1. COX-1 is constitutively expressed and catalyzes the production of prostaglandins that are involved in numerous physiologic functions (maintenance of normal renal function in the kidneys, mucosal protection in the gastrointestinal tract, production of proaggregatory thromboxane A2 in the platelets).
2. COX-2 expression can be induced by inflammatory mediators in many tissues and has a role in the mediation of pain, inflammation, and fever.
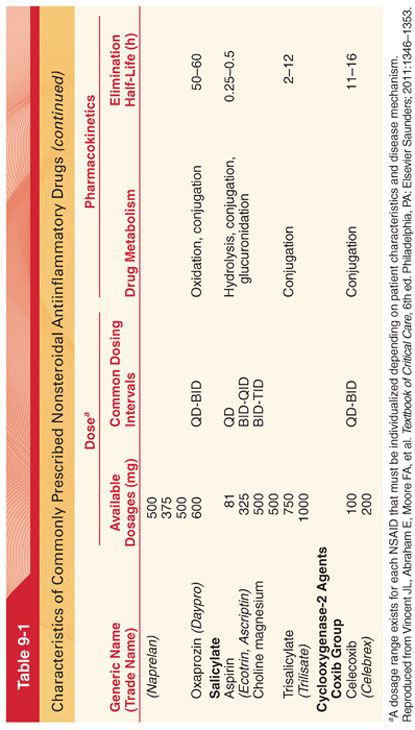
a. COX-2 selective inhibitors (known as the “coxibs”) have less gastrointestinal toxicity than nonselective NSAIDs. However, increased cardiovascular risk has been associated with the use of this class of drugs (celecoxib is the only COX-2 selective inhibitor available for clinical use).
b. Coxibs may be a safer alternative to NSAIDs (platelet dysfunction and gastrointestinal toxicity in the perioperative settings); benefits include improved quality of analgesia, reduced incidence of gastrointestinal side effects versus conventional NSAIDs, and no platelet inhibition.
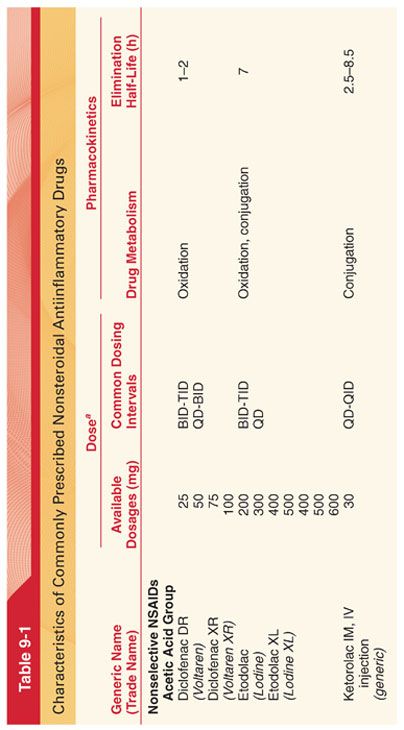
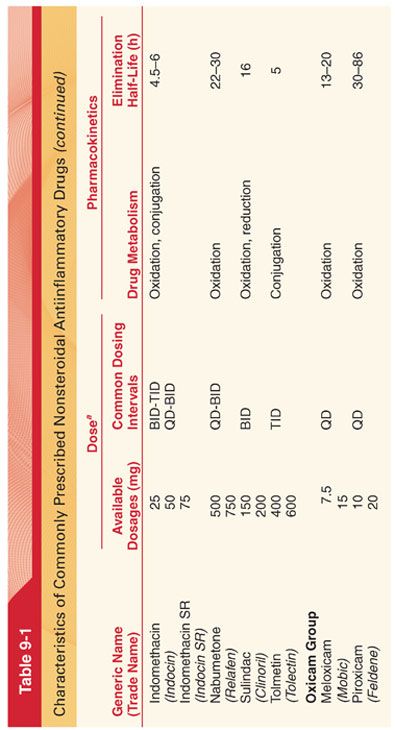
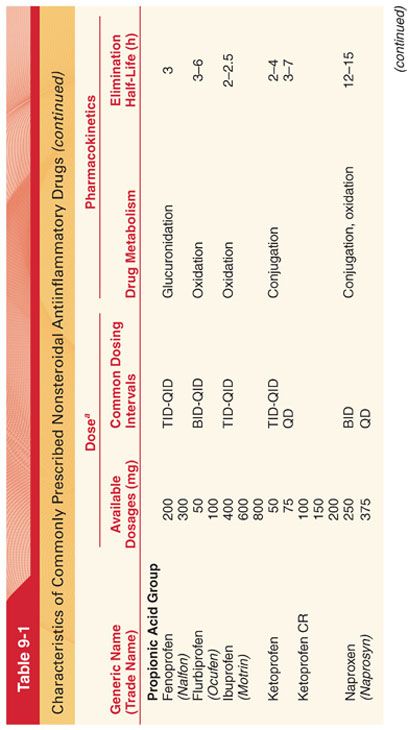
III. NSAIDS belong to a number of chemical families including acetic acids, oxicams, propionic acids, salicylates, fenamates, furanones, and coxibs (Table 9-1). All NSAIDs are weakly acidic chemical compounds and share similarities in pharmacokinetic properties. Gastrointestinal absorption of NSAIDs occurs rapidly, usually within 15 to 30 minutes. The liver metabolizes most NSAIDs, with subsequent excretion into urine or bile (reduced renal function prolongs NSAID half-life and the dose should be lowered proportionally in patients with impaired kidney function, and moderate to severe liver disease impairs NSAID metabolism, increasing the potential for toxicity).
A. Side Effects of NSAIDs (Table 9-2)
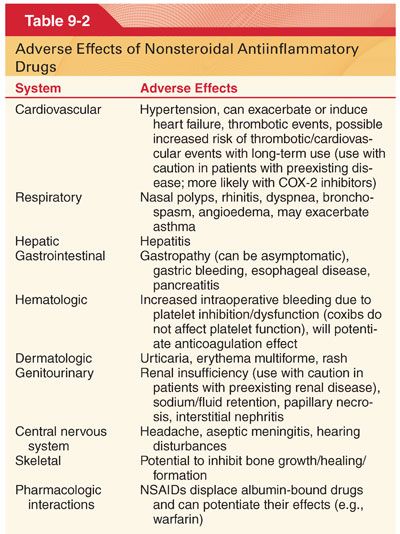
1. Platelet Function. NSAIDs and aspirin inhibit the activity of COX-1 (thromboxane production), but the COX-2 specific inhibitors have no effect on COX-1 and thus no effect on platelet function.
2. Gastrointestinal Side Effects. NSAIDs are associated with a spectrum of upper gastrointestinal complications, ranging from endoscopic ulcers in 10% to 30% of patients to serious ulcer complications in 1% to 2% of patients, including perforation and bleeding (patients with gastrointestinal risk factors should be treated with COX-2 selective agents or nonselective NSAIDs with gastrointestinal protective cotherapy).
3. Cardiovascular Side Effects. NSAIDs are associated with an increased risk of cardiovascular adverse events (myocardial infarction, heart failure, hypertension). COX inhibition is likely to disturb the balance between COX-2–mediated production of proaggregatory thromboxane in platelets and antiaggregatory prostaglandin I2 in endothelial cells.
a. A meta-analysis of randomized trials on nonselective NSAIDs found that high-dose ibuprofen and high-dose diclofenac were associated with a moderately increased risk of vascular events compared with placebo, similar to that observed with COX-2–selective agents.
b. The risks associated with naproxen, although they cannot be completely excluded, appeared to be substantially lower.
4. Renal Side Effects. The effects of the NSAIDs on renal function include changes in the excretion of sodium, changes in tubular function, potential for interstitial nephritis, and reversible renal failure due to alterations in filtration rate and renal plasma flow (prostaglandins and prostacyclins are important for maintenance of intrarenal blood flow and tubular transport). Avoiding perioperative use of NSAIDs in patients with hypovolemia from any cause is an important means of minimizing renal injury.
5. Pulmonary Side Effects
a. Many adverse reactions attributed to NSAIDs are due to inhibition of prostaglandin synthesis in local tissues (patients with allergic rhinitis, nasal polyposis, and asthma are at increased risk for anaphylaxis).
b. The use of selective COX-2 inhibitors as an alternative to aspirin and other NSAIDs has been suggested for patients with aspirin-exacerbated respiratory disease.
6. Hypersensitivity reactions to NSAIDs rarely occur, and they are more common in individuals with nasal polyps or asthma.
B. Drug–drug interactions with NSAID therapy may result from their pharmacodynamic or pharmacokinetic interactions.
1. Nonselective NSAIDs affect other antiplatelet agents via additive inhibition of platelet aggregation (result is an increased bleeding risk with the concomitant use of NSAIDs and other antiplatelet agents).
2. NSAIDs decrease lithium clearance and increase serum lithium concentrations by inhibiting renal prostaglandin production and altering intrarenal blood flow.
3. Concurrent administration of digoxin and NSAIDs can decrease renal clearance of digoxin, increase plasma drug concentration, and potentiate digoxin toxicity.
4. NSAIDs interact with anticonvulsant agents (phenytoin and valproic acid) by displacing the anticonvulsants from their protein-binding sites, which increases the free drug concentration.
IV. Acetaminophen (Tylenol) is a popular antipyretic and analgesic (little, if any, antiinflammatory action) found in many over-the-counter and prescription products.
A. Acetaminophen is the leading cause of acute liver failure in the United States, and nearly half of acetaminophen-associated cases are due to unintentional overdose.
1. Damage to the liver results from one of acetaminophen’s metabolites, N-acetyl-p-benzoquinoneimine (NAPQI). NAPQI leads to liver failure by depleting the liver’s natural antioxidant glutathione and directly damaging liver cells, leading to liver failure.
2. Treatment is aimed at removing the paracetamol from the body and replacing glutathione. Acetylcysteine is administered as an antidote and acts as a precursor for glutathione and can neutralize NAPQI directly.
B. Oral acetaminophen has excellent bioavailability. The conventional oral dose of acetaminophen is 325 to 650 mg every 4 to 6 hours; total daily doses should not exceed 4,000 mg.
C. Acetaminophen is the first-line analgesic in osteoarthritis and particularly valuable for patients in whom aspirin is not recommended.
D. An intravenous (IV) preparation of acetaminophen is currently available for clinical use.
V. Acetylsalicylic acid (Aspirin) is the oldest and most widely used medicinal compound in the world, acting as a general analgesic by blocking the action of the COX enzymes and thus prevents the production of prostaglandins (effectively treats headaches, back and muscle pain). Aspirin irreversibly inactivates COX, leading to prolonged inhibition of platelet aggregation.
A. Overdose
1. The mechanism of NSAID toxicity in overdose is related to both their acidic nature and their inhibition of prostaglandin production.
2. Symptoms include nausea, vomiting, abdominal pain, tinnitus, hearing impairment, and central nervous system (CNS) depression (see Table 9-2). With higher dose aspirin ingestion, metabolic acidosis, renal failure, CNS changes (agitation, confusion, coma), and hyperventilation with respiratory alkalosis due to stimulation of the respiratory center occurs. The presence of acidemia permits more salicylic acid to cross the blood–brain barrier.
3. Management should be directed at symptomatic support (no antidote available), prevention of further absorption, and correction of acid–base imbalance.
a. Appropriate hydration and activated charcoal should be considered within 1 hour after ingestion.
b. Urine alkalinization increases salicylate elimination.
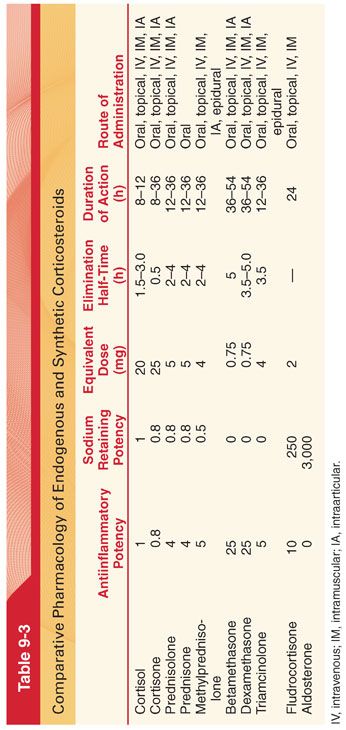
VI. Steroids (Tables 9-3 and 9-4)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


