• Site of attachment of axial skeleton and lower limbs • Transmits weight of upper limbs, head, neck, and trunk to lower limb • Protects and contains pelvic viscera (distal ureters, bladder, rectum, sigmoid colon, reproductive organs) • Anterior superior iliac spine (ASIS) • Site of lateral attachment of inguinal ligament • Site of attachment of sartorius and tensor fascia lata muscles • Midpoint between pubic tubercle and ASIS marks the site for palpating femoral artery and vein (the midinguinal point) • Follows curve between anterior posterior superior iliac spines • Highest point is at approximately level of umbilicus—level of L4 vertebral body • Supracristal plane passes between highest points of iliac crests • Superior—pelvic inlet and inferior abdominal cavity • Anterior wall—bodies and rami of pubic bone and pubic symphysis • Posterior wall—sacrum and coccyx, adjacent ilia, and overlying piriformis muscle • Lateral walls—hip bones, obturator foramen and membrane, and overlying obturator internus muscle • Inlet defined by oblique plane • Rim of pelvic inlet = pelvic brim, composed of a bony line running through • Pelvic inlet divides pelvis into two parts • Birth canal includes pelvic inlet, true pelvis, cervix, vagina, and pelvic outlet • Union of bodies of right and left pubic bones • Secondary cartilaginous joint • Fibrocartilaginous interpubic disc in joint • Stabilized by superior and inferior pubic ligaments • Affected by the hormone relaxin during pregnancy to permit freer movement between vertebral column and to increase pelvic diameter during childbirth • The weight of the body acting through the spine will tend to rotate the sacrum, tipping the lower part backward. • This movement is prevented by the sacrospinous and sacrotuberous ligaments. • Sacrospinous ligament: extends from lateral border sacrum to ischial spine • Sacrotuberous ligament: larger and extends from dorsum and lateral border sacrum and posterior surface ilium to ischial tuberosity • Attachments of sacrospinous and sacrotuberous ligaments enclose the lesser and greater sciatic notches, respectively, forming the greater and lesser foramina Structures Passing Through the Greater and Lesser Sciatic Foramina • Differences linked to function • Pelvis is heavier and has more pronounced muscle attachment sites in men than in women. • Pubic arch is narrower and subpubic angle more acute in men than women. • Ischial tuberosities are closer in men than in women, and pelvis outlet is thus comparatively smaller. • All of the ilia are less flared in men than in women, so the greater pelvis is deeper. • Pelvic inlet is heart-shaped in men and more transversely oval in women. • Obturator foramen is round in men and oval in women. • Female pelvis is broader than in men to allow passage of fetal head. • Used to determine capacity of female pelvis for childbearing • Measured radiologically on a lateral x-ray • Distance from superior border of pubic symphysis to sacral promontory • Transverse diameter: widest distance of pelvic inlet • Oblique diameter: distance from sacro-iliac joint to contralateral iliopectineal line • A large force is required to fracture the pelvis, and fractures usually result from direct trauma, such as occurs in automobile accidents. • The bony pelvis may fracture at any point and there may be associated damage to pelvic viscera; for example, bladder and urethral rupture can occur with fractures involving the pubis. • Pelvic fractures are classified as stable or unstable. • In a stable fracture, the pelvis remains stable and there is only one break-point in the pelvic ring with minimal hemorrhage. • In an unstable fracture, the pelvis is unstable with two or more break-points in the pelvic ring with moderate to severe hemorrhage. • Signs of a fractured pelvis include pain in the groin, hip, or lower back; difficulty walking; urethral, vaginal, or rectal bleeding; scrotal hematoma; and shock as a result of concealed hemorrhage (contained bleeding into the pelvic cavity) • A fracture can be confirmed on radiograph and is seen as a break in continuity of the pelvic ring. • Can be a partial- or full-thickness loss of skin, underlying connective tissue, and can extend into muscle, bone, tendons, and joint capsules • Two thirds of pressure sores occur in patients older than 70 years. • Results from prolonged pressure on an area of skin, connective tissue, and muscle from a mattress, wheelchair seat, or bed rail • Commonly occur in those with poor mobility, bed-bound, poor nutrition, and incontinence. • Can become infected with bacteria from poor skin care or fecal or urinary incontinence • The hip and buttock regions account for 67% of all pressure sores, with ischial