Post-Chemotherapy Histiocyte-rich Pseudotumor of Spleen
Roberto N. Miranda, MD
Key Facts
Terminology
Residual splenic mass after chemotherapy composed of viable nonneoplastic cells and necrotic neoplastic cells
Etiology/Pathogenesis
Chemotherapy is toxic to neoplastic cells in spleen
Tumor necrosis releases chemotactic substances
Circulating monocytes are attracted and recruited to site of necrosis and become histiocytes
Clinical Issues
Residual masses after successful chemotherapy are rarely diagnosed in spleen
More common in patients with bulky tumors
In lymphoma patients, post-chemotherapy histiocyte-rich pseudotumors can
Revert to normal upon follow-up for > 1 year in ˜ 50%
Relapse in about 20% of those with residual masses
Image Findings
FDG-PET is considered one of the most helpful noninvasive imaging techniques
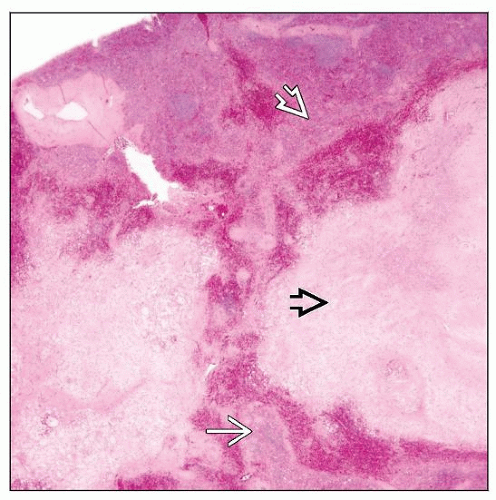
Microscopic Pathology
Nonviable tumor cells usually appear as cell ghosts
Many lipid-laden histiocytes; other inflammatory cells common
Top Differential Diagnoses
Residual viable tumor associated with necrosis
Storage diseases
Splenic inflammatory pseudotumor
TERMINOLOGY
Synonyms
Xanthomatous pseudotumor
Benign histiocytic proliferation with xanthomatous changes
Definitions
Residual splenic mass after chemotherapy composed of viable nonneoplastic cells and necrotic neoplastic cells
Similar masses can occur in other sites
ETIOLOGY/PATHOGENESIS
Chemotherapy-induced Tumor Necrosis
Sensitive tumors usually resolve after effective chemotherapy
However, large or bulky masses may persist after chemotherapy; more frequent with
Hodgkin lymphoma
Aggressive non-Hodgkin lymphomas
Metastatic carcinomas
Pediatric malignancies of primitive cells
Pathogenesis
Presumably, toxic effects of therapy kill neoplastic cells, which then elicits tissue reaction
Toxic effects of normal tissue stroma also may occur
Tumor necrosis releases chemotactic substances
Circulating monocytes are attracted and recruited to site of necrosis and become histiocytes
Role of lipid-accumulating macrophages in the pathogenic process is complex
There is transcription of genes associated with M2 activation
Mannose receptor/CD206
Scavenger receptor/CD163
Chemokine CCL18
Anti-inflammatory cytokine IL-10
CLINICAL ISSUES
Site
Spleen is focus of this chapter
Involved by tumor before therapy
Occasionally splenic mass is detected after chemotherapy
Rare site of post-chemotherapy histiocyte-rich pseudotumor
Other anatomic sites also can be involved: Mediastinum, lymph nodes, gastrointestinal tract
Presentation
Wide age range, in accordance with type of lymphoma and carcinoma
Variable time of follow-up depending on clinical assessment
Usually 1-6 months after completion of therapy
Splenic mass can be asymptomatic or associated with pain
Persistent mass after chemotherapy usually prompts suspicion of recurrent malignancy
Clinical or radiologic evidence of residual mass used to prompt “2nd look” surgery
Highly sensitive CT scans can detect smaller lesions of unknown clinical significance
PET scans can show high uptake
Post-therapy, splenic mass can be of similar size or larger than viable tumor mass before therapy
In general, the larger the size of residual mass, the higher the likelihood of residual viable cancer
Residual masses > 3 cm have greater chance of harboring viable tumor
Post-chemotherapy evaluation has clinical relevance
Hodgkin lymphoma
Assessment of response to chemotherapy may lead to further chemotherapy or radiation therapy
Nonseminomatous germ cell tumors with persistent lymphadenopathy (> 1 cm)
Revealed 2% residual viable cancer, 62% teratoma, and 36% necrosis; 4% had recurrence elsewhere
Resection is needed for better outcome in cases of teratoma or residual cancer
Wilms tumor
Post-chemotherapy complete tumor necrosis is considered as “low risk” in Wilms tumor
If tumor is stage I, may not require further chemotherapy
Residual masses can occur in ˜ 60% of patients after chemotherapy for lymphomas
More common in patients with bulky tumors
Symptoms are variable depending on site of involvement
Smaller, asymptomatic lesions may go undetected
Natural History
Related to underlying malignant neoplasm, including recurrences
Post-chemotherapy masses in lymphoma patients can
Revert to normal upon follow-up for > 1 year (˜ 50%)
Lead to sclerosis, fibrous scars, or calcification after longer periods of follow-up
Relapse in about 20% of those with residual masses
Mass is smaller or remains stable after chemotherapy has been completed
Occasionally splenic masses are 1st detected following chemotherapy for disease elsewhere
Splenic mass inapparent prior to therapy and resultant development of pseudotumor
Treatment
Observation or follow-up only
If imaging studies show evidence of progression, then resection, further chemotherapy, or radiotherapy may be indicated
Overdiagnosis of malignancy may lead to unnecessary additional therapy
Prognosis
Long-term prognosis related to underlying malignancy
Discovery of residual mass in mediastinum of Hodgkin lymphoma patients after chemotherapy correlates with higher 5-year relapse rate
2nd-line regimens (salvage therapy) are becoming more successful when residual disease is detected
IMAGE FINDINGS
MR Findings
Considered poorly sensitive for staging and follow-up of lymphoma patients
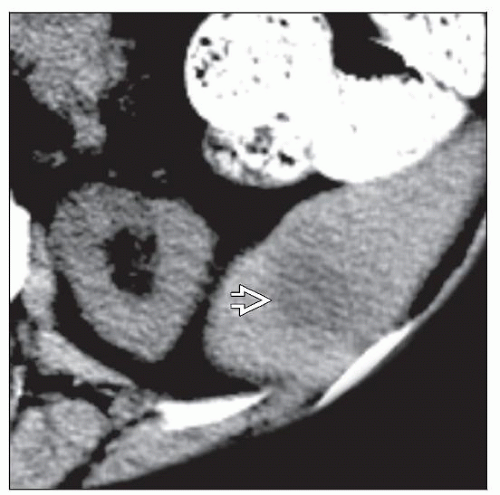
CT Findings
Sensitive technique to diagnose and monitor therapy
Advantage of being noninvasive and accurately determines extent of disease
Eliminates need for lymphangiography and staging laparotomy for Hodgkin lymphoma
In untreated lymphoma patients, any mass or lymph nodes > 1.5 cm is considered active disease
CT diagnosis of residual disease may lead to further chemotherapy, change of drug regimens, or radiotherapy
CT is considered nonspecific to assess tumor viability in patients who received chemotherapy
F18 Fluorodeoxyglucose (FDG) Positron Emission Tomography (PET)
Considered one of the most helpful noninvasive imaging techniques
Based on increased glucose metabolism of tumor cells
FDG is taken up by cell, but not metabolized, and it is retained intracellularly
Hodgkin lymphoma and aggressive non-Hodgkin lymphomas are generally FDG avid
Suggested that FDG PET is more sensitive for B-cell rather than T-cell lymphoma
Indolent non-Hodgkin lymphomas show variable FDG avidity
Advantageous over CT scan in assessing stage and detection of residual disease or early tumor relapse
Assessment of metabolic activity of cells in mass can predict tumor viability (high standardized uptake value [SUV])
Nonmetabolically active pseudotumors predict nonviable tumor and may prevent splenectomy
Approximately 10-30% false-positive rate as determined by concomitant biopsies
Refining may be required for cases with higher SUV values
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree