Category
Histology
Comments
Normal
Absent or inactive septal inflammation
Active inflammation includes blastic lymphocytes and/or eosinophils
Indeterminate for ACR
Active septal inflammation without additional findings
No ductitis or venulitis
Grade I/mild ACR
Active septal inflammation with ductitis or venulitis
And/or 1–2 foci per lobule of acinar inflammation
Absent/minimal acinar injury
Grade II/moderate ACR
Minimal intimal arteritis (<25 % luminal compromise)
And/or multiple foci (≥3 foci/lobule) of acinar inflammation with individual cell injury
No confluent or diffuse inflammation
Requires differentiation from AMR
Grade III/severe ACR
Diffuse acinar inflammation with focal or diffuse confluent acinar cell necrosis
And/or moderate to severe intimal arteritis
And/or necrotizing arteritis
Requires differentiation from AMR
8.1.1 Normal Pancreas
The normal pancreas shows absent to sparse inflammatory infiltrates, confined to the fibrous septa without involvement of septal structures. The fibrous septa are proportional to the size of the associated duct and vessels.
8.1.2 Indeterminate for Rejection
Focal active septal inflammation is present; however, the overall features do not fulfill the criteria for mild ACR
8.1.3 Grade I (Mild)
Active inflammation, including activated blastic lymphocytes and/or eosinophils, involving septal structures is present. This inflammatory infiltrate may be variable. Foci of venulitis are seen, which is characterized by circumferential lymphocytic/inflammatory accumulation in the subendothelium with associated endothelial injury (Figs. 8.1 and 8.2). Ductal injury (ductitis) should also be present and will show lymphocytic or eosinophilic inflammation within the ductal epithelium. As a result of the inflammatory infiltrate, the ductal epithelial cells often show irregular spacing of the nuclei, anisonucleosis, and reactive changes (Fig. 8.3). Denudation of the epithelial cells may also be seen. The presence of venulitis or ductitis is sufficient for the diagnosis of mild ACR. In the absence of venulitis and ductitis, mild ACR may be diagnosed by the presence of focal acinar inflammation, limited to no more than two inflammatory foci per lobule with absent to minimal acinar cellular injury or dropout (Fig. 8.4).
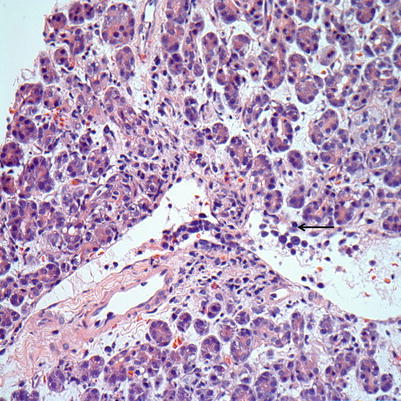
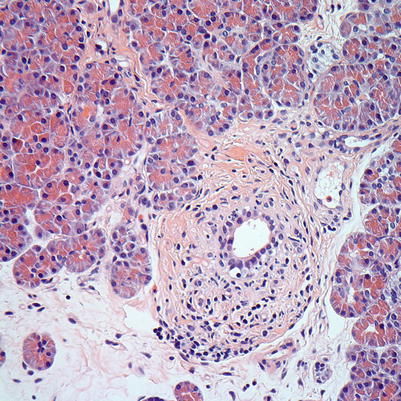
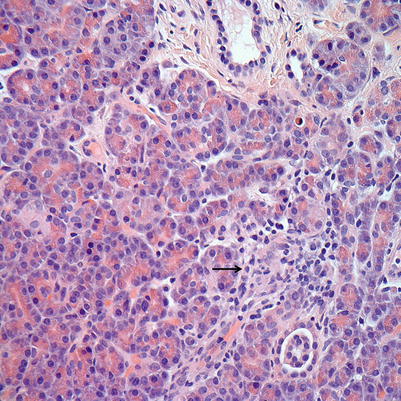
Fig. 8.1
(a, b) Mild ACR. (a) Interlobular septa show inflammation including activated blastic lymphocytes, plasma cells, eosinophils, and rare neutrophils. (b) The inflammatory infiltrate may be rich in eosinophils
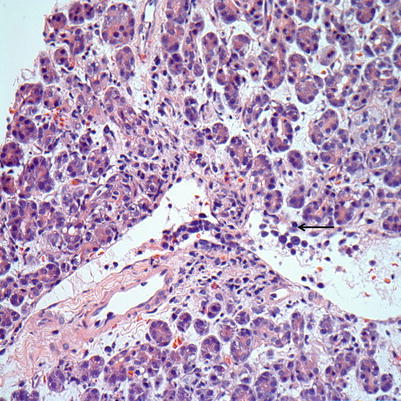
Fig. 8.2
Mild ACR. Septal vein shows venulitis with subendothelial accumulation of lymphocytes, activated blastic lymphocytes, and endothelial cell lifting and damage (arrow)
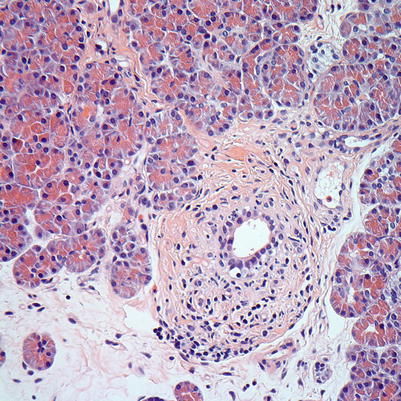
Fig. 8.3
Mild ACR. Interacinar duct with infiltration by lymphocytes and epithelial injury. The ductal epithelium shows cytoplasmic vacuolization, irregular nuclear spacing, and scattered apoptotic nuclei
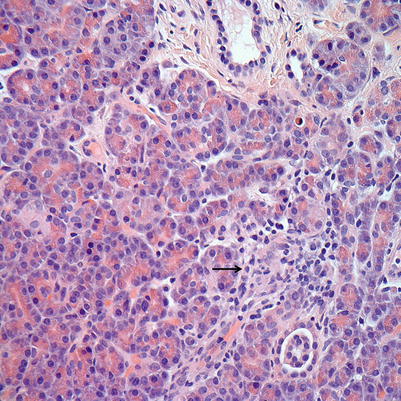
Fig. 8.4
Mild ACR. Spotty acinar inflammation and injury with minimal (arrow) to absent acinar dropout. These findings in isolation may also be diagnostic of mild ACR
8.1.4 Grade II (Moderate)
In addition to the histological findings of mild rejection, moderate ACR includes the finding of multifocal acinar inflammation (three or more foci per lobule) with individual acinar cell injury/dropout (Fig. 8.5). Alternatively, the diagnosis of moderate ACR may be defined by the presence of mild intimal arteritis, which is characterized by rare or occasional subendothelial inflammation by mononuclear cells without activation of or damage to the overlying arterial endothelium. The extent of the arteritis should compromise less than 25 % of the vessel lumen (Fig. 8.6).
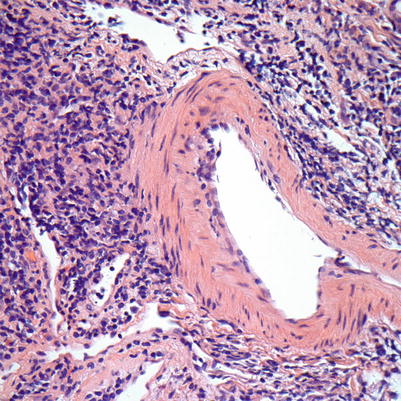
Fig. 8.5
(a, b) Moderate ACR. (a) Septal inflammation with lymphocytes, plasma cells, and rare eosinophils. (b) Focal acinar inflammation with spotty multifocal acinar injury/dropout (arrows). Septal venulitis is also identified
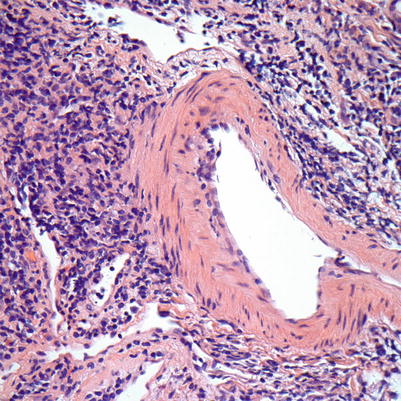
Fig. 8.6
Moderate ACR. Intimal arteritis with mononuclear cells in the subendothelium of this muscular artery. There is focal endothelial swelling and lifting/damage. The damage seen occupies less than 25 % of the arterial lumen
8.1.5 Grade III (Severe)
Severe ACR is characterized by diffuse acinar inflammation (confluent) with associated focal or diffuse confluent acinar cell necrosis. Interstitial edema and hemorrhage are characteristic of severe tissue damage. There should be no significant acinar tissue present without inflammatory infiltrate. Severe ACR may also be diagnosed by moderate to severe intimal arteritis, in which mononuclear cells are seen within the intima of a muscular artery with evidence of injury. This injury can manifest as endothelial cell activation or sloughing, margination of neutrophils, macrophage activation, proliferation of myofibroblasts within the intima, and fibrin leakage. Greater than 25 % of the vessel lumen should be compromised by the injury. Necrotizing arteritis, with focal or circumferential fibrinoid necrosis, may be seen with or without transmural inflammation. This finding can also be seen in AMR and should raise this possibility.
8.2 Antibody-Mediated Rejection
8.2.1 Hyperacute Rejection
This type of rejection is immediate graft rejection (within 1 h) due to preformed antibodies in the recipient serum. The histological findings include edema, acinar cell injury with vacuolization, degranulation, and spotty necrosis. Neutrophilic margination in capillaries and veins may be seen. In later stages, hemorrhagic necrosis is seen throughout the graft. Widespread fibrinoid vascular necrosis and thrombosis are present. C4d staining is seen throughout graft vasculature.
8.2.2 Accelerated AMR
Accelerated AMR is similar to hyperacute rejection, but occurs hours to days after transplantation.
8.2.3 Acute AMR
The diagnosis of acute AMR involves the combination of three criteria. These criteria include laboratory-confirmed circulating donor-specific antibodies (DSA), morphological evidence of tissue injury (see grading criteria later), and C4d positivity in interacinar capillaries (>5 % of acinar lobular surface) by immunostaining. When three of three criteria are met, the findings are diagnostic of AMR. If two of three criteria are met, the findings are consistent with AMR. If only one of three criteria is met, the finding requires exclusion of AMR. The grading of AMR is based on the histological features seen in the biopsy material (Table 8.2).
Table 8.2




Histological grading of AMR in pancreas transplant biopsies [12]
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


