B. Plasma/fresh frozen plasma contains multiple factors for hemostasis and has increasingly been considered a critical component (see Fig. 31-1).
C. Platelet Administration
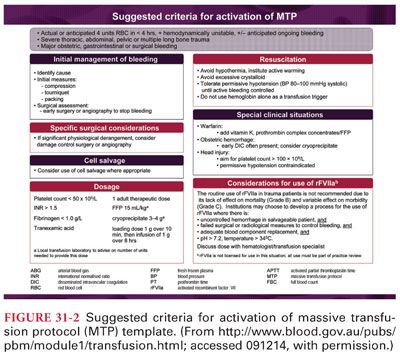
1. Following traumatic injury or significant postoperative bleeding, the critical platelet count for transfusion is often based on consensus therapy rather than true objective data. Although a count of 50,000 or more is recommended, the threshold for administration of platelets, especially in cases of dilutional coagulopathy, remains unclear as do the ideal ratio of platelets to other blood components.
2. Most protocols attempt to develop a strategy that mimics whole blood replacement with RBC:plasma/FFP:platelets at a 1:1:1 ratio with massive bleeding.
3. Assessing platelet function in the bleeding patient is not possible; therefore, empiric platelet administration is often undertaken.
D. Antifibrinolytic Agents
1. Because of the critical role of fibrinolysis with severe bleeding and trauma, the antifibrinolytic agent tranexamic acid is increasingly used as a therapeutic strategy.
2. Inhibiting fibrinolysis during acute bleeding has many beneficial effects including preserving initial clot formation at a bleeding site that may otherwise be broken down.
VI. Postpartum hemorrhage is an important cause of life-threatening hemorrhage and continues to be a major cause of maternal mortality. As in all life-threatening bleeding, a treatment algorithm that includes a massive transfusion protocol is important.
VII. Multimodal Resuscitation: Damage Control Resuscitation
A. Managing life-threatening and uncontrolled bleeding is a clinical problem that can occur following traumatic injury, during major surgical procedures, and following delivery.
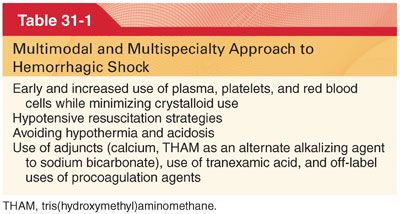
B. A multimodal and multispecialty approach has evolved for the optimal resuscitative approach to hemorrhagic shock (Table 31-1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


