Perineurioma
Lester D. R. Thompson, MD
Key Facts
Terminology
Benign peripheral nerve sheath tumor, specifically of perineurial cell derivation that surrounds endoneurial connective tissue space of nerve fibers
Etiology/Pathogenesis
May be related to Schwann cells, fibroblasts, or arachnoid cap cells
Clinical Issues
Women affected slightly more often than men
Presents with solitary, painless mass in superficial subcutaneous soft tissue
Macroscopic Features
Usually discrete but without easily detected capsule
Microscopic Pathology
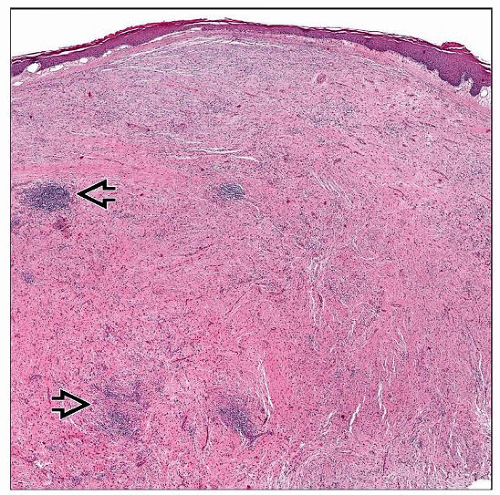
Superficial subcutaneous or dermal site, well circumscribed
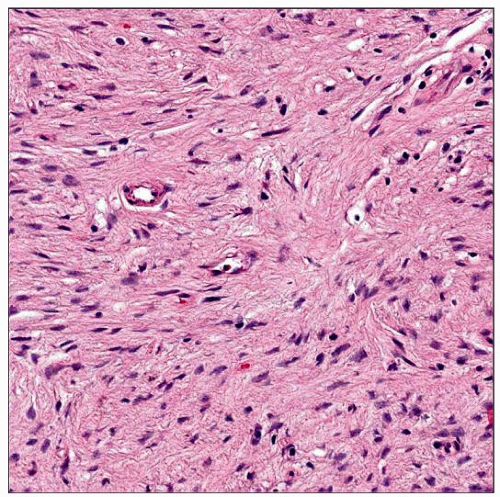
Spindled tumor cells organized in many patterns (fascicles, storiform, pinwheel, whorled, lamellar)
Bipolar, bland, plump spindled cells with pale, eosinophilic cytoplasm
Background stroma is collagenous, myxoid or a mixture, without vascular hyalinization
Ancillary Tests
Variably positive with perineurial markers (EMA, claudin-1, GLUT1, CD34) and collagen IV
Top Differential Diagnoses
Neurofibroma, schwannoma, solitary fibrous tumor, meningioma
TERMINOLOGY
Abbreviations
Soft tissue perineurioma (STP)
Synonyms
Storiform perineurial fibroma
Perineurial cell tumor
Definitions
Benign peripheral nerve sheath tumor, specifically of perineurial cell derivation that surrounds endoneurial connective tissue space of nerve fibers
Tumors are traditionally separated into intraneural, sclerosing, and soft tissue perineurioma
Perineurial cells can be seen in other tumors, such as neurofibroma and schwannoma
ETIOLOGY/PATHOGENESIS
Pathogenesis
May be related to Schwann cells, fibroblasts, or arachnoid cap cells
CLINICAL ISSUES
Epidemiology
Incidence
Exceedingly rare
Represents < 0.5% of peripheral nerve sheath tumors
Age
Wide age range: 2-85 years
Majority: 2nd-5th decades
Mean: 45 years
Gender
Slight female preponderance
Female > male (1.1-1.2:1)
Site
Superficial subcutaneous soft tissue
Most common in soft tissues of lower and upper extremities
2nd most common in trunk
Head and neck sites affected in ˜ 15% of all perineuriomas
Oral cavity is affected ˜ 4% of the time
Presentation
Most patients present with solitary painless mass
May have syndrome/familial association
Neurofibromatosis type 2 (NF2)
Nevoid basal cell carcinoma (Gorlin) syndrome
Interestingly, both have meningioma in common
Perineurium may be derived from arachnoid cap cells
Treatment
Surgical approaches
Excision is treatment of choice
Some advocate for wide excision to prevent recurrence
Prognosis
Local recurrence is uncommon (< 5% of cases)
May develop late
Only seen if originally incompletely excised
Metastases are not reported
Pleomorphic cells and infiltrative margins do not affect clinical outcome
MACROSCOPIC FEATURES
General Features
Usually discrete, but without easily detected capsule
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree