Plasmablastic Lymphoma Arising in HHV8+ Multicentric Castleman Disease
L Jeffrey Medeiros, MD
Key Facts
Terminology
PBL-MCD is a monoclonal proliferation of HHV8(+) plasmablasts that express IgMλ and arise in MCD
Etiology/Pathogenesis
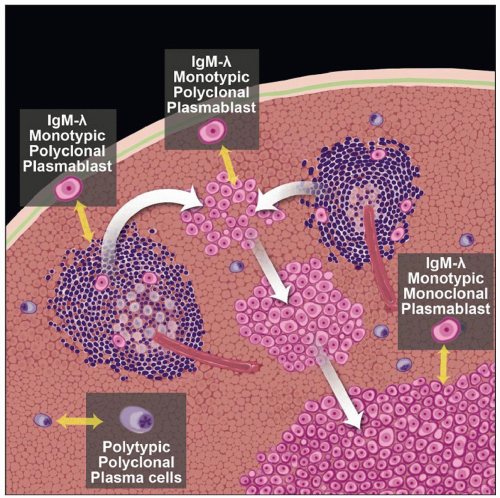
HHV8 initially infects singly scattered plasmablasts in mantle zones of follicles
HHV8(+) plasmablasts expand to form so-called microlymphomas
HHV8(+) “microlymphomas” expand into histologically overt lymphoma
Most patients with PBL-MCD have profound immunosuppression
Clinical Issues
Lymph nodes, spleen
Leukemic involvement as part of a terminal phase
Poor; survival often < 1 year
Microscopic Pathology
Plasmablastic lymphoma
Sheets of plasmablasts (or immunoblasts)
Mitotic figures common
Ancillary Tests
HHV8(+), IgM(+), λ(+)
CD45/LCA(+/-), CD20(-/+), CD79a(-), EBV(-)
Single-cell PCR studies show monoclonal IgH rearrangements in PBL
Top Differential Diagnoses
Primary effusion lymphoma (PEL)
Extracavitary PEL
HHV8(+) germinotropic lymphoproliferative disorder
TERMINOLOGY
Abbreviations
Plasmablastic lymphoma (PBL) arising in HHV8(+) multicentric Castleman disease (MCD)
Synonyms
Large B-cell lymphoma arising in HHV8(+) MCD
Terminology of World Health Organization Classification, 2008
HHV8(+) plasmablastic lymphoma
KSHV(+) plasmablastic lymphoma
Definitions
PBL-MCD is a monoclonal proliferation of HHV8(+) plasmablasts that express IgMλ and arise in MCD
ETIOLOGY/PATHOGENESIS
Infectious Agents
Human herpes virus 8 (HHV8) is involved in pathogenesis
a.k.a. Kaposi sarcoma herpes virus (KSHV)
HHV8 initially infects singly scattered plasmablasts in mantle zones of follicles
These plasmablasts are naive B cells that express IgM
Plasmablasts express λ light chain but are polyclonal at molecular level
Plasmablasts lack evidence of immunoglobulin (Ig) somatic hypermutation
HHV8 encodes at least 10 homologues of cellular genes
Inhibit cell apoptosis, promote cell proliferation, and drive infected B cells to differentiate into plasmablasts
HHV8 encodes for viral homologue of IL-6, which is thought to induce many features of MCD
HHV8(+) plasmablasts expand to form so-called microlymphomas
Polyclonal or monoclonal associated with HHV8(-) polyclonal cells
HHV8(+) “microlymphomas” expand into histologically overt lymphoma
Cells in overt lymphoma are monoclonal
Analysis of HHV8 episomes shows virus is monoclonal
Indicates HHV8 is present prior to clonal expansion
Immunosuppression
Most patients with PBL-MCD have profound immunosuppression
HIV infection is very common
Patients with MCD and HIV have 15x increased risk of non-Hodgkin lymphoma
CLINICAL ISSUES
Epidemiology
Incidence
Rare
Age
Depends in part on presence or absence of HIV infection
HIV(+): Age mirrors that of HIV(+) patients in general
HIV(-): Older patients
Ethnicity
In HIV(-) patients, PBL-MCD is more common in regions endemic for HHV8 infection
Mediterranean basin, Africa
Site
Lymph nodes, spleen
Leukemic involvement as part of a terminal phase
Extranodal sites not (or rarely) involved
Presentation
Evidence of profound immunosuppression
Lymphadenopathy; ± splenomegaly
± Kaposi sarcoma
Treatment
No consensus
Therapeutic choices often limited by marked immunosuppression
Prognosis
Poor; survival often < 1 year
IMAGE FINDINGS
General Features
Lymphadenopathy and splenomegaly are most common
MICROSCOPIC PATHOLOGY
Histologic Features
Multicentric Castleman disease is characterized by
Hyaline-vascular &/or lymphocyte-depleted follicles
Scattered plasmablasts/immunoblasts in mantle zones of follicles
Marked interfollicular plasmacytosis without atypia
Vascular proliferation
Microlymphomas
Small clusters of atypical cells arising in mantle zone ± surrounding germinal centers
Large cells with plasmablastic or (less likely) immunoblastic features
Abundant cytoplasm, vesicular nucleus, prominent nucleoli
Plasmablastic lymphoma
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree