45 Parkinson’s disease
Salient features
History
• Tremor: usually unilateral at onset; usually starts in upper limbs. Also seen in the legs and jaws
• Rigidity: ask about history of falls, poor balance, pain and muscle stiffness
• Poverty of movement: ask about drooling of saliva, difficulty in writing (micrographia), difficulty in turning in bed and change in voice (softness of voice)
• Family history of disease (susceptibility genes include α-synuclein, leucine rich repeat kinase 2 and glucocerebrosidase)
• History of smoking (never smokers are twice as likely to develop disease) and caffeine intake (those who take no or very low quantities of daily caffeine, are at increased risk, ~25%) (Lancet 2009;373;2055–66)
• History of exposure to managanese dust, carbon disulfide or carbon monoxide
• Use of 1-Methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) for recreational purposes
• Elicit a drug history, particularly regarding neuroleptics (reserpine, metoclopramide)
• History of herbal medications, particularly Pacific sedative kava kava and Indian snake root Rauwolfia serpentina
• History of severe head injury, encephalitis, hypertension or cerebrovascular disease.
Examination
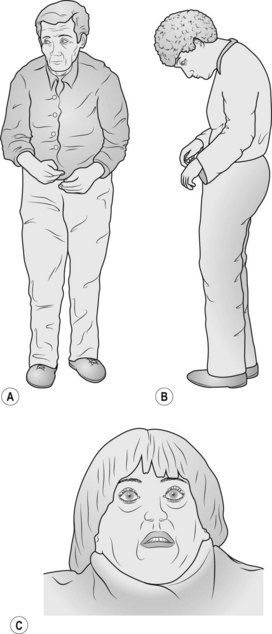
• Comment on the expressionless face, pill-rolling movement and drooling of saliva so that the examiner knows that you have observed these abnormalities. Elicit bradykinesia by asking the patient to touch her thumb with each finger in turn.
• Examine the tone, in particular at the wrist for cog-wheel rigidity.
• Proceed to do the glabellar tap (tap the forehead just above the bridge of the nose repeatedly (about twice per second): in normal subjects, the blinking will stop whereas the patient with Parkinson’s disease continues to blink: referred to as Myerson’s sign. (It must be remembered that this sign is unreliable.)
• Ask the patient to walk and comment on the paucity of movement including the absence of arm swing and festinating gait (the patient walks with a stooped posture as if trying to catch up with her centre of gravity). The feet may scrape the floor in taking steps so the patient trips easily (be prepared to prevent the patient from falling when examining the gait).
• Tell the examiner that you would like to:
• Tell the examiner that you would like to look for:
Questions
What comprises Parkinson’s disease?
• Upper body dyskinesia must be present; it is a symptom complex containing many of the following features:
• Rigidity is usually but not always present:
• Postural instability is usually a late feature
Advanced-level questions
What are the pathological changes in Parkinson’s disease?
The most typical pathological hallmarks of Parkinson’s disease are:
• neuronal loss with depigmentation of the substantia nigra
• Lewy bodies, which are eosinophilic cytoplasmic inclusions in neurons consisting of α-synuclein.
The following associations have been made with clinical features and pathological changes:
| Clinical deficit | Pathology |
|---|---|
| Motor symptoms | Degeneration of dopaminergic nigrostriatal pathway |
| Cognitive defects | Degeneration of dopaminergic mesocortical and mesolimbic pathways |
| Autonomic dysfunction | Dopamine depletion in the hypothalamus |
| ‘Freezing phenomenon’ | Degeneration of the noradrenergic locus ceruleus |
| Dementia | Degeneration of the cholinergic nucleus |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree