4 (Part II) The therapeutic properties of essential oils
There are many reasons why essential oils need to be included in the armoury of the fight against disease. They have many positive properties and effects which are desirable and have few drawbacks. They are capable of being anti-inflammatory, antiseptic, appetite stimulating, carminative, choleretic, circulation stimulating, deodorizing, expectorant, granulation stimulating, hyperaemic, insecticidal, insect repelling and sedative (Schilcher 1985 p. 217). They are natural antimicrobial agents able to act on bacteria, viruses and fungi, and many trials have been performed in this field (see below).
Essential oils are applied to the skin, ingested or inhaled, and all are harmless unless used incorrectly. They are much used in products for the home (obvious examples are lemon and lavender) and are well accepted, and the aroma can have beneficial effects on the person using them (see Ch. 7).
The aromatherapist determines the therapeutic materials to be used so that the treatment is tailored to the individual patient. Generally speaking there is an absence of unwanted side effects from the use of essential oils (see Synergism in Ch. 3 Part I); also, plant extracts are ecologically sound, causing no pollution, unlike antibiotics, which are flushed down the drain and pollute the land (Verdet 1989).
Antiseptic, antibacterial
Essential oils have multiple actions and effects, e.g. when used for a respiratory infection an oil may be not only antiseptic but also mucolytic and anti-inflammatory (Duraffourd 1987 p. 17). In the digestive system, the oils are antiseptic in action but do not act unfavourably on flora and the digestive secretions, in contrast to some unwelcome effects of antibiotics. The molecules of essential oils are not inimical to the human body: they support the immune system and can be considered as pro– and eubiotic as opposed to synthetic antibiotics.
Essential oils are especially valuable as antiseptics because their aggression towards microbial germs is matched by their total harmlessness to tissue; one of the chief drawbacks of some antiseptics used today is that they are likely to be as harmful to the cells of the organism as to the cause of the disease. It is very important to remember that antiseptics can destroy not only the microorganisms but also the surrounding cells (Valnet 1980 p. 44).
Case 4.1 Antibacterial, antiinfectious, cicatrizant (A deep, open wound)
Assessment
2 drops Lavandula angustifolia – antibacterial, anti-inflammatory, cicatrizant
2 drops Melaleuca alternifolia [tea tree] – antibacterial, anti-infectious
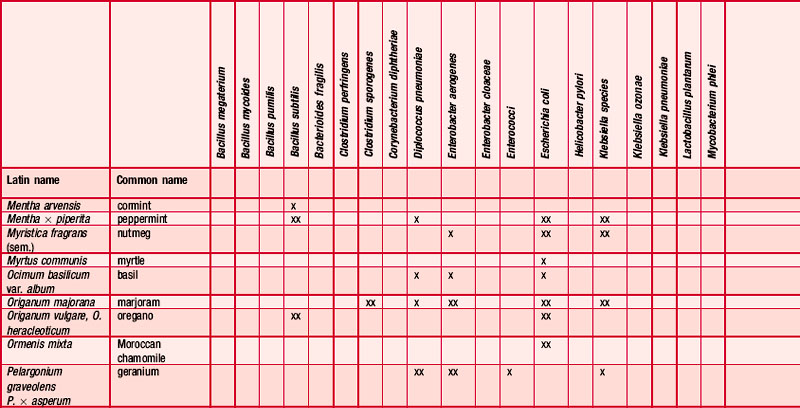
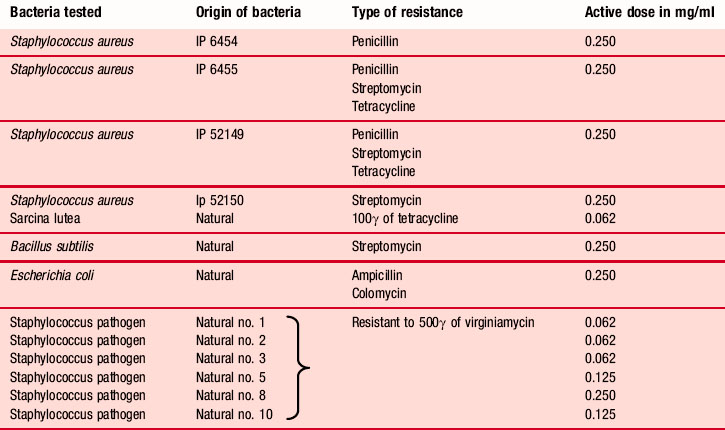
selectively (Pellecuer, Allegrini & De Buochberg 1974). Germs resistant to synthetic antibiotics are susceptible in certain cases to some essences in high dilution, e.g. 1 in 16,000 for Satureia montana (Belaiche 1979 p. 31) (Table 4.1).
Table 4.1 Antibacterial spectrum of Satureia montana on some species and strains resistant to antibiotics (after Pellecuer et al. 1976)
Testing for antiseptic and antibacterial activity
Tests have been carried out on the antiseptic and antibacterial properties of essential oils for more than a century, and now there is a reasonably good knowledge base on this aspect of the effects of essential oils – Koch’s 1881 investigation of turpentine with respect to the anthrax bacillus and Chamberland’s 1887 investigation into the activity of cinnamon oils, angelica and geranium. Since then the antiseptic and bactericidal powers of many essential oils have been tested many times in laboratories across the world using the aromatogram technique, a recognized standard test; the results obtained are repeatable and universally accepted: it is virtually the same as the antibiogram test.
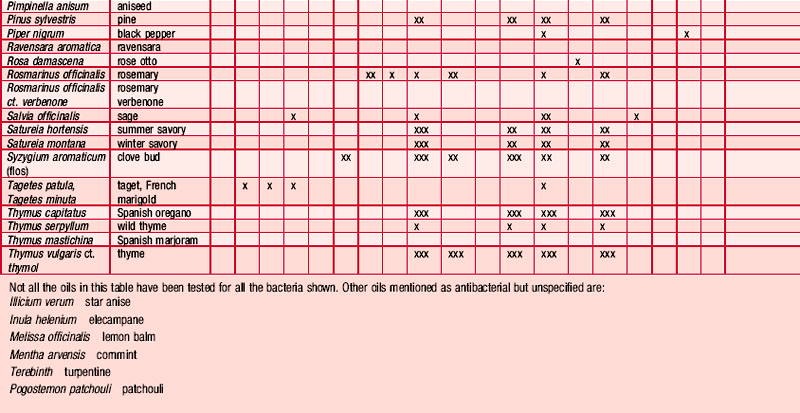
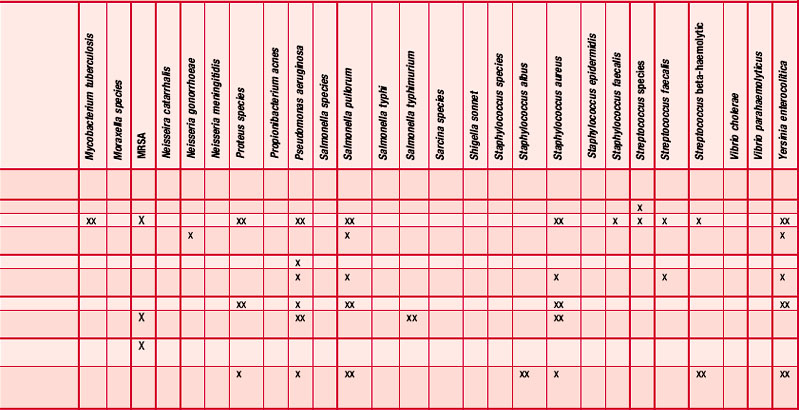
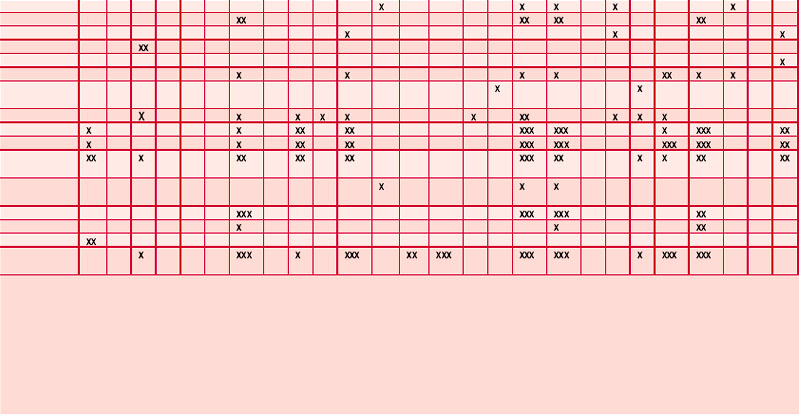
Antibiogram and aromatogram
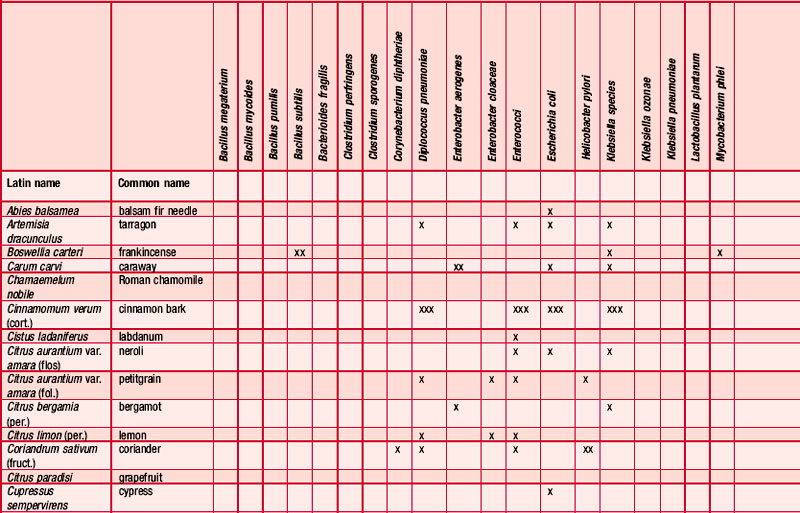
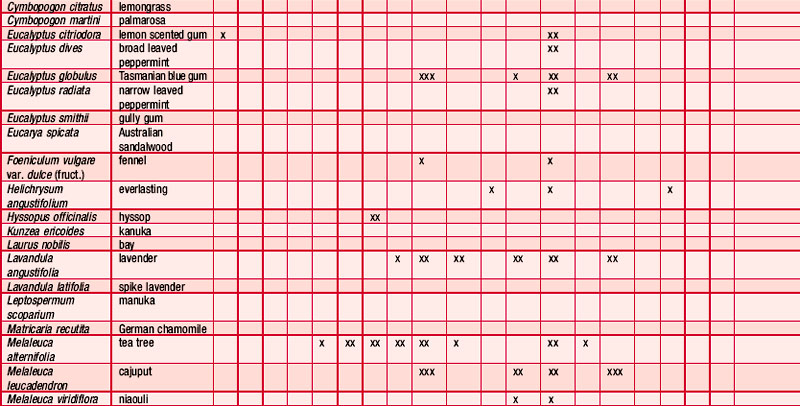
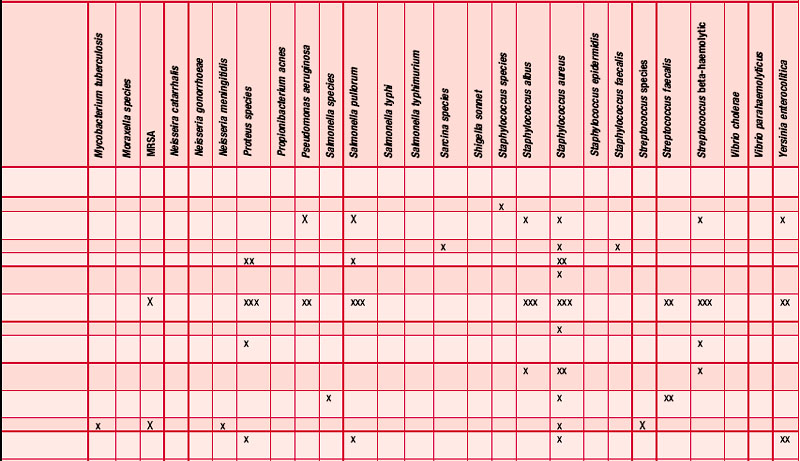
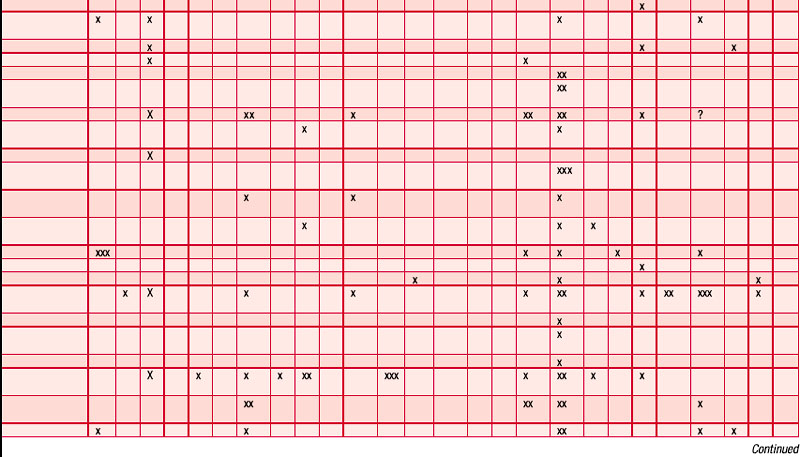
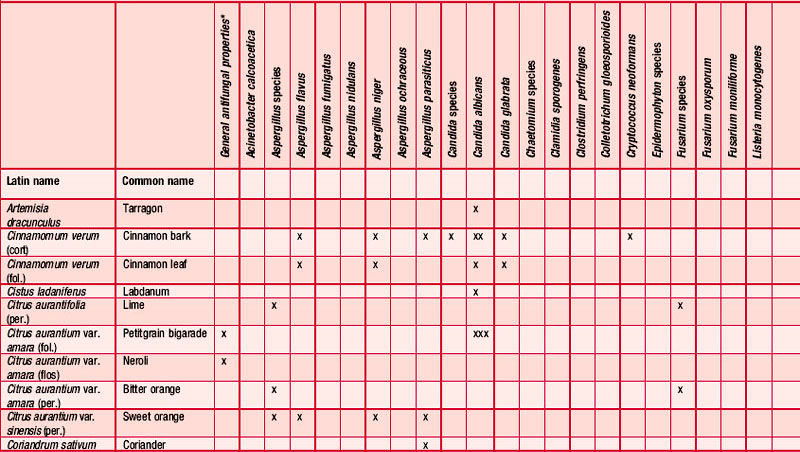
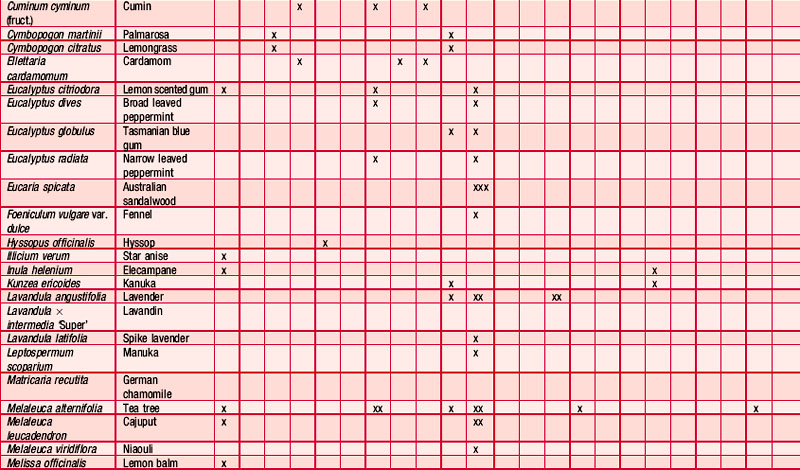
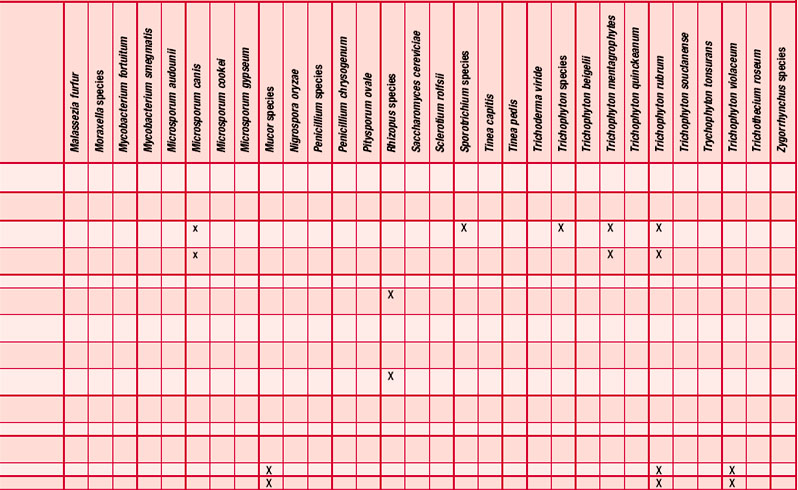
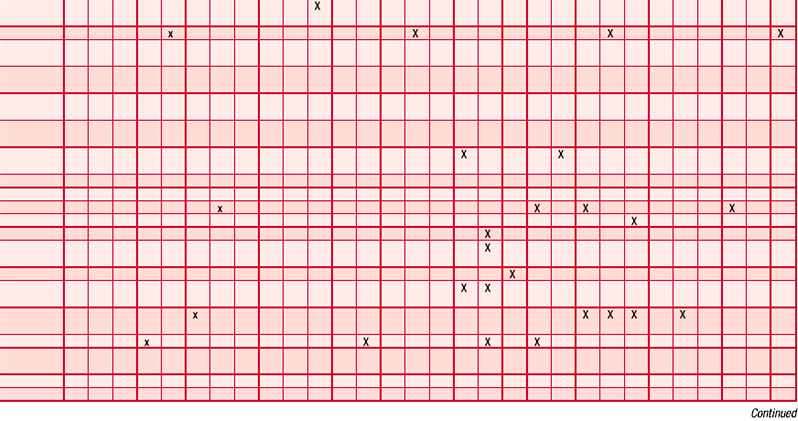
An antibiogram can test the validity of an antibiotic agent for the treatment of, say, a chest infection. A sample of sputum is taken and a culture grown in a dish. The antibiotic is introduced into the centre of the culture and its activity against the offending microorganism measured by the diameter of a clear ‘killing zone’, which indicates the power of the antibiotic: the greater the diameter, the greater the effectiveness of the antibiotic agent. An aromatogram is carried out in exactly the same way except that essential oil is used instead of an antibiotic. Both methods are subject to the proviso that in vitro activity is not always echoed in vivo, which is modified by absorption, metabolism, bioavailability etc. Finding the most effective essential oil to counteract a specific germ can be a lengthy undertaking: if there were no previous experience to draw on it would be necessary to test all the oils available to the therapist. This testing procedure has confirmed the antiseptic powers of many oils and at the same time has revealed previously unsuspected antiseptic powers in other oils. Foeniculum vulgare var. dulce [fennel] was known only for being an appetite stimulant, Myristica fragrans [nutmeg] as a stomachic and Artemisia dracunculus [tarragon] as an antispasmodic, but now the antiseptic qualities of these oils are also recognized. A huge number of aromatogram results have now been published, making it possible to list the major essential oils by their antimicrobial properties (Table 4.2).
Essential oils provide a very pleasant and effective means of disinfecting the air in an enclosed area (Kellner & Kober 1954, 1955, 1956) and are therefore ideal for use in sick rooms, burns units, reception areas, waiting rooms etc. A test describing the use of a blend of pine, thyme, peppermint, lavender, rosemary, clove and cinnamon essential oils for the bacteriological purification of the air concluded that ‘the atmospheric dispersion of the prepared liquid brought about a very marked disinfection of the air, as demonstrated by the considerable reduction in the number of pre-existing micro-organisms, some types being destroyed completely’ (Valnet 1980 pp. 36–38).
Methicillin resistant Staphylococcus aureus (MRSA)
Hospital-acquired infections and antibiotic-resistant bacteria continue to be major health concerns worldwide. Particularly problematic is MRSA and its ability to cause severe soft tissue, bone or implant infections, but recent experience has indicated that essential oils have an important part to play in dealing with this resistant bacterium. At a presentation to the Royal Society of Medicine, Michael Smith, pathologist, stated that several essential oils (including Ormenis multicaulis, Origanum vulgare, Thymus vulgaris ct. thymol, Lavandula intermedia ‘Super’, Cupressus sempervirens, Mentha x piperita, Ravensara aromatica, Juniperus communis (unspecified), Citrus limon, Cymbopogon martinii, Eucalyptus globulus and Eucalyptus smithii) were effective against MRSA (cited in Buckle 1997 p. 125). Sherry et al. (2001) successfully used a blend of phytochemicals (Eucalyptus globulus, Melaleuca alternifolia, Thymus sp., Syzygium aromaticum, citrus extracts and bioethanol) to treat two cases of MRSA infection with no reported recurrence. More recently several common and hospital-acquired bacterial and yeast isolates (six Staphylococcus strains including MRSA, four Streptococcus strains and three Candida strains, including Candida krusei) were tested by Warnke et al. (2009) for their susceptibility to eucalyptus, tea tree, white thyme, lavender, lemon, lemongrass, cinnamon, grapefruit, clove bud, sandalwood, peppermint, kunzea and sage oil with the agar diffusion test. Large zones of inhibition were observed for white thyme, lemon, lemongrass and cinnamon oil, and other oils also showed considerable efficacy. Almost all the tested oils demonstrated efficacy against hospital-acquired isolates and reference strains.
Analgesic
Many essential oils have analgesic properties and there seems to be no single reason. It is thought that the effect is partly due to the anti-inflammatory, circulatory and detoxifying effects of some oils and to the anaesthetic effect of others. The phenol eugenol found in the oil of clove is well known for its use in calming dental pain, wintergreen oil (containing methyl salicylate, an ester) has traditionally been used in rubs for muscle pain, and menthol has been used specifically for headaches. On the skin, oils rich in terpenes have an analgesic effect, especially those containing p-cymene (Franchomme & Pénoël 2001 p. 99); many aromatherapists report that the oil of Melaleuca alternifolia [tea tree] has this effect, as have azulene and chamazulene (found in the chamomiles). Some essential oils have a universal sedative or soporific action leading to an easing of pain, e.g. Chamaemelum nobile, Cananga odorata, Citrus reticulata (fol.) (Rossi et al. 1988), Citrus bergamia per., fol. (Franchomme & Pénoël 2001 p. 99). According to Roulier (1990), the analgesic and antalgic essential oils are white birch, chamomile, frankincense, wintergreen, clove, lavender and mint (common names only given).
At Monklands Hospital in Scotland more than 75% of patients suffering from chronic complaints (e.g. back or shoulder pain, long-term problems, premenstrual tension, depression, anxiety or mood swings) referred by local GPs found that complementary therapies helped to provide short-term relief of their symptoms. The patients were treated with essential oils, reflexology or acupuncture during an 8-week trial (Anderson 1998) (see Appendix B.9 on the CD-ROM for a list of effective oils).
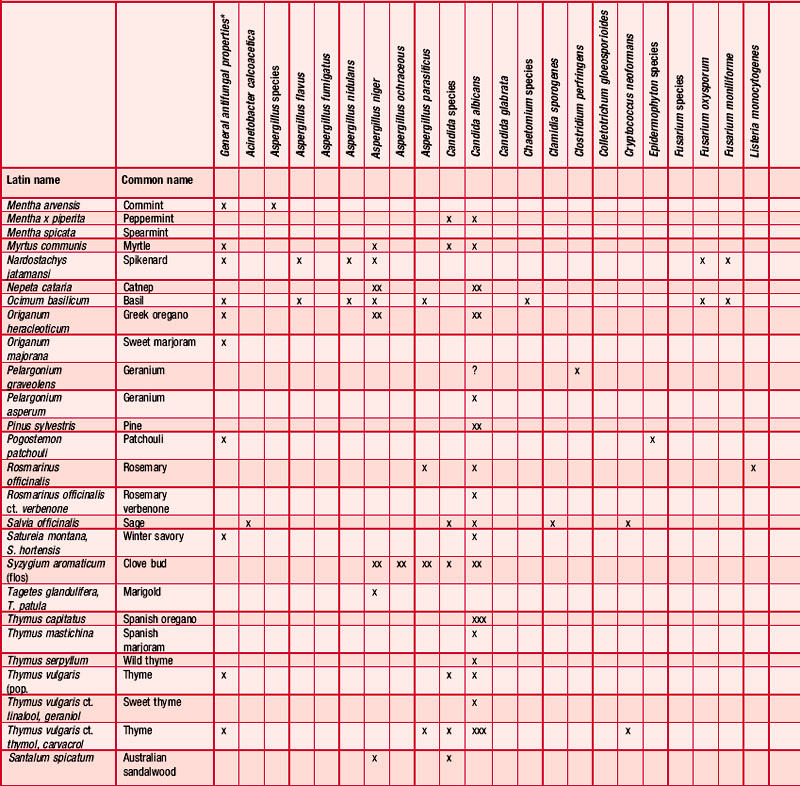
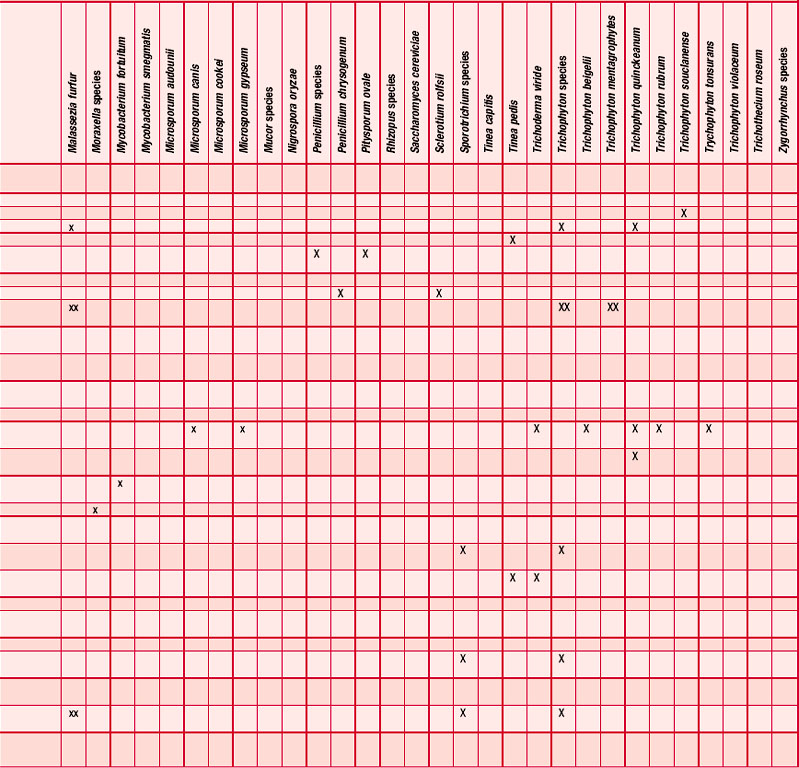
Antifungal
Many essential oils have been reported as having an antifungal effect (Table 4.3) and many investigations have taken place, some more than half a century ago (Schmidt 1936), showing the fungicidal and fungistatic effects of cinnamon, clove, fennel and thyme; these were active against Candida albicans, Sporotrichon and Trichophyton species (Gildemeister & Hoffmann 1956 p. 140). The fungicidal activity of the oil of Chamomilla recutita and its components, including chamazulene and (–)-α-bisabolol, has been well investigated and shown to
Case 4.2 Analgesic (headache)
Case 4.3 Antifungal (Candida albicans)
Intervention
• Citrus bergamia (per.) [bergamot]
• Eucalyptus globulus [blue gum]
• Melaleuca alternifolia [tea tree]
• Zingiber officinale (antispasmodic and laxative)
• Foeniculum vulgare var. dulce (appetite stimulant, laxative and circulation stimulant)
• Mentha x piperita (analgesic, antiinflammatory and stomachic).
be effective against Trichophyton rubrum, T. mentagrophytes, T. tonsurans, T. quinckeanum and Microsporum canis in concentrations of 200 mg/mL (Janssen et al. 1984, 1986, Szalontai, Verzar-Petri & Florian 1976, 1977, Szalontai et al. 1975a,b). Satureia montana has been found to be active against Candida sp. (Pellecuer et al. 1975). A general review of some essential oils with antifungal properties was carried out by Pellecuer et al. (1976) and in other trials a number of compounds found in essential oils, especially the aldehydes and esters, were effective against various fungi, including candida infection (Larrondo & Calvo 1991, Maruzella 1961, Thompson & Cannon 1986). Melaleuca alternifolia has been investigated in vaginal infection with candida and found to be effective (Belaiche 1985, Pena 1962, Shemesh & Mayo 1991). Rosemary, savory and thyme also have antifungal properties (Pellecuer, Roussel & Andary 1973) and Ocimum basilicum has both antifungal and insect-repellant properties (Dube, Upadhyay & Tripath 1989).
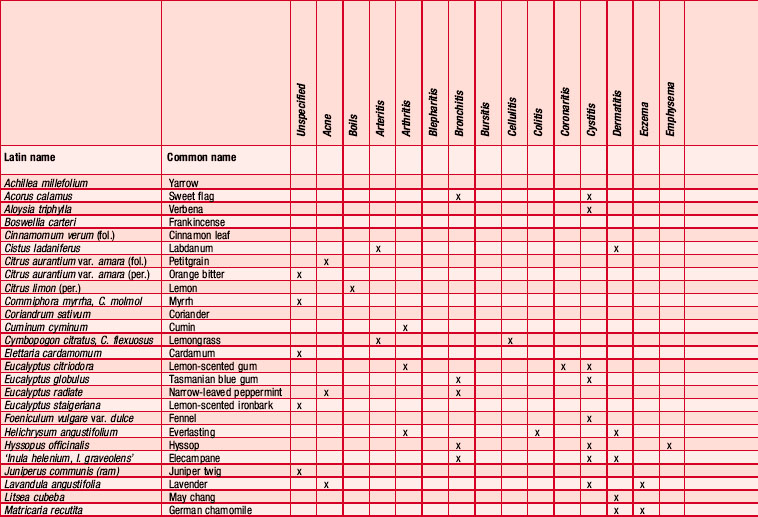
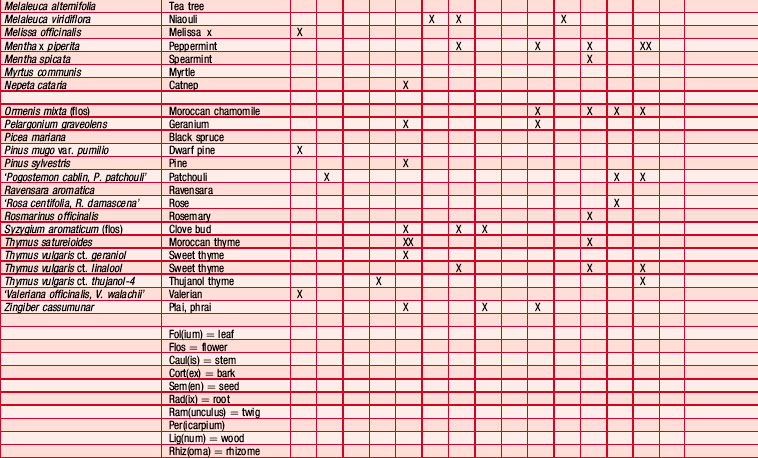
Anti-inflammatory
The oils of Lavandula angustifolia [lavender] and Chamomilla recutita [German chamomile] are widely used to soothe minor inflammations such as sunburn, small burns and insect bites, and plenty of people can testify to their effectiveness in this respect. Jakovlev, Isaac and Flaskamp (1983) showed the anti-inflammatory effect of yarrow, chamomile and turpentine. Although chamazulene and (–)-α-bisabolol found in chamomile oils are anti-inflammatory agents (Weiss 1988 p. 24), other azulenes that may be added to anti-inflammatory preparations are not so effective, e.g. guaiazulene (manufactured from guaiol) and elemazulene (from elemol). Also (+)-α-bisabolol and synthetic (–)-α-bisabolol are not as effective as the natural form.
Otitis media is an infectious and inflammatory disease which may lead to impairment of hearing; over a 2-year period Kang Mok Yoo, an otolaryngologist in South Korea, used aromatherapy to treat 200 patients suffering from chronic mucoid otitis media with effusion and found that the success rate was 90% achieved in just 13 days on average (personal communication) (Table 4.4 and Appendix B Table B1 on the CD-ROM).
Antipruritic
Lavender and tea tree oils (both unspecified) were diluted in jojoba wax and sweet almond oil used in massage in a study to determine the effects of aromatherapy on pruritus and Stratum corneum hydration pruritus in patients undergoing haemodialysis: the results showed pruritus to be significantly decreased and skin hydration greatly enhanced (Ro et al. 2002).
Antitoxic
Chamomile oil has been found to be capable of inactivating toxins produced by bacteria. The amount of oil obtained by distilling 0.1 g of chamomile is sufficient to destroy, within 2 hours, three times that amount of staphylococcal toxins – the highest concentration of toxin so far found in the human organism; streptococcal toxins proved even more sensitive (Weiss 1988 p. 26).
Case 4.4 Anti-inflammatory (gangrene)
Intervention
• 8 drops Eucalyptus globulus [blue gum] – anti-inflammatory, bactericidal, rubifacient
• 8 drops Lavandula angustifolia [lavender] – analgesic, antibacterial, anti-inflammatory, cicatrizant
The foot and leg were then massaged using the following blend:
• 16 drops Juniperus communis fruct. [juniper berry] – analgesic, depurative
• 16 drops Pelargonium graveolens [geranium] – analgesic, antibacterial, anti-infectious, anti-inflammatory, cicatrizant, haemostatic
• 16 drops Eucalyptus globulus – as above
Mr A was given the rest of the blend to apply at home twice a day.
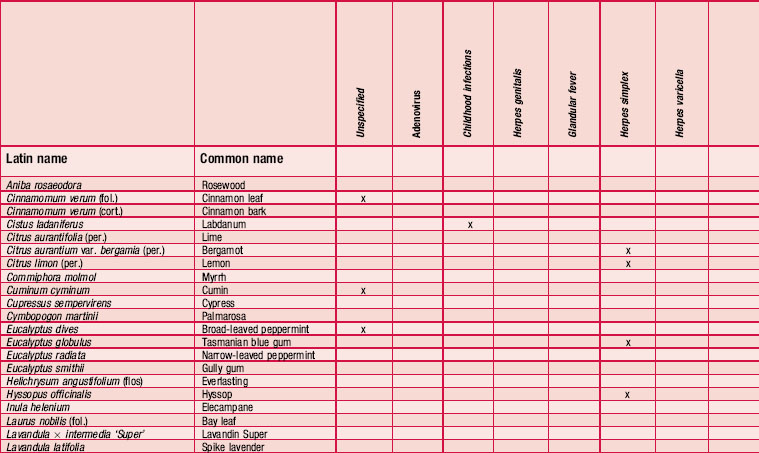
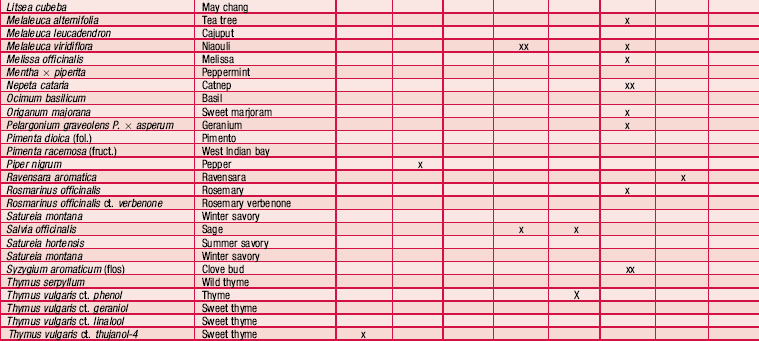
Antiviral
Most people practising aromatherapy have reported success in the control of viruses causing herpes simplex type I, but there is no consistency in the choice of oils used (as can be seen from Table 4.5). Speaking from personal experience, the editors have found the oils Melissa officinalis, Pelargonium graveolens and Eucalyptus smithii to be helpful for herpes simplex I (cold sore). The use of melissa agrees with tests showing this plant to be antiviral (Cohen, Kucera & Herrman 1964, Herrman & Kucera 1967, Kucera & Herrman 1967). For herpes zoster (shingles) the oil of Pelargonium graveolens [geranium] is specifically recommended; it is best applied at the first sign of an attack to prevent virus replication. Used early it prevents blisters from forming and damps down the pain. For herpes simplex II (genital herpes) the many oils suggested include Melaleuca alternifolia [tea tree] and M. viridiflora [niaouli] (Franchomme & Pénoël 2001 pp. 397, 398), but little success has been reported. Despite the lack of
Case 4.5 Antiviral
Intervention
The following essential oils were then chosen and blended:
• Chamaemelum nobile [Roman chamomile] – anti-inflammatory, calming, vulnerary
• Matricaria recutita [German chamomile] – cicatrizant, antiallergic, anti-inflammatory
• Melaleuca alternifolia [tea tree] – analgesic, antiinfectious, anti-inflammatory, antiviral, immunostimulant
• Thymus vulgaris ct. linalol [sweet thyme] – anti-infectious, anti-inflammatory, antiseptic, antiviral, immunostimulant
• Juniperus communis fruct. [juniper berry] – analgesic, antiseptic, antiviral, depurative
These were made up in three ways:
• A 5% concentration with a 95% blend of vegetable carrier oils, also active in the healing process: macerated oils of calendula (60%) and St John’s Wort (25%) and oil of Calophyllum inophyllum (5%). The parents were asked to apply this blend to each boil, using a fine paintbrush.
• A blend of the essential oils above was given to the parents to be used internally – 1 drop blended in honey six times per day.
• 3 drops, diluted in vegetable oil, were put into capsules, to use as suppositories.
A second blend of essential oil was made with equal quantities of:
This was to be applied without dilution to the sole of the each foot six times a day.
Box 4.1 Antiviral (avian and swine flu prevention)
• 4 mL Ravensara aromatica – antibacterial, antiinfectious, antiviral
• 2 mL Eucalyptus radiata – antiinfectious, strong antiseptic, antiviral
• 2 mL Melaleuca viridiflora – antibacterial, antiinfectious, antiviral, immunostimulant
• 2 mL Syzygium aromaticum – antibacterial, antiinfectious, antiviral, immunostimulant.
scientific support, many aromatherapists find that herpes simplex type II and other viral infections such as glandular fever and influenza do respond to essential oil treatment, and there is research to support the use of Piper nigrum [black pepper] (Lembke & Deininger 1988). Cymbopogon flexuosus [lemongrass], Mentha arvensis [cornmint] and Vetiveria zizanioides [vetiver] (Pandey et al. 1988), and Eucalyptus viminalis, E. macarthurii [woolly-butt] and E. dalrympleana appear to be effective both in vitro and in ovo on two strains of influenza virus (Vichkanova, Dzhanashiya & Goryunova 1973). There have been other papers published on this topic in India, Russia and China, and a Swiss patent was filed in 1979 for an antiviral preparation using essential oils.
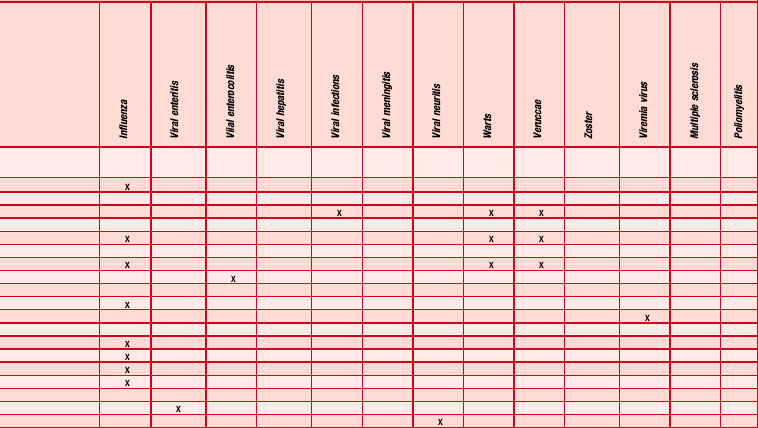
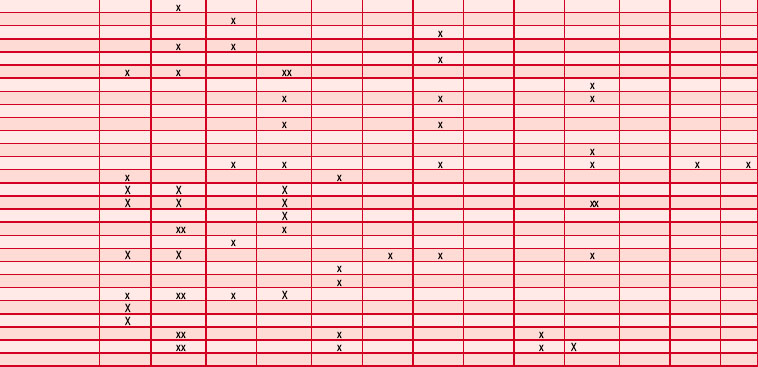
Table 4.5 shows the essential oils that have been recommended for antiviral use. The information has been culled from many sources, which often use only the plant’s common name. Many other oils have been mentioned anecdotally as having antiviral properties, but without specific indications.
Several constituents found naturally in a wide range of essential oils (anethole, β-caryophyllene, carvone, cinnamic aldehyde, citral, citronellol, eugenol, limonene, linalool, linalyl acetate, α-sabinene, γ-terpinene) were found to be active against herpes simplex (Lembke & Deininger 1985, 1988). If the oils are effective it could well be because of some property common to all of them – perhaps lipid solubility. The in vitro studies conducted so far indicate that many essential oils have antiviral properties but that they affect only enveloped viruses and only when they are in a free state, before the virus has entered or is attached to the host cell (e.g. Schnitzler et al. 2008). This is in contrast to the majority of synthetic agents, which either stop complete penetration of viral particles into the host cell or interfere with replication once the virus is inside the cell (Harris 2010 p. 319).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree