Palisaded Myofibroblastoma
L. Jeffrey Medeiros, MD
Key Facts
Terminology
Intranodal palisaded myofibroblastoma
Synonyms
Intranodal hemorrhagic spindle-cell tumor with amianthoid fibers
Myofibroblastoma
Clinical Issues
Rare benign tumor of probable myofibroblastic origin
Almost always involves inguinal lymph nodes
Excision is curative
Macroscopic Features
Well encapsulated
Microscopic Pathology
Crisscrossed fascicles of parallel, slender, spindled cells
Often display palisading pattern
Can resemble Antoni type A areas of schwannoma
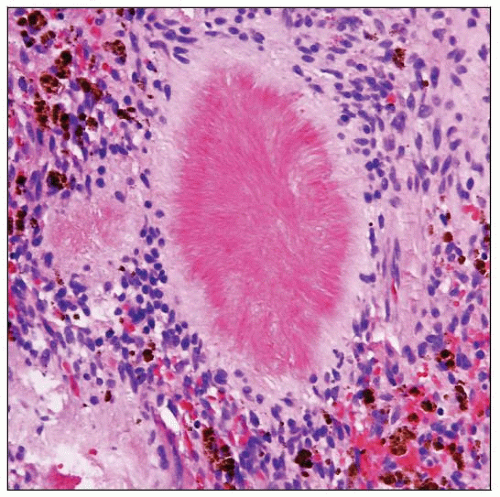
Mats of eosinophilic material (amianthoid fibers)
Stellate or circular shapes depending on plane of section
Homogeneous, deeply eosinophilic
Ancillary Tests
Immunohistochemistry
Actin-sm(+), myosin(+)
Vimentin(+), Cyclin-D1(+/-)
Desmin(-), S100(-), HMB-45(-), CD34(-), CD117(-)
Top Differential Diagnoses
Schwannoma
Angiomyomatous hamartoma
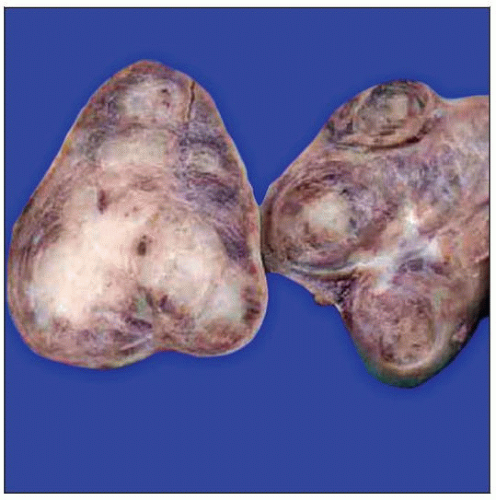 A fixed excisional lymph node biopsy specimen shows replacement by palisaded myofibroblastoma. Note the central gray-white areas and subcapsular hemorrhage (“milk freshly poured into tea”). |
TERMINOLOGY
Abbreviations
Palisaded myofibroblastoma (PM)
Synonyms
Intranodal palisaded myofibroblastoma
Intranodal hemorrhagic spindle cell tumor with amianthoid fibers
Myofibroblastoma
Definitions
Benign tumor of probable myofibroblastic origin that almost always arises in inguinal lymph nodes
Minority view suggests smooth muscle origin (from vessels or capsule)
ETIOLOGY/PATHOGENESIS
Acquired Abnormality
Inguinal lymph nodes have increased numbers of myofibroblasts compared with other lymph nodes
May be related to increased lymphatic drainage at this site
Predisposes to benign proliferation of myofibroblastic cells
CLINICAL ISSUES
Epidemiology
Incidence
Rare tumor; approximately 50 cases reported in literature
Age
Wide age range: 19-71 years
Median: 6th decade
Gender
Slight male predominance (M:F = 4:1)
Ethnicity
No ethnic preference reported
Presentation
Painful mass
Unilateral; no side preference
Unicentric; rare multicentric cases reported
Almost all cases arise in inguinal lymph nodes
Located deeply; under inguinal ligament
Overlying skin is not involved
Rare cases reported in submandibular or cervical lymph nodes
Treatment
Surgical approaches
Excision is curative
No additional therapy required
Prognosis
Excellent
Benign lesion
Only 2 cases have recurred locally and needed reexcision
Recurrence at 6 years and 9 years
MACROSCOPIC FEATURES
General Features
Size: Range 0.6-5.0 cm in greatest dimension
Well encapsulated
Cut surface is gray-white and nodular with subcapsular hemorrhage
Likened to “milk freshly poured into tea”
MICROSCOPIC PATHOLOGY
Histologic Features
Often nodular pattern at low power
Surrounded by pseudocapsule
Uninvolved lymph node parenchyma often compressed
Crisscrossed fascicles of parallel, slender, spindled cells
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree