Parastomal Hernia
Melissa M. Alvarez-Downing
Susan M. Cera
DEFINITION
Parastomal hernia is defined as an incisional hernia which occurs at the site of or immediately adjacent to an existing ostomy.
DIFFERENTIAL DIAGNOSIS
Abdominal wall mass (tumor, hematoma, abscess)
Eventration of the abdominal wall
PATIENT HISTORY AND PHYSICAL FINDINGS
A thorough history should be obtained to determine the time frame of onset, severity of symptoms, and degree of size change. Patients should also be questioned about their satisfaction with stoma site location because relocation is an option for repair of parastomal hernia.
The most common symptoms associated with an uncomplicated parastomal hernia include bulging near the stoma that worsens with activity and difficulty of adherence of the stoma wafer due to irregularities and bulging of the skin surface. The result is frequent leakages and skin excoriation. In addition, patients complain of the associated expense of increased appliance/wafer usage. Occasionally, wafer leakage may be the presenting complaint and parastomal hernia should be included in the differential diagnosis.
Other symptoms associated with a complication of the parastomal hernia (obstruction, incarceration, and strangulation) include abdominal pain, decreased ostomy output, cramping, nausea, or vomiting.
Characteristic findings on physical exam will render the diagnosis of parastomal hernia in most patients. Examination should be performed with the stoma wafer off with the patient in both the supine and standing position. The patient should be asked to perform a Valsalva maneuver. A characteristic bulge adjacent to the stoma site will be present and confirmed with digital palpation (FIG 1). A search for concomitant hernias should be undertaken, especially at previous laparotomy scars, because these can occur in up to 41% of patients.1
Abdominal tenderness or skin discoloration associated with a nonreducible hernia is indicative of incarceration and/or strangulation and requires urgent/emergent intervention.
IMAGING AND OTHER DIAGNOSTIC STUDIES
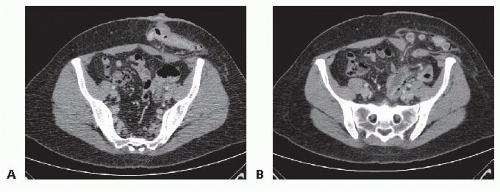
Computed tomography (CT) scan of the abdomen and pelvis performed with intravenous (IV) and oral contrast can confirm the presence of a hernia and help guide operative intervention (FIG 2A,B). Having the patient perform Valsalva during the CT may unmask a hernia and/or reveal the true extent of the hernia. The use of oral contrast will assist in identification of partial or complete obstruction associated with the hernia. The CT scan will also aid in the identification of other associated hernias, that is, at the site of previous laparotomy scars. The size of the neck of the hernia is important and is especially useful in determining the size of the mesh needed in cases where it will be used in the repair. Knowing the contents of the hernia sac (omentum, small bowel, large bowel) preoperatively aids in minimizing bowel injury during surgery because the peritoneum of the hernia sac and bowel serosa can appear similar during dissection. In addition, the planes between the hernia sac and intestine are often distorted by adhesions.
If the stoma was created for inflammatory bowel disease, thorough evaluation of the entire gastrointestinal (GI) tract to evaluate for active disease that may necessitate surgical intervention at the time of the hernia repair is warranted. In addition to endoscopic exams (see below), radiologic testing may include barium small bowel follow-through and capsule endoscopy.
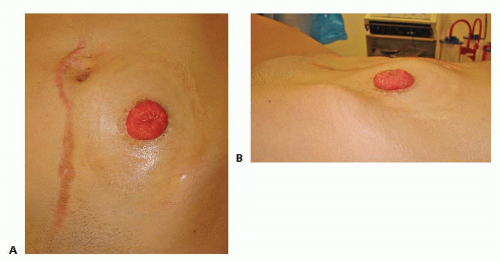 FIG 1 • A,B. Characteristic parastomal bulge seen on physical exam in a patient with a parastomal hernia. |
SURGICAL MANAGEMENT
Preoperative Planning
Patients should be counseled that parastomal hernia is the most frequent complication following the construction of a stoma and can occur in up to 50% of patients because the stoma itself creates a weakened area in the abdominal wall.2
Patients should also be counseled on the various techniques/options available for treatment. Nonsurgical options are appropriate for asymptomatic patients and include use of a hernia belt (secured to the stoma wafer) or an abdominal binder. Surgical intervention is reserved for an enlarging hernia or those associated with symptoms or decreased quality of life because of inadequate stoma pouching. If surgical intervention is considered, the choice of procedure should be tailored to the individuals’ life expectancy, operative risk/benefit analysis, degree of physiologic function (which often corresponds to the degree of weakness of the abdominal wall and ability to successfully sustain repair), and risk of recurrence.
Type of surgical technique chosen is based on patient factors, surgeon experience, and safety of laparoscopic approach.
Risk of initial occurrence and recurrence after repair is associated with obesity and/or weight gain, smoking, emergent intervention, poor nutritional status, immunosuppression, infection, and persistent underlying malignancy or inflammatory bowel disease.
Informed consent should include a possibility of conversion to open in laparoscopic procedures and possible placement of a mesh, particularly in large hernia repairs.
If stoma relocation is planned, preoperative stoma marking for a new stoma site is an important step. Consultation with a stoma nurse is advised. Stoma relocation may include placing the stoma in either of the upper quadrants as opposed to the lower quadrants because less tangential pressure is generated in the upper abdominal wall. This type of placement is also beneficial in morbidly obese patients with a large abdominal wall pannus. Additionally, it is important to explain to patients that the new ostomy site is associated with the same risk of hernia formation.3
In morbidly obese patients, preoperative weight loss can assist with durability of parastomal hernia repair.
Colonoscopy/ileoscopy should be performed to ensure no concomitant lesions are present, which would require simultaneous surgical resection. This can be performed the day prior to planned hernia repair so that the patient can undergo a single bowel preparation.
After obtaining appropriate preoperative medical clearance, a standard bowel preparation with an isoosmotic lavage (polyethylene glycol solution) and oral antibiotics is used for parastomal hernias associated with colostomy. Bowel preparation is not needed for paraileostomy hernias. These patients are instructed to take a liquid diet the day prior to surgery. As with all abdominal surgery, perioperative IV antibiotics should be administered within 1 hour prior to incision and routine venous thromboprophylaxis should be instituted.
Positioning
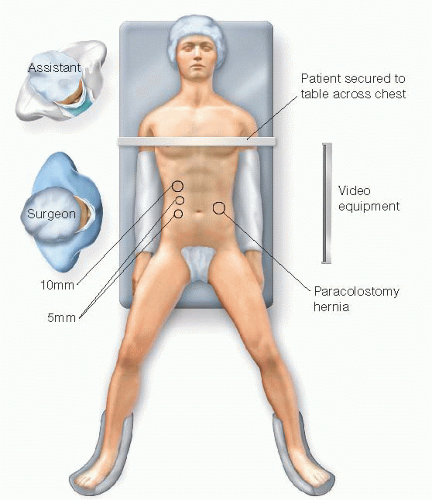
The patient is placed in a modified lithotomy position (FIG 3) for all cases whether open or laparoscopic because of the possibility of encountering extensive adhesions, which may require surgeon repositioning between the patient’s legs. The arm on the working side (opposite the stoma and hernia) should be abducted. Securing the patient to the operative table with use of a bean bag and safety strap or silk tape across the chest is recommended to allow for rotational
adjustment during the procedure if laparoscopic approach is planned.
After induction of general anesthesia, a nasogastric and sterile indwelling bladder catheter are placed. A nasogastric tube (NGT) and inpatient hospitalization is advocated for larger hernia repairs to prevent postoperative vomiting that may result in immediate postoperative disruption of the repair.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree