Patient Story
As a longtime pregnancy care provider, it was difficult to choose a single story as representative of pregnancy and birth. Most of the stories are meaningful because of the context of the relationship with the woman and the family—a few are tragic and yet filled with grace and the amazing strength displayed by even the very young, some are truly epic tales, and all are learning opportunities. Pregnancy experiences are filled with consternation at the myriad of changes, discomforts, and worries. They are filled with laughter as women’s bodies alter in amazing ways; we waddle, unconsciously rest plates on our bellies, and lose sight of our feet (Figure 4-1). Our partners and/or supportive others alternate between reassurance and befuddlement. And then a child appears, miraculously from a space that seems far too small to accommodate, and (regardless of the outcome) a new journey begins.
Epidemiology
- Planned pregnancy—Approximately 85% of sexually active women not using a contraceptive method will become pregnant over the course of a year. The probability of conception is 15% to 33% per cycle, depending upon the frequency of sexual intercourse.1
- Unplanned pregnancy—Half of all pregnancies in the United States are unintended, and approximately half of these unintended pregnancies end in abortion.2
- • Unintended pregnancy (defined as a pregnancy mistimed or not wanted at the time conception occurred) is the result of lack of use of a contraceptive or failure of the contraceptive.
- • Unintended pregnancy occurs among women of all ages, socioeconomic status, and marital status. Although unintended pregnancies are often associated with teens, 41% of pregnancies among women 35 to 39 years of age and 51% of those among women older than 40 years are unintended.3
- • Some unintended pregnancies end in abortions. A total of 827,609 legally induced abortions occurred in the United States in 2007 (16 per 1000 women aged 15 to 44 years).4
- The highest percentages of reported abortions were for women who were unmarried (82%), white (55%), and aged <25 years (51%).
- Of all abortions for which gestational age was reported, 62.3% were performed at ≤8 weeks’ gestation.4
- • Unintended pregnancy (defined as a pregnancy mistimed or not wanted at the time conception occurred) is the result of lack of use of a contraceptive or failure of the contraceptive.
- Maternal mortality has declined dramatically in the United States over the past century. Rates declined from 607.9 maternal deaths per 100,000 livebirths in 1915 to 12.7 per 100,000 livebirths in 2007. Still, maternal mortality over the past 25 years has not improved.5 The leading causes of pregnancy-related death are embolism (20%), hemorrhage (17%), and pregnancy-induced hypertension (16%).6 Major racial disparities continue to exist.
- • Maternal mortality (2007) in non-Hispanic black women was 34 per 100,000 live births compared with 10.4 per 100,000 live births in non-Hispanic whites and 9.6 per 100,000 live births in Hispanics. African-American women have 2.7 times the risk of pregnancy-related death compared with whites.
- Care delivery by family physicians (Figure 4-2)—Eighteen percent of family physicians perform deliveries as a regular part of their practice; 19.6% perform vacuum extraction; 6.9% do forceps deliveries; 6.3% offer trial of labor after cesarean delivery; and 7.3% perform cesarean deliveries.7
- Care outcomes by family physicians—Several studies compare outcomes between family physicians and obstetricians, primarily for comparable patients at low maternal risk (although proportions of high-risk patients are frequently similar across disciplines). One study examining management of vaginal delivery found that obstetricians are more likely to perform episiotomies than family physicians; no difference between groups was noted for instrument use (vacuum or forceps) or neonatal outcomes.8 Another study comparing rates of trial of labor attempts and vaginal birth after cesarean (VBAC) rates found a trial of labor attempt rate of 81.1% for family physicians and 50.6% for obstetricians. Success rates were 76.1% for family physicians and 64.3% for obstetricians (P = 0.002), although there was a statistically nonsignificant higher uterine rupture/dehiscence rate in the family physician group.9
Etiology and Pathophysiology
- The most fertile period for women is the several days prior to ovulation and ends 24 hours after ovulation.10 The ovum is able to be fertilized for only 12 to 24 hours after ovulation.10
- Sperm usually remain viable for 3 days after intercourse.
- Once the egg is fertilized, it is transported to the uterine cavity in approximately 2 to 3 days. Implantation occurs approximately 6 to 7 days after fertilization following cell division that forms a blastocyst.10
- Pregnancy is defined by the National Institutes of Health, the American College of Obstetricians and Gynecologists, and the Food and Drug Administration as implantation of the blastocyst in the endometrium.11
- The precise cause of labor is not known but the physiologic changes prior to labor onset include decreased placental progesterone secretion and stimulation of prostaglandin production (E2 and F2α) from the decidua, uterine endometrium, and fetal membranes.
- Labor is defined as progressive dilation of the cervix with uterine contractions. Bloody show (blood-tinged mucus from the vagina), indicating extrusion of the mucus plug, is helpful in predicting impending labor onset.
Diagnosis
A detailed menstrual history should be obtained with the goal of accurately determining the first day of the most recent menstrual cycle. This date is traditionally used to calculate the estimated date of delivery (EDD) by using Naegele’s rule (EDD = [first day of last menstrual period minus 3 months] plus 7 days). The rule is most useful in women who have regular 28-day cycles followed by an abrupt cessation of menses.
- Common early symptoms include amenorrhea, nausea, fatigue, and breast tenderness.
- Signs of pregnancy include the following:
- Alterations in the skin (e.g., a hyperpigmented streak appearing below the umbilicus [linea nigra] and a reddish hyperpigmentation over the bridge of the nose and cheeks [chloasma]) (Figure 4-3).
- Alterations in the vulva, vagina, and cervix (i.e., bluish discoloration [Chadwick sign] caused by vascular engorgement of the pelvic organs and softening of the cervix [Hegar sign]).
- Alterations in the skin (e.g., a hyperpigmented streak appearing below the umbilicus [linea nigra] and a reddish hyperpigmentation over the bridge of the nose and cheeks [chloasma]) (Figure 4-3).
- Pregnancy tests are an accurate marker for pregnancy and use urine (qualitative) or serum (quantitative) to check for β-human chorionic gonadotropin (HCG).
- Urine tests are generally positive around the time of the first missed period. β-HCG concentrations in the range of 25 to 50 mIU/mL are detectable in qualitative urine samples.
- Home pregnancy test kits detect β-HCG in the urine. β-HCG is detectable within 1 to 2 weeks after fertilization, but a pregnancy cannot be detected prior to implantation. The highest sensitivity (97%) of home pregnancy tests is at 1 week after the first day of the missed period.
- Serum pregnancy tests detect β-HCG at levels as low as 10 to 15 mIU/mL and mean levels closely correspond with gestational age during the first trimester. In healthy gestations, β-HCG levels double every 1.4 to 2 days, increasing exponentially until the fetus is 8 to 10 weeks old. Levels then decline somewhat and remain steady throughout the pregnancy. A minimum increase of 66% is expected every 48 hours. An appropriate rise in β-HCG levels on two quantitative (serum) pregnancy tests drawn 48 hours apart is reassuring for normal pregnancy development.
- Urine tests are generally positive around the time of the first missed period. β-HCG concentrations in the range of 25 to 50 mIU/mL are detectable in qualitative urine samples.
- Transvaginal ultrasound may be used to confirm and date a pregnancy. Sonographic landmarks like the gestational sac and fetal pole correlate highly with β-HCG levels.
- The gestational sac is generally seen when the pregnancy is 4.5 to 5 weeks along and the β-HCG level is greater than 1000 mIU/mL.
- The double decidual sign is a thick, hyperechoic (white) ring that surrounds the gestational sac. The yolk sac is the early nourishment for the embryo, seen at 6 weeks when β-HCG levels are greater than 2500 mIU/mL.
- The fetal pole is seen at 7 weeks gestation with β-HCG levels more than 5000 mIU/mL.
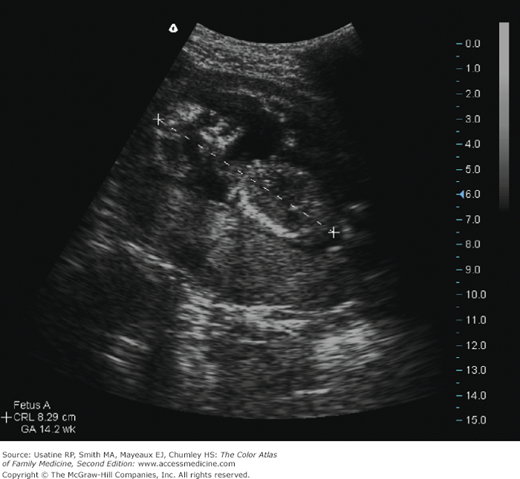
- Ultrasound measurements of the gestational sac and the crown to rump length (Figure 4-4) of the fetus are a very accurate means of establishing the EDD. First trimester transvaginal ultrasound confirms gestational age within ± 7 days.
- The gestational sac is generally seen when the pregnancy is 4.5 to 5 weeks along and the β-HCG level is greater than 1000 mIU/mL.
Differential Diagnosis
The differential diagnosis of pregnancy includes several gynecologic and nongynecologic conditions. Conditions presenting with an enlarged uterus or abdominal mass include the following:
- Uterine leiomyomas—benign tumors arising from uterine smooth muscle cells. Although most women with symptomatic leiomyomas are in the age range of 30 to 40 years, tumors are occasionally found in adolescents. Myomas occur as single or multiple tumors and range in size from microscopic to large masses. A 20-cm myoma often mimics pregnancy with increased abdominal girth and fullness, but can be distinguished on ultrasound.
- Large adnexal masses and tuboovarian abscesses (TOAs)—The bimanual examination often distinguishes between an adnexal mass and an enlarged uterus. TOA is associated with cervical motion tenderness and abdominal pain. Both conditions can be further evaluated by transvaginal ultrasonography.