tuberosity, trochanteric, and sacral locations being most common. • In the sitting position, the ischial tuberosity bears the weight of the whole body and thus is a prime site of ulceration. • Muscular partition from pubis to coccyx and from lateral wall to lateral wall • Separates pelvic cavity from perineum inferiorly • Pelvic diaphragm is composed of two paired muscles • Arcus tendineus: thickened line of fascia over obturator internus muscles running in arching line from pubis to ischial spine • Central perineal tendon or perineal body • Components of levator ani muscle • Is anterior part of levator ani • Main contributor to levator ani • Arises from posterior body of pubic bone and anterior part of arcus • Medial muscle fibers of the pubococcygeus border the urogenital hiatus • Most anterior fibers insert into urethra • Other fibers sweep behind vagina or prostate and insert into central perineal tendon—called levator prostatae, or pubovaginalis. • Reinforces pelvic floor posteriorly • Inserts on lower two sacral and upper two coccygeal segments • Innervation of levator ani and coccygeus muscles • Levator ani innervated by branches from anterior rami of S3–S4 spinal nerves. • Puborectalis also innervated by branch of pudendal nerve (S2,3,4). • Coccygeus supplied by branches of anterior rami of S4–S5 spinal nerves. • Proximal attachment: pelvic surfaces of ischium and ilium and obturator membrane • Distal attachment: greater trochanter of femur • Innervated by nerve to obturator internus (L5, S1–S2) • Occupies space between peritoneum and muscles of pelvic floor and walls • Parietal pelvic fascia lines internal surface (facing pelvic cavity) of muscles of floor and walls. • Visceral pelvic fascia invests each of the pelvic organs. • Visceral and parietal fascia are continuous where organs penetrate pelvic floor. • Where they are continuous, fascia thickens to form tendineus arch of pelvic fascia (arcus tendinous fasciae pelvis). • Arches are bilateral bands running from pubis to sacrum, adjacent to viscera. • Between parietal and visceral fascia is endopelvic fascia • Major condensation is hypogastric sheath. • Transverse cervical (cardinal) ligaments are part of hypogastric sheath. • Run from lateral wall to uterine cervix and vagina • Uppermost part is beneath broad ligament and transmit uterine artery • Sufficiently fibrous to provide passive support for uterus • Uterosacral (female) or genitosacral (male) ligaments • Septa separate the pelvic organs and include • Weakness of pelvic floor muscles or in pelvic fascia, which support the pelvic organs, can result in prolapse of pelvic organs (e.g., vaginal or rectal prolapse). • Lines lateral and posterior pelvic walls and pelvic floor • Covers rectum, urinary bladder, uterus, and adnexa in females • Covers anterior and lateral surfaces of upper portion of rectum in both sexes • Sweeps forward from rectum to bladder • Creates recess between rectum and bladder: rectovesical pouch • Continues over superior surface of bladder and ascends on internal side of anterior abdominal wall • Sweeps forward from rectum onto posterior fornix of uterus and posterior uterine wall • Creates recess between rectum and uterus: recto-uterine pouch (of Douglas) • Covers posterior, superior, and anterior surfaces of uterus before reflecting onto superior surface of bladder • Fluid (blood, pus) can collect in rectovesical or recto-uterine pouches, causing infection and forming pelvic abscesses. • Cross pelvic brim at level of sacro-iliac joint, anterior to bifurcation of common iliac artery to pierce posterior surface of bladder • Enter posterolateral surface of bladder and run obliquely through bladder wall, creating flap valve • In males: pass under ductus deferens, superior to seminal vesicles • In women: descend posterior to ovary and into base of broad ligament, passing under uterine artery (“water under the bridge”) • Supplied by branches of common and internal iliac arteries and uterine artery (inferior vesicle artery in males) and drained by veins with same names. • Lies posterior to pubic bones and pubic symphysis • When empty is tetrahedron in shape and lies entirely within true pelvic cavity; spherical when full and may reach as high as umbilicus • When empty has base (posterior surface) and one superior and two inferolateral surfaces • Base (posterior surface) of bladder defined internally by two ureteric openings at superolateral corners and internal urethral opening inferiorly • Triangular area defined by these openings is vesicle trigone. • Ridge between two urethral openings is interureteric fold. • Neck of bladder is where base and inferolateral sides meet, inferiorly. • Anterior angle or apex is site of attachment of urachus—fibrous remnant of fetal allantois, which is seen as median umbilical ligament on anterior abdominal wall. • Bladder wall is composed of thick layer of interwoven bundles of smooth muscle running transversely, longitudinally, and obliquely—detrusor muscle. • In region of neck, detrusor muscle runs circularly as involuntary internal sphincter. • Bladder mucosa is thrown into rugae except within trigone, which is smooth. Relations of the Urinary Bladder • Superior vesicle arteries (branches of internal iliac artery) supply apex and superior part of bladder. • Inferior vesical arteries supply fundus and neck in males. • Vaginal arteries (branches of uterine arteries) supply fundus and neck in females. • Obturator arteries (branches of internal iliac artery) provide arterial twigs. • 3- to 4-cm long fibromuscular tube bound to anterior vaginal wall • Extends from internal urethral meatus of bladder to external meatus situated just anterior to vaginal opening in vestibule • Descends with vagina through urogenital hiatus and pelvic diaphragm and through perineal membrane, where it is surrounded by external sphincter urethrae • Para-urethral glands, homologs to the prostate, open on either side near external urethral orifice • Supplied by internal pudendal and vaginal arteries • Drained by veins of same name • Innervated by branches of pudendal nerve via S2–S4 spinal cord segments and afferents run with pelvic splanchnic • Conveys both urine and semen • Extends from internal urethral meatus of bladder to external urethral meatus in glans penis • Divided into three parts: prostatic, membranous, and spongy urethra Comparison of Prostatic, Membranous, and Spongy Parts of the Male Urethra • The bladder has a capacity of 400 to 500 mL. • During micturition, coordinated reflexive contraction of detrusor and relaxation of external urethral sphincter occur. • Controlled by autonomic and visceral innervation • Visceral afferent fibers traveling along tract of parasympathetic fibers are stimulated by stretching (and pain in lower bladder). • Parasympathetic innervation via pelvic splanchnic nerves and pelvic plexus reflexively stimulates detrusor contraction during micturition. • Sympathetic fibers via hypogastric plexus to bladder neck relax bladder neck (internal urethral sphincter) and prevent retrograde ejaculation during micturition in males. • As a result of a shorter urethra, women are more susceptible to UTIs. • Commonly occurs in women after sexual intercourse • Pathogen is commonly Escherichia coli. • Infection may lead to urethritis, cystitis, or pyelonephritis (inflammation of urethra, bladder, and kidneys, respectively). • Symptoms include dysuria, urgency, frequency, and occasionally hematuria. • Factors maintaining continence in the female are the external urethral sphincter (striated muscle surrounding middle third of urethra) and support of the bladder and urethra by the levator ani muscles. • Urinary stress incontinence is an involuntary loss of urine that occurs during coughing, sneezing, laughing, lifting, or exercise, because of the inability of these muscles to counter the increase in intra-abdominal pressure. • Urinary stress incontinence is often seen in women who have had multiple pregnancies and vaginal childbirths and in men after prostate surgery. • About 50% of all women have occasional urinary incontinence • Approximately 8 cm long by 5 cm wide • Supported by the pelvic diaphragm • Body (corpus)—upper two thirds • Fundus—rounded upper part superior to entrances of uterine tubes • Isthmus—narrower area just above cervix • Cervix (neck)—cylindrical inferior part that projects into superior vagina • Uterine cavity is small (6 cm in length) and slitlike. • Uterine horns are superolateral regions where the uterine (fallopian tubes) enter. • Uterine wall has three layers. • Perimetrium—outer layer of peritoneum with underlying connective tissue • Myometrium—middle, thick layer of smooth muscle • Endometrium—vascular inner mucosal layer the thickness of which varies with menstrual cycle and age • Uterus has two surfaces: anteroinferior and posterosuperior. • A portion of the cervix and body and fundus of uterus are covered with peritoneum. • Thick-walled canal, 2.5 cm long, connecting body of uterus with vagina • Communicates superiorly via internal os with uterus • Communicates with vagina inferiorly via external os • Approximately half of cervix lies above vagina (supravaginal) and is covered posteriorly with peritoneum of recto-uterine pouch. • Bladder is separated from anterior surface the supravaginal part of cervix by connective tissue. • Lower half of cervix (vaginal part) protrudes into vagina and can be examined clinically.
Pelvis and Perineum Study Guide
5.1 Topographic Anatomy
Guide
Functions of the Pelvic Girdle
Key Landmarks
5.2 Bones and Ligaments
Guide
Bones and Boundaries of the Pelvis
Pelvic Cavity
Pelvic Inlet, Outlet, and Brim
Joints of the Pelvis
Pubic Symphysis
Ligaments of the Pelvis
Greater Sciatic Foramen
Lesser Sciatic Foramen
Piriformis muscle
Tendon of obturator internus
Sciatic nerve
Nerve to obturator internus
Inferior gluteal nerve and artery
Pudendal nerve
Internal pudendal nerve, artery, and vein
Internal pudendal artery
Nerve to obturator internus muscle
Nerve to quadratus femoris
Posterior cutaneous nerve of the thigh
Sex Differences of Pelvis
Anatomical Points
Measurements of the Pelvic Inlet
Clinical Points
Fractures of the Pelvis
Decubitus Ulcers
5.3 Pelvic Floor and Contents
Guide
Pelvic Floor
Muscles of Pelvic Floor
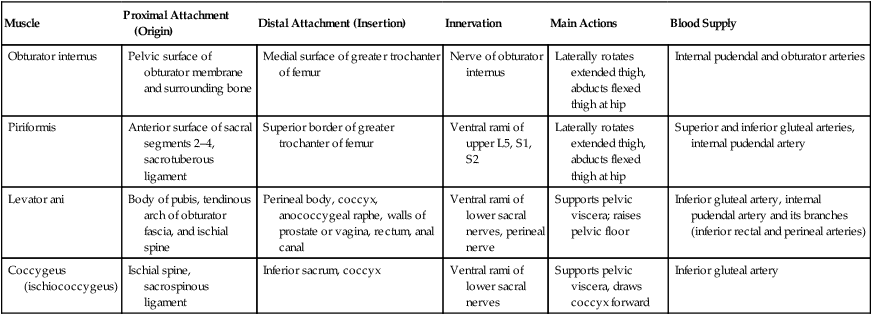
Muscles Lining Lateral Walls of Pelvis
Muscle
Proximal Attachment (Origin)
Distal Attachment (Insertion)
Innervation
Main Actions
Blood Supply
Obturator internus
Pelvic surface of obturator membrane and surrounding bone
Medial surface of greater trochanter of femur
Nerve of obturator internus
Laterally rotates extended thigh, abducts flexed thigh at hip
Internal pudendal and obturator arteries
Piriformis
Anterior surface of sacral segments 2–4, sacrotuberous ligament
Superior border of greater trochanter of femur
Ventral rami of upper L5, S1, S2
Laterally rotates extended thigh, abducts flexed thigh at hip
Superior and inferior gluteal arteries, internal pudendal artery
Levator ani
Body of pubis, tendinous arch of obturator fascia, and ischial spine
Perineal body, coccyx, anococcygeal raphe, walls of prostate or vagina, rectum, anal canal
Ventral rami of lower sacral nerves, perineal nerve
Supports pelvic viscera; raises pelvic floor
Inferior gluteal artery, internal pudendal artery and its branches (inferior rectal and perineal arteries)
Coccygeus (ischiococcygeus)
Ischial spine, sacrospinous ligament
Inferior sacrum, coccyx
Ventral rami of lower sacral nerves
Supports pelvic viscera, draws coccyx forward
Inferior gluteal artery
Pelvic Fascia
Clinical Points
Peritoneal Reflections
5.4 Urinary Bladder
Guide
Ureters
Urinary Bladder
General Structure
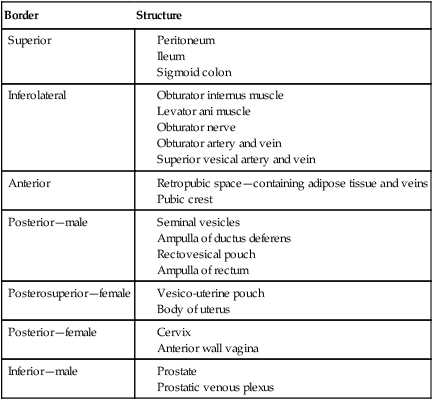
Border
Structure
Superior
Inferolateral
Anterior
Posterior—male
Posterosuperior—female
Posterior—female
Inferior—male
Arterial Supply
Female Urethra
Male Urethra
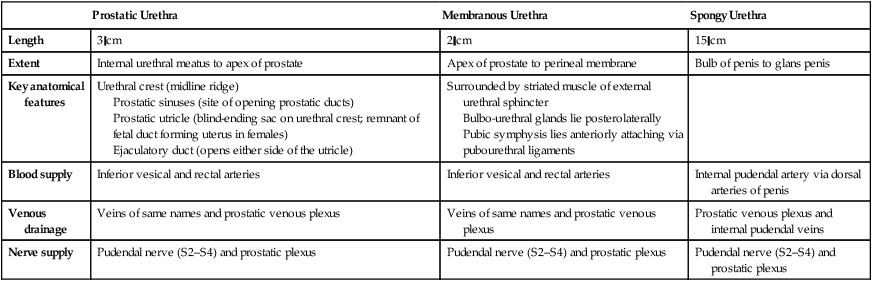
Prostatic Urethra
Membranous Urethra
Spongy Urethra
Length
3 cm
2 cm
15 cm
Extent
Internal urethral meatus to apex of prostate
Apex of prostate to perineal membrane
Bulb of penis to glans penis
Key anatomical features
Urethral crest (midline ridge)
Prostatic sinuses (site of opening prostatic ducts)
Prostatic utricle (blind-ending sac on urethral crest; remnant of fetal duct forming uterus in females)
Ejaculatory duct (opens either side of the utricle)
Surrounded by striated muscle of external urethral sphincter
Bulbo-urethral glands lie posterolaterally
Pubic symphysis lies anteriorly attaching via pubourethral ligaments
Blood supply
Inferior vesical and rectal arteries
Inferior vesical and rectal arteries
Internal pudendal artery via dorsal arteries of penis
Venous drainage
Veins of same names and prostatic venous plexus
Veins of same names and prostatic venous plexus
Prostatic venous plexus and internal pudendal veins
Nerve supply
Pudendal nerve (S2–S4) and prostatic plexus
Pudendal nerve (S2–S4) and prostatic plexus
Pudendal nerve (S2–S4) and prostatic plexus
Clinical Points
Micturition
Urinary Tract Infections (UTIs)
Urinary Stress Incontinence
5.5 Uterus, Vagina, and Supporting Structures
Guide
Structures
Uterus
Basic Structure.



