Peripheral T-cell Lymphoma, Not Otherwise Specified
James M. You, MD, PhD
Key Facts
Clinical Issues
PTCL represents approximately 6.0% of all non-Hodgkin lymphomas
Mainly arises in middle-aged adults; rare in children
Advanced-stage disease with B symptoms
Poor prognosis with frequent relapses
Lymphadenopathy; extranodal sites often involved
Microscopic Pathology
Paracortical infiltrate or diffuse effacement of lymph node architecture
Wide cytological spectrum
Background inflammatory cells often numerous
± postcapillary venules in arborizing fashion
± high rates of proliferation and apoptosis
Ancillary Tests
Pan-T-cell antigens(+)
CD4(+) CD8(−) or CD4(−) CD8(+)
Aberrant T-cell immunophenotypes in ˜ 80% of cases
CD30 can be positive, exceptionally CD15(+)
± cytotoxic molecules
Monoclonal TCR gene rearrangements
No consistent chromosomal/molecular abnormality
Top Differential Diagnoses
Angioimmunoblastic T-cell lymphoma
Adult T-cell leukemia/lymphoma
Anaplastic large cell lymphoma
Classical Hodgkin lymphoma
T-cell/histiocyte-rich large B-cell lymphoma
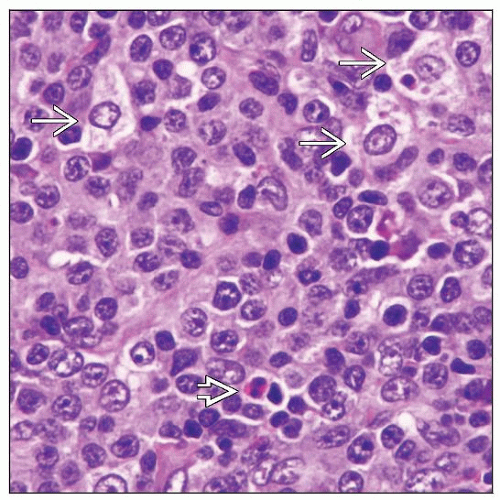
 Peripheral T-cell lymphoma (PTCL) involving lymph node. The neoplastic cells in this case show abundant clear cytoplasm. |
TERMINOLOGY
Abbreviations
Peripheral T-cell lymphoma, not otherwise specified (PTCL-NOS)
Synonyms
Peripheral T-cell lymphoma (PTCL)
Peripheral T-cell lymphomas, unspecified
Term used in 2001 World Health Organization (WHO) classification
Post-thymic T-cell lymphoma
Immunoblastic sarcoma of T-cell lineage
Definitions
Mature T-cell lymphomas that cannot be classified into specific T-cell categories
Heterogeneous group in current WHO classification
PTCL is, in part, diagnosis of exclusion
ETIOLOGY/PATHOGENESIS
Etiology and Pathogenesis
Evidence that aberrant T-cell signaling drives T-cell lymphoproliferation
The specific etiology of PTCL is unknown
Once etiology or pathogenesis of a subgroup is defined, this subset is likely to be reclassified
Cell of Origin
Activated mature T-lymphocyte, either CD4(+) or CD8(+)
CLINICAL ISSUES
Epidemiology
Incidence
PTCL represents approximately 6% of all non-Hodgkin lymphomas
˜ 50% of all NK/T-cell neoplasms
Age
Mainly arises in middle-aged adults; rare in children
Gender
Male to female ratio ˜ 2:1
Site
Lymph nodes are usually involved
Involvement of extranodal sites is common, including
Bone marrow, spleen, liver, lung, and skin
Presentation
Most patients have advanced-stage disease with B symptoms
Bulky disease in ˜ 10% of patients
Leukemic phase is rare at presentation
Cytokine-related paraneoplastic phenomena can occur, including
Pruritus &/or eosinophilia
Hemophagocytic syndrome
Prior to onset of PTCL, immune-mediated disorders can occur, including
Hashimoto thyroiditis, rheumatoid arthritis
Immune thrombocytopenic purpura
Laboratory Tests
Elevated serum lactate dehydrogenase (LDH) level is common
Treatment
Aggressive combination chemotherapy ± consolidation therapy
Induction combination chemotherapy regimens combine anthracycline with alkylating agent
Consolidation therapy
Hematopoietic stem cell transplantation
Radiation therapy
Treatment for refractory or relapsed PTCL
Prognosis
Overall response to therapy is poor with frequent relapses
5-year overall survival and failure-free survival (20-30%)
Poor prognosis has been associated with
High stage
High international prognostic index (IPI)
Features suggested but need to be confirmed
Epstein-Barr virus (EBV)(+)
Gene expression profile showing NF-κB dysregulation or high proliferation signature
Cytotoxic immunophenotype
Small subset of patients with localized disease and low IPI have better outcome
IMAGE FINDINGS
Radiographic Findings
Lymphadenopathy
FDG-PET is often positive
MICROSCOPIC PATHOLOGY
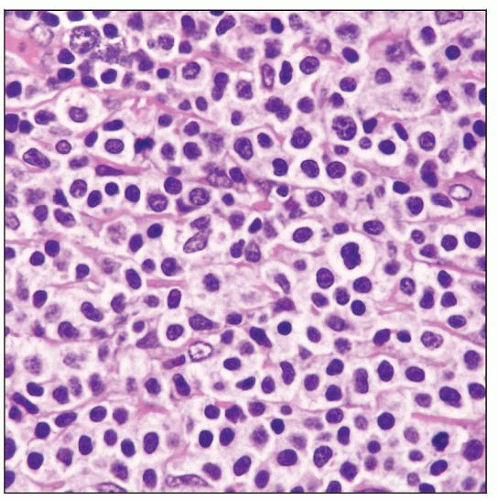
Histologic Features
Lymph node
Paracortical infiltrate or diffuse effacement of architecture
Proliferation of postcapillary venules in interweaving (arborizing) fashion can be present
High rates of proliferation and apoptosis
Background inflammatory cells usually present, including:
Eosinophils, plasma cells, small lymphocytes
Epithelioid histiocytes, large B cells
In subset of cases, there is preferential involvement of T-zones
In some cases, neoplasm is associated with fibrosis
Fibrous bands can compartmentalize neoplasm, simulating nodular pattern
Skin
PTCL commonly infiltrates dermis and subcutis; can produce nodules with central ulceration
Angiocentricity and adnexal involvement may be seen
Epidermotropism is rare
Spleen
Solitary or multiple fleshy nodules involving white pulp with colonization of periarteriolar sheath
Predominant infiltration of red pulp in some cases
Cytologic Features
Wide spectrum of neoplastic T-cells of small, intermediate, or large size
Numerous intermediate-sized &/or large cells, most common
Neoplastic cells have sparse or abundant cytoplasm
Clear, eosinophilic, or basophilic
Nuclei of neoplastic cells show wide spectrum
Vesicular, hyperchromatic, or pleomorphic
Multinucleated or Reed-Sternberg-like nuclei can occur
Morphologic Variants of PTCL
Lymphoepithelioid (Lennert lymphoma)
Diffuse replacement of lymph node architecture
Predominantly small lymphoid cells with slight nuclear irregularities
Confluent clusters of epithelioid histiocytes
Scattered, larger, more atypical cells, including occasional Reed-Sternberg-like cells (usually EBV[+])
Occasional admixed inflammatory cells, including eosinophils and plasma cells
Neoplastic cells are often CD8(+)
PTCL with “follicular” pattern
Also reported as perifollicular, intrafollicular, or paracortical nodular variants of PTCL
Intrafollicular aggregates of T-cell lymphoma that mimic follicular lymphoma at low-power magnification
Enlarged perifollicular zones surrounding hyperplastic follicles mimicking nodal marginal zone B-cell lymphoma
Small nodular aggregates of PTCL in background of progressively transformed germinal centers
Can mimic nodular lymphocyte-predominant Hodgkin lymphoma
Neoplastic cells are T cells, usually CD4(+)
T zone
Predominantly perifollicular or interfollicular growth pattern
Reactive follicles are preserved and can be hyperplastic
Small or intermediate-sized neoplastic cells with clear or eosinophilic cytoplasm
Minimal nuclear pleomorphism
Commonly associated with vascular proliferation and heterogeneous mixture of reactive cells
PTCL with Associated B-cell Proliferation
Approximately 10% (or less) of PTCL cases can be associated with numerous B cells
B-cells are small mature plasma cells, plasmacytoid large B-lymphocytes, or plasmablasts
B cells are often EBV(+)
ANCILLARY TESTS
Immunohistochemistry
Mature T-cell immunophenotype
Pan-T-cell antigens(+)
CD4(+)/CD8(−) or CD4(−)/CD8(+)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree