Patient Story
A 39-year-old woman presented to her physician with a malodorous vaginal discharge. On exam, a thin white discharge was seen covering the introitus (Figure 80-1). A speculum exam revealed a thin whitish gray discharge and a distinct fishy odor. The pH of the discharge was 4.6, and 40% of the epithelial cells on her wet prep were clue cells (Figure 80-2). She was diagnosed with bacterial vaginosis and treated with oral metronidazole.
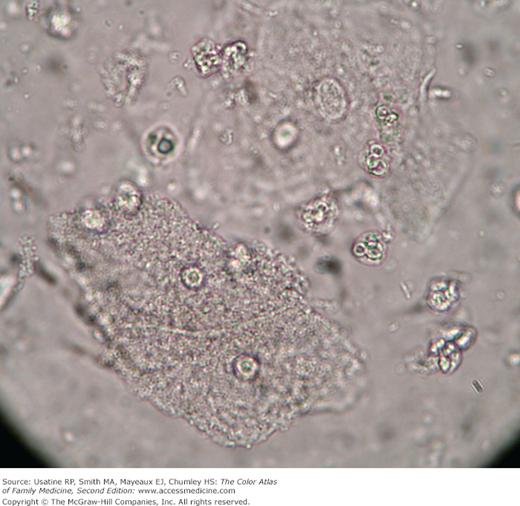
Figure 80-2
A wet mount of vaginal discharge in saline under high-power light microscopy. Note the presence of vaginal epithelial cells, smaller white blood cells (polymorphonucleocytes), and bacteria. The bacteria are the coccobacilli of Gardnerella vaginalis covering the cell membranes of the two vaginal epithelial cells near the lower end of the field. These are clue cells seen in patients with bacterial vaginosis. (Courtesy of Richard P. Usatine, MD.)
Introduction
Vaginal discharge is a frequent presenting complaint in primary care. The three most common causes are bacterial vaginosis, candidiasis, and trichomoniasis. However, a significant number of patients with vaginal discharge will have some other condition, such as atrophic vaginitis. Providers must refrain from “diagnosing” a vaginitis based solely on the color and consistency of the discharge, as this may lead to misdiagnosis and may miss concomitant infections.1
Epidemiology
The reported rates of chlamydia and gonorrhea are highest among females ages 15 to 19 years. Adolescents are at greater risk for sexually transmitted diseases (STDs) because they frequently have unprotected intercourse, are biologically more susceptible to infection, are often engaged in partnerships of limited duration, and face multiple obstacles to utilization of health care.1
Etiology and Pathophysiology
- The quantity and quality of normal vaginal discharge in healthy women vary. Physiologic leukorrhea refers to generally nonmalodorous, mucousy, white or yellowish vaginal discharge in the absence of a pathologic cause. It is not accompanied by signs and symptoms, such as pain, pruritus, burning, erythema, or tissue friability. However, slight malodor and irritative symptoms can be normal for some women at certain times.2 Physiologic leukorrhea is usually a result of estrogen-induced changes in cervicovaginal secretions.
- Noninfectious causes of vaginitis include irritants (e.g., scented panty liners, spermicides, povidone-iodine, soaps and perfumes, and some topical drugs) and allergens (e.g., latex condoms, topical antifungal agents, chemical preservatives) that produce hypersensitivity reactions.
- Before starting an examination, determine whether the patient douched recently, because this can lower the yield of diagnostic tests and increase the risk of pelvic inflammatory disease.3 Patients who have been told not to douche will sometimes start wiping the vagina with soapy washcloths, which also irritates the vagina and cervix and may cause a discharge. Douching is associated with increases in bacterial vaginosis and acquisition of sexually transmitted infections when exposed. However, recent studies indicate that douching with plain water once a week or less did not disturb normal flora.4,5
- There are many causes of vaginitis in humans. Infectious causes include bacterial vaginosis (40% to 50% of cases) (see Figures 80-1 and 80-2), vulvovaginal candidiasis (20% to 25%), and trichomonas (15% to 20%) (Figure 80-3).6 Less common causes include atrophic vaginitis, foreign body (especially in children), cytolytic or desquamative inflammatory vaginitis, streptococcal vaginitis, ulcerative vaginitis, and idiopathic vulvovaginal ulceration associated with HIV infection.
- Rarer noninfectious causes include chemicals, allergies, hypersensitivity, contact dermatitis, trauma, postpuerperal atrophic vaginitis, erosive lichen planus, collagen vascular disease, Behçet syndrome, and pemphigus syndromes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree