Patient Story
A 50-year-old woman presented to the clinic with an abrupt onset of an intensely pruritic rash that extended over the dorsal aspect of both arms (Figure 199-1). The patient notes no new medicines and no recent exposures to any new chemicals. She acknowledged recent time spent outside in the sun. The plaques were photodistributed, with sparing of her watch area. A clinical diagnosis of polymorphous light eruption (PMLE) was made, and the patient was started on oral antihistamines and topical steroids. It was recommended that she minimize her sun exposure.
Figure 199-1
Polymorphous light eruption noted over dorsum of left forearm. Note absence of the lesion where the patient had been wearing her watch. (From Wenner C, Lee A. A bright red pruritic rash on the forearms. J Fam Pract. 2007;56(8):627-629. Reproduced with permission from Frontline Medical Communications.)
Introduction
Photosensitivity is an abnormal skin response to ultraviolet light that occurs on sun-exposed areas of the skin. There are three common types of photodermatitis:
- PMLE (Figures 199-1 and 199-2).
- Phototoxic eruptions (Figures 199-3, 199-4, 199-5, 199-6, and 199-7).
- Photoallergic eruptions (Figure 199-8). Table 199-1 compares key characteristics of phototoxic and photoallergic reactions.
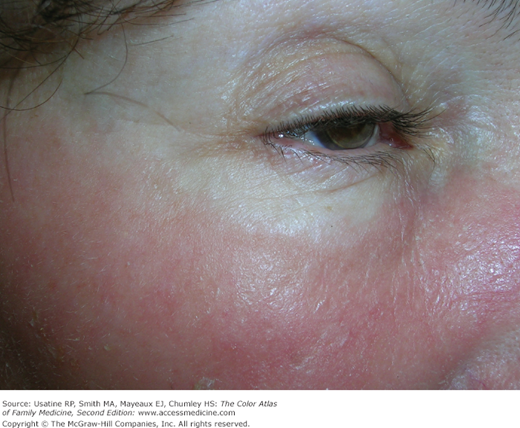
Figure 199-6
Phytophotodermatitis in a woman, caused by lime juice and sun exposure on the beach. Note the hand print of her fiancé who had been squeezing limes into their tropical drinks. This contact occurred when they posed for a photograph. (From Darby-Stewart AL, Edwards FD, Perry KJ. Hyperpigmentation and vesicles after beach vacation. Phytophotodermatitis. J Fam Pract. 2006;55(12):1050-1053. Reproduced with permission from Frontline Medical Communications.)
Figure 199-7
Phytophotodermatitis visible on the arm, trunk, and leg caused by lime juice and sun exposure on the beach. Note the hyperpigmentation that occurs in conjunction with the erythema. (From Darby-Stewart AL, Edwards FD, Perry KJ. Hyperpigmentation and vesicles after beach vacation. Phytophotodermatitis. J Fam Pract. 2006;55(12):1050-1053. Reproduced with permission from Frontline Medical Communications.)
Feature | Phototoxic Reaction | Photoallergic Reaction |
|---|---|---|
Incidence | High | Low |
Amount of agent required for photosensitivity | Large | Small |
Onset of reaction after exposure | Minutes to hours | 24 to 72 hours |
More than 1 exposure to agent required | No | Yes |
Examination findings | Exaggerated sunburn | Dermatitis |
Immunologically mediated | No | Yes |
UV light radiating from the sun may be categorized into UVA (wavelength 320 to 400 nm), UVB (290 to 320 nm), and UVC (200 to 290 nm). UVC is completely absorbed by the earth’s ozone layer and thus does not play a role in photosensitivity. Photosensitivity may be induced by UVA, UVB, or visible light (400 to 760 nm). Longer wavelength light penetrates deeper into the skin. UVA penetrates through to the dermis, but UVB mainly penetrates and affects the epidermis.
Ultraviolet light has multiple effects on the skin. Notably, it causes DNA damage and has immunosuppressive effects on skin inflammatory cells increasing the risk of carcinogenesis. In patients with photosensitivity, it elicits an inflammatory response in the skin, leading to the development of a photodermatosis.
Epidemiology
- PMLE (Figures 199-1 and 199-2) may affect up to 10% of the population, with a predilection for females.1 The prevalence increases in northern latitudes. Onset typically occurs within the first three decades of life, but may appear spontaneously at any age.
- The incidence of drug- and plant-induced phototoxic reactions in the United States is unknown. Phototoxic reactions are much more common than photoallergic reactions.
Etiology and Pathophysiology
PMLE is an idiopathic, delayed-type hypersensitivity reaction to UVA light and, to a lesser extent, UVB light (Figures 199-1 and 199-2). PMLE is the most common photoeruption encountered in clinical practice. The reaction will remit spontaneously with time and absence of sun exposure, but occasionally it will last as long as sun exposure occurs. PMLE usually begins in the first three decades of life and occurs more commonly in women. The rash develops within hours to days after exposure to sunlight and lasts for several days to a week.
There is a broad range of degrees of photosensitivity with PMLE. Extremely sensitive individuals can tolerate only minutes of exposure, whereas many people have a low sensitivity and require prolonged exposure to sunlight before developing a reaction. It is a recurrent condition that persists for many years in most patients.2
Phototoxic reactions are the most common drug-induced photoeruptions (Figures 199-3, 199-4, 199-5, 199-6, and 199-7). They are caused by absorption of ultraviolet rays by the causative drug, which releases energy and damages cell membranes, or, in the case of psoralens, DNA. The drugs that most frequently cause phototoxic reactions are NSAIDs, quinolones, tetracyclines, amiodarone, and the phenothiazines3 (Table 199-2). Most of these drugs have at least one resonating double bond or an aromatic ring that can absorb radiant energy. Most compounds are activated by wavelengths within the UVA (320 to 400 nm) range, although some compounds have a peak absorption within the UVB or visible range.
Class | Medication |
|---|---|
Antibiotics | Tetracyclines Fluoroquinolones Sulfonamides Griseofulvin |
NSAIDs | Ketoprofen Ibuprofen Naproxen |
Diuretics | Furosemide Hydrochlorothiazide |
Retinoids |