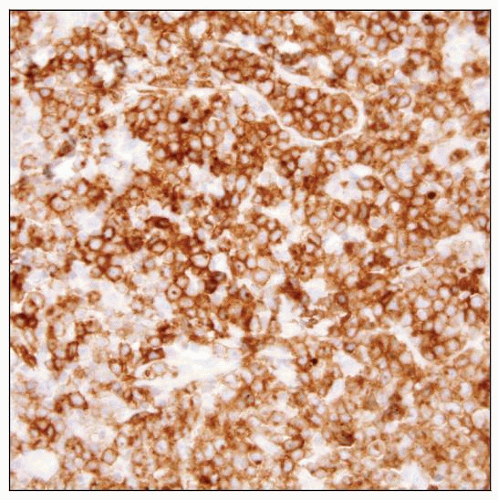
ANCILLARY TESTS
Immunohistochemistry
> 75% of neoplastic large cells are CD30(+)
Activated CD4(+) T-cell phenotype
Rarely show CD8(+) T cell or null CD4(-)/CD8(-) immunophenotype
Variable loss of pan-T-cell antigens: CD2, CD3, CD5, T-cell receptor (βF1)
Cytotoxic proteins(+), cutaneous lymphocyte antigen (+/-)
CD56(-/+), EMA(-), CD15(-), ALK(-)
Cytogenetics
No specific cytogenetic abnormalities identified
No translocations involving ALK gene at chromosome 2p23
Array-based comparative genomic hybridization has revealed chromosomal imbalances
Gains in 7q, 17q, 21; losses in 3p, 6q, 8p, 13q
Molecular Genetics
Most cases show monoclonal T-cell receptor rearrangements
DIFFERENTIAL DIAGNOSIS
Systemic ALK(+) ALCL with Cutaneous Involvement
Children and young adults
Peripheral lymph nodes and extranodal sites (+)
CD30(+), ALK(+)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree