Penetrating Neck Injury
Andrew B. Peitzman
Alain Corcos
But one spot lay exposed, where collarbones lift the neckbone off the shoulders, the open throat, where the end of life comes quickest
Book 22: The Death of Hector, The Iliad
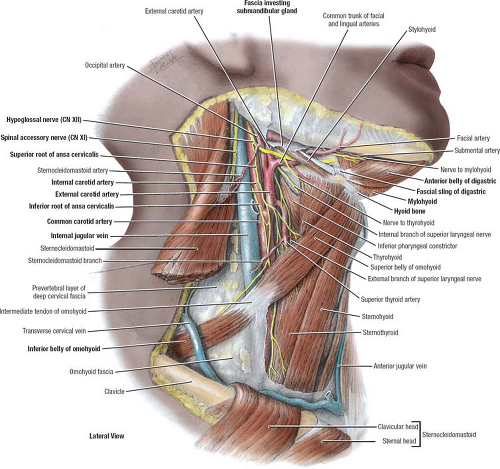
Few areas of the body concentrate vital anatomy as the neck. Notable structures include the pharynx, larynx, trachea, esophagus, common carotid artery, internal carotid artery, external carotid artery and its branches, the vertebral and subclavian arteries, the internal and external jugular veins and their tributaries, cranial nerves IX to XII (glossopharyngeal, vagus, spinal accessory, and hypoglossal), thyroid, parathyroid, and submandibular glands, and the bony spine and spinal cord. Knowledge of the anatomy of this region is essential. To begin, one must appreciate the importance of the platysma muscles. Spreading subcutaneously as a sheet across the entire length of the lower border of the mandible down to and across the length of the clavicle below, this muscle serves to distinguish superficial from deep. Deeper fasciae envelope the infrahyoid “strap” muscles (sternohyoid, omohyoid, and sternothyroid) laterally, and encircle the esophagus and trachea centrally. Palpable landmarks along the midline of the neck, which is not covered by platysma muscle, include the thyroid cartilage superiorly, the cricoid cartilage caudally, and the suprasternal notch at the base of the neck between the clavicles.
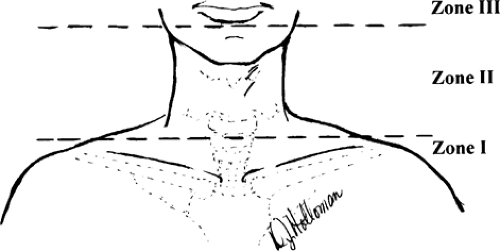
Traditionally, anatomists divide the neck into triangular areas (Fig. 1), bordered by musculature and bony landmarks, while surgeons refer to Monson’s three “zones” of the neck. The dominant muscular landmark of the lateral neck is the sternocleidomastoid muscle. Coursing obliquely from the skull base to the sternum and medial clavicle, the sternocleidomastoid separates anterior and posterior triangles. The anterior triangle is further bounded by the midline and lower border of the mandible and contains the “carotid bundle” (carotid artery and bifurcation, internal jugular vein, and vagus nerve) (Fig. 2). Zone I of the neck extends from the clavicle to the cricoid cartilage, zone II from the cricoid to the angle of the mandible, and zone III from the angle of the mandible to the skull base. Surgeons have historically favored the classification by zones because it is useful in prediction of operative access to structures of surgical importance. While injuries within zone II are easily exposed and repaired, operative approaches to zones I (the thoracic outlet) and III (the skull base) are challenging.
As with any injured patient, the principles set forth by Advanced Trauma Life Support guide our initial assessment. Important information from the history includes mechanism of injury and blood loss at the scene. Gunshot wounds are associated with a significantly higher likelihood of vital structure injury than stab wounds. The primary survey will identify patients in shock or with hard signs of vital structure injury such as airway compromise, massive subcutaneous emphysema, a sucking wound, active hemorrhage, expanding or pulsatile hematoma, carotid bruit or thrill, neurologic defect, or absent/decreased radial pulse in the ipsilateral upper extremity. Immediate surgical intervention is indicated when any of these “hard” signs are appreciated.
Impending airway occlusion can occur with tracheal or laryngeal injury, with compression from a large or expanding hematoma, or from intraoral hemorrhage. Control of the airway is a priority in these patients and may be accomplished by oral endotracheal intubation, cricothyroidotomy, or formal tracheotomy. While blind nasotracheal intubation is contraindicated in this setting, fiberoptic bronchoscopy-assisted nasotracheal intubation may be helpful when tracheal deviation from large hematoma is present. It is important to recognize the patient with penetrating neck injury who has a large hematoma or blood in the hypopharynx, who needs to be intubated early but not urgently in the emergency department, and who is spontaneously breathing. The initial inclination in such a patient is often rapid sequence induction with pharmacologic paralysis. This may convert a patient who was marginally protecting his airway but breathing to the patient who now cannot be intubated or ventilated with a bag valve mask. Recognition of such patients and control of the airway with the patient awake, sometimes including a surgical airway under local anesthesia, is critical to prevent an avoidable disaster.
When oral intubation fails or is not feasible, cricothyroidotomy is the quickest and most efficient way to access and secure the airway. It is critical to understand that this is a procedure performed basically by palpation, not by visualization, of structures. If right-handed, the operator should be on the patient’s right side and should begin by palpating the superior and inferior aspects of the thyroid cartilage and by securing this structure with his left hand between the thumb and middle fingers, leaving the index finger free to palpate the membranous space between the thyroid and cricoid cartilages. A transverse incision or vertical incision (if landmarks are not absolutely clear) is made at this level and the subcutaneous tissues are separated bluntly with a straight or curved clamp to the cricothyroid membrane, which is then incised with a No. 11 or 15 knife blade for direct access to the subglottic space. This will allow entry of the left index finger for control and dilatation or one can use the knife handle or curved clamp to dilate the space. A No. 6 endotracheal tube can then be positioned and secured (or No. 5 in a small female). Do not incise too deeply with the blade, as this can injure posterior trachea wall and esophagus. In addition, avoid cutting or spreading in a vertical axis, as this may injure the cricoid cartilage. Remember that the cricoid cartilage is the only circumferential support for the airway; injury will require repair. When a cricothyroidotomy is required it should be converted to a tracheotomy at the earliest safe opportunity.
Large-bore peripheral venous catheters are adequate for circulatory support. However, avoid the ipsilateral upper extremity as an access site in patients with zone I (thoracic outlet) entry or trajectory. Patients should have plain radiographs of the chest to assess for hemopneumothorax or missiles and as thorough a neurologic examination as possible prior to sedation and intubation. Active hemorrhage from a wound in the neck in any zone is best managed by digital compression until the airway is controlled and surgical access can be obtained. This digital tamponade may be required until proximal and distal vascular control can be obtained in the operating room. On occasion, gauze packing or insertion of a balloon catheter in the oral cavity to control hemorrhage may be necessary.
Physical examination is unreliable in excluding aerodigestive tract injuries in the asymptomatic patient with penetrating neck wounds deep to the platysma muscle. Although some authors have described successful observation protocols in patients without hard signs of vascular injury, such protocols are not appropriate to exclude pharynx, esophagus, larynx, or trachea injury in the asymptomatic patient. The diagnostic approach to this group of patients has evolved significantly over the past two decades. Mandatory surgical exploration of injuries in zone II trades ease and reliability for a high rate of negative and nontherapeutic operation. A more selective operative approach, based on findings from various radiologic and endoscopic studies, has replaced this standard. With the advancements in technology associated with the multislice helical computed tomography (CT) scanner, CT angiography (CTA) has emerged as the screening modality of choice for penetrating neck wounds in asymptomatic or stable patients. CTA is easily accessible, well tolerated with minimal risk, sensitive for defining trajectory, and reliable to exclude significant arterial injury. Abnormalities identified on CTA or trajectory suspicious for aerodigestive tract injury should be further evaluated with surgical exploration, laryngoscopy, tracheobronchoscopy, catheter-based arteriography, esophagoscopy, or esophagography as needed. A comprehensive literature review by the Practice Management Guidelines Committee of the Eastern Association for the Surgery of Trauma in 2008 concluded that “either contrast esophagography or esophagoscopy can be used to rule out an esophageal perforation that requires operative repair.”
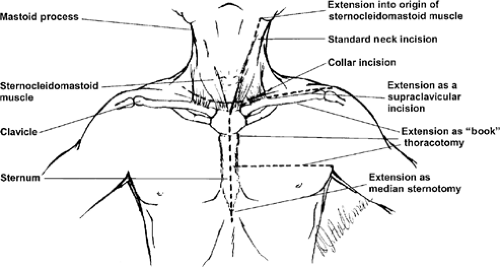
In the symptomatic patient who requires operation without prior diagnostic testing, zone of entry and likely trajectory are critical for planning exposure. The patient should be positioned supine, with arms tucked, neck extended, and head deviated slightly away from the side of injury. A towel roll placed transversely beneath the shoulder will extend the neck. The sterile preparation should include both sides of the neck from the temporomandibular joint to the lower lip down to and including the entire anterior chest to the table laterally and torso distally to the midthighs. Thoracotomy or median sternotomy may be required for proximal control; this may be the initial incision with zone I injury (Fig. 3). Access to the groins and saphenous veins must be available. Zone II injuries are best approached via an oblique incision along the anterior border of the sternocleidomastoid muscle from the angle of the jaw to the clavicular head (Fig. 4). With zone I entry, the surgeon should be prepared to perform a median sternotomy for access to and repair of structures in the thoracic outlet or base of the neck. In this circumstance the ipsilateral arm should be free and prepped to the elbow. A horizontal incision along the superior aspect of the clavicle will supply access to the proximal subclavian vessels and innominate vessels on the right. This incision may be independent or can extend an anterior sternocleidomastoid or median sternotomy incision when
necessary. Clavicle resection is usually only necessary if access to the axillary artery is required. Exposure to the left subclavian artery at its origin is difficult through a median sternotomy due to its posterior position on the aortic arch. When exposure of the proximal left subclavian artery is required, it is best obtained via a left anterior thoracotomy. Wounds in zone III may require a curvilinear posterior extension over the mastoid process to allow exposure of the distal internal carotid artery to the skull base (see “Surgical Technique”). A horizontal “collar” incision can offer excellent exposure to multiple zones when subplatysmal flaps are developed. This incision is most useful for isolated laryngotracheal injuries that require a surgical airway or axial traverse gunshot wounds that require bilateral exploration.
necessary. Clavicle resection is usually only necessary if access to the axillary artery is required. Exposure to the left subclavian artery at its origin is difficult through a median sternotomy due to its posterior position on the aortic arch. When exposure of the proximal left subclavian artery is required, it is best obtained via a left anterior thoracotomy. Wounds in zone III may require a curvilinear posterior extension over the mastoid process to allow exposure of the distal internal carotid artery to the skull base (see “Surgical Technique”). A horizontal “collar” incision can offer excellent exposure to multiple zones when subplatysmal flaps are developed. This incision is most useful for isolated laryngotracheal injuries that require a surgical airway or axial traverse gunshot wounds that require bilateral exploration.
Carotid Artery
Carotid artery injury should generally be repaired. Primary repair, patch angioplasty, or interposition grafting are options depending on the nature of the injury. Small, clean wounds (stab wounds <2 cm) that can be approximated without significant narrowing should be repaired with a nonabsorbable, monofilament suture (4-0, 5-0, or 6-0 polypropylene). Saphenous vein or polytetrafluoroethylene (PTFE) can be used for patch repair in cases where primary closure would narrow the vessel or as an interposition conduit when segmental resection is required and end-to-end repair is restricted by tension. PTFE as a conduit has not been shown to increase the incidence of thrombosis or infection when compared with the saphenous vein.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree