4 Poisoning
Acute poisoning accounts for 10–20% of acute medical admissions in the UK. There is wide geographical variation in the substances involved in poisoning. In the UK, paracetamol poisoning is common, but it accounts for only 7% of overdoses in the USA. Poisoning with tricyclic antidepressants (TCAs), selective serotonin re-uptake inhibitors (SSRIs) and drugs of misuse is very common in the UK and USA. In South-east Asia, pesticide ingestion is endemic, and constitutes the most common cause of death by poisoning.
GENERAL APPROACH TO THE POISONED PATIENT
The diagnosis of poisoning is usually apparent from the history. Occasionally, the ingested substance is unknown or patients deliberately mislead doctors (e.g. drug misusers). Full details of the type of substance, quantity and timing of ingestion should be sought. Remaining pills or empty packets may help to corroborate the substance taken. Commercially available databases (e.g. TICTAC®; http://tictac.vhn.net/home/) can be used to identify unlabelled pills from their visual appearance. Establishing the source of the drug (i.e. over the counter/prescription/belonging to a relative) is important in the prevention of future poisoning.
Ask the patient why the overdose was taken and take time to listen to the explanation. Reasons often include relationship difficulties, work- or school-related difficulties, drug addiction, psychiatric illness or bereavement. Details of the past medical history, particularly a history of asthma, jaundice, drug misuse, head injury, epilepsy, cardiovascular problems, previous psychiatric illness and self-harm, should be taken. It is also important to ask about allergies and alcohol history.
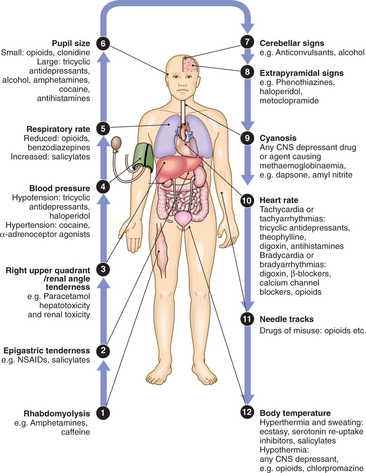
CLINICAL EXAMINATION OF THE POISONED PATIENT
CLINICAL FEATURES (p. 34)
PSYCHIATRIC ASSESSMENT
To determine appropriate placement and supervision for a patient, an initial assessment of suicidal intent must be made. Suicide attempts were once much more common in women than in men but now the ratios are more equal. Risk factors for suicide are shown in Box 4.1.
MANAGEMENT OF THE POISONED PATIENT
Most patients admitted with poisoning require only general care. Up-to-date information on diagnosis and management of overdoses of specific substances can be found on TOXBASE® (www.toxbase.org). Eye or skin contamination should be treated with appropriate washing or irrigation. Only patients who have ingested significant overdoses need further measures to prevent absorption or increase elimination:
In the seriously poisoned patient, meticulous supportive care, including the treatment of seizures, coma and cardiovascular complications, along with ventilatory support where required, is critical to good outcome. Despite popular misconceptions, specific antidotes are only available for a small number of poisons (Box 4.2).
4.2 ANTIDOTES AVAILABLE FOR THE TREATMENT OF SPECIFIC POISONINGS ![]()
| Poison | Antidote |
|---|---|
| Anticoagulants (e.g. warfarin) | Vitamin K, fresh frozen plasma |
| β-adrenoceptor antagonists (β-blockers) | I.v. glucagon, adrenaline (epinephrine) |
| Calcium channel blockers | Calcium gluconate, calcium chloride, glucagon |
| Cyanide | Oxygen, dicobalt edetate, nitrites, sodium thiosulphate, hydroxocobalamin |
| Ethylene glycol/methanol | Ethanol, 4-methylpyrazole |
| Lead | DMSA, DMPS, disodium calcium edetate |
| Mercury | DMPS |
| Iron salts | Desferrioxamine |
| Opioids | Naloxone |
| Organophosphorus insecticides, nerve agents | Atropine, oximes (pralidoxime, obidoxime salts, HI-6, HLo-7) |
| Paracetamol | N-acetylcysteine, methionine |
| Cardiac glycosides, e.g. digoxin | Digoxin-specific antibody fragments (Fab) |
POISONING BY SPECIFIC PHARMACEUTICAL AGENTS
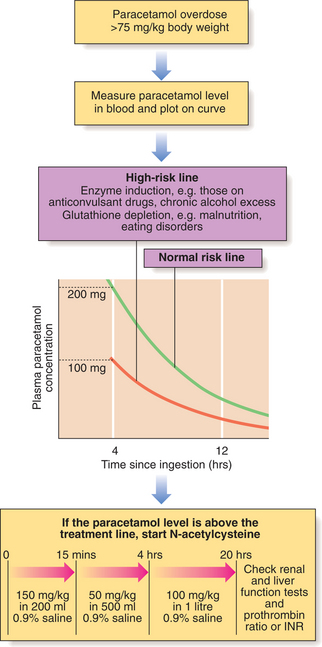
PARACETAMOL
This causes hepatic damage in overdose and can occasionally cause renal failure. The antidote of choice is i.v. N-acetylcysteine (NAC), which provides complete protection against toxicity if given <10 hrs after overdose (Fig. 4.1). A patient presenting >8 hrs after ingestion should have immediate NAC administration, which can later be stopped if the paracetamol level is below the treatment line. If a patient presents >15 hrs after ingestion, LFTs, PTR (or INR) and renal function tests should be performed, the antidote started, and a poisons information centre or local liver unit contacted for advice. Liver transplantation should be considered in individuals who develop acute liver failure due to paracetamol poisoning. If multiple ingestions of paracetamol have taken place over several hours or days (a staggered overdose), plasma paracetamol concentration will be uninterpretable. Such patients should be given NAC if the paracetamol dose exceeds 150 mg/kg body weight in any one 24-hr period (75 mg/kg in ‘high-risk groups’).
CARDIOTOXIC DRUGS
The main categories are β-blockers, digoxin, calcium channel blockers and TCAs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree