Plasmablastic Lymphoma
Francisco Vega, MD, PhD
Key Facts
Terminology
Diffuse neoplasm with immunoblastic or plasmablastic features and plasma cell immunophenotype
Aggressive clinical course
Poor prognosis
Etiology/Pathogenesis
Associated with immunodeficiency
HIV infection most common
Clinical Issues
Frequently originates in mucosa of oral cavity
Nonoral cases also occur
Microscopic Pathology
Large neoplastic cells with variable degree of immunoblastic or plasmablastic features
“Starry sky” pattern frequent
High mitotic and apoptotic rates
Ancillary Tests
Pan-B-cell antigens: Weak or absent
Plasma cell markers(+)
EBER(+), HHV8(−)
Monoclonal IgH gene rearrangements
High proliferation index (Ki-67)
Top Differential Diagnoses
Diffuse large B-cell lymphoma, immunoblastic variant
Plasmablastic plasma cell myeloma
Multicentric Castleman disease, HHV8 positive
ALK(+) large B-cell lymphoma
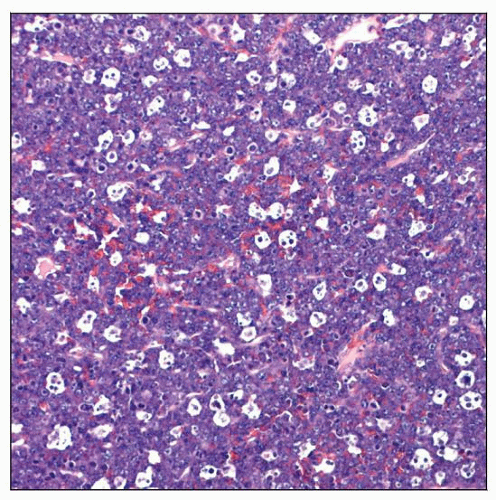 This case of plasmablastic lymphoma (PBL) is characterized by diffuse infiltrate of large atypical lymphoid cells with a “starry sky” pattern. |
TERMINOLOGY
Abbreviations
Plasmablastic lymphoma (PBL)
Definitions
PBL was initially described as rare variant of diffuse large B-cell lymphoma (DLBCL) involving oral cavity
15 of 16 patients were immunodeficient as a result of human immunodeficiency virus (HIV) infection
PBL is currently defined as diffuse proliferation of large neoplastic cells
Immunoblastic or plasmablastic cytologic features
Plasma cell immunophenotype: CD38(+), CD138(+), CD20(−)
ETIOLOGY/PATHOGENESIS
Infectious Agents
EBV positive
Strongly associated with HIV infection
Has been reported in patients with immunodeficiency due to other causes
Example: Post-transplantation
CLINICAL ISSUES
Epidemiology
Incidence
Unknown
Frequency: PBL represents < 1% of all non-Hodgkin lymphomas
Age
Depends on clinical setting
HIV(+) patients: Median age = 40 years
HIV(−) patients: Children or elderly
Gender
Male predominance: 7:1
Related to HIV(+) population affected
Presentation
PBL most often originates in mucosal extranodal sites
2 general groups: Oral and nonoral sites
Rapidly growing and often painful mass
Oral cavity is most common site
90% of patients are HIV(+)
Patients have very low CD4(+) counts
Mean duration of HIV(+) prior to PBL: 5 years
60% have localized disease (stage I) at diagnosis
PBL frequently arises near mucosa
Often involves gingiva
Frequently infiltrates adjacent bone
Nonoral type PBL
Less frequently HIV(+)
60% are disseminated disease (stage IV) at diagnosis
Most common nonoral sites
Maxillary sinus, nasopharynx, gastrointestinal tract
Less common nonoral sites
Orbit, skin, lung, gastrointestinal tract, soft tissues
Rare sites of PBL (case reports)
Mediastinum, vulva, bone marrow
PBL uncommonly involves lymph nodes
PBL can widely disseminate during course of disease
International prognostic Index (IPI): Usually intermediate or high score
Some cases are reported in patients with history of myeloma or lymphoma
Better considered as plasmablastic transformation of underlying neoplasm
Treatment
Prognosis
Poor prognosis
Most patients die within 1st year after diagnosis
In large review, prognosis did not correlate with
Age, sex, CD4(+) count, HIV load
Stage, anatomic site of PBL, EBV status
Use of CHOP chemotherapy
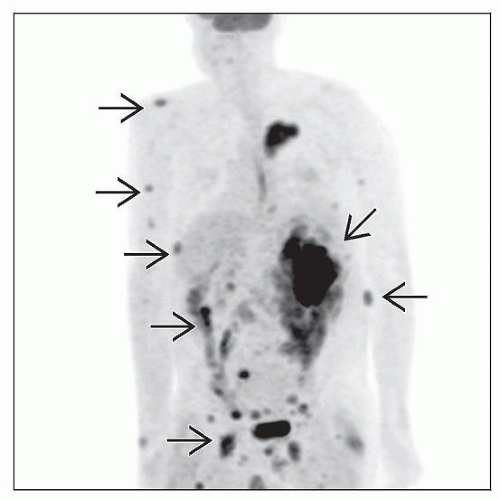
IMAGE FINDINGS
Radiographic Findings
PBL is PET scan positive
PET or CT scan can show widespread bone involvement
MICROSCOPIC PATHOLOGY
Histologic Features
Diffuse growth pattern
Frequent “starry sky” pattern with tingible body macrophages
Apoptotic bodies and mitoses are usually numerous
Confluent areas of necrosis are common
Cytologic Features
Monotonous proliferation of large neoplastic cells in histologic sections
More cytologic variability in smear/imprint preparations
PBL cases can exhibit cytologic spectrum
Immunoblastic
Cells have prominent central nucleoli
More common in oral cavity and in HIV(+) patients
Plasmablastic
Cells have more abundant cytoplasm and eccentrically located nuclei
More common in nonoral sites
Binucleation or multinucleation is common in PBL
Cytoplasm of PBL cells is usually deeply basophilic
Dutcher and Russell bodies are usually absent in PBL
ANCILLARY TESTS
Immunohistochemistry
Immunophenotype is essential to establish diagnosis of PBL
Common pan-B-cell markers commonly absent
CD20, CD22, and pax-5
Weak expression reported in small subset of cases
CD79a is more often positive; also often weak intensity
Strong positivity for plasma cell-associated markers
IRF-4/MUM1(+), CD38(+), CD138/syndecan-1(+), VS38/p63(+)
PRMD1/BLIMP1(+), XBP1(+)
Ki-67 is high: > 70% in most cases
Monotypic cytoplasmic light chain positive in 50-70% of cases
EMA is often positive; CD30(+) in subset
Aberrant expression of T-cell markers in some cases
CD3, CD4, CD43, CD7
Germinal center B-cell antigens positive in subset of PBL
Bcl-6 uncommon; CD10 (+ in ˜ 50%)
CD56 can be positive in cases with plasmablastic cytologic features
Must exclude plasma cell myeloma
Bcl-2 is usually negative
CD45/LCA is negative or weakly positive in subset of cases
ALK1(−), CD117(−), Cyclin-D1(−)
HHV8(−)
EBV-LMP 1 and 2 are not expressed
Consistent with restricted latency
In contrast to AIDS-related immunoblastic lymphomas that usually express EBV-LMP 1
No significant differences in frequency of expression of any immunohistochemical marker between PBL and plasmablastic plasma cell myeloma
Cytogenetics
t(8;14)(q24;q32) or MYC-IgH fusion identified in subset of PBL
HIV(+) patients
In Situ Hybridization
EBV small encoded RNA (EBER) is positive in ˜ 75% of cases
EBER useful for distinguishing PBL from plasmablastic plasma cell myeloma (EBER[-])
PCR
Monoclonal IgH gene rearrangements
T-cell receptor genes usually in germline configuration
Single case reports showing both IgH and TCR gene rearrangements
IgH genes commonly show somatic mutations of IgH variable regions
DIFFERENTIAL DIAGNOSIS
Diffuse Large B-cell Lymphoma, Not Otherwise Specified (DLBCL)
DLBCL often has centroblastic cytologic features
Plasmacytoid differentiation is uncommon
Immunophenotype of DLBCL is distinct from PBL
CD19(+), CD20(+), CD22(+), pax-5(+)
CD45/LCA is usually positive
Large subset is strongly positive for CD10 &/or Bcl-6
Diffuse Large B-cell Lymphoma, Immunoblastic Variant (DLBCL-IB)
Morphologic overlap between DLBCL-IB and PBL
Immunophenotype is needed to make this distinction
DLBCL-IB is usually CD20(+) &/or pax-5(+)
CD45/LCA often positive
CD10(+/−), Bcl-6(+/−)
CD4(+) is extremely rare in DLBCL-IB
By contrast, PBL is CD20(−), CD38(+), CD138/syndecan-1(+), and VS38/p63(+)
CD4 or CD56 can be positive
Plasma Cell Myeloma (PCM)
Clinically important to distinguish between PCM and PBL
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree