A. Structure–Activity Relationships
1. Modifications of structure, such as introduction of a double bond in prednisolone and prednisone, have resulted in synthetic corticosteroids with more potent glucocorticoid effects than the two closely related natural hormones, cortisol and cortisone, respectively (Table 40-1).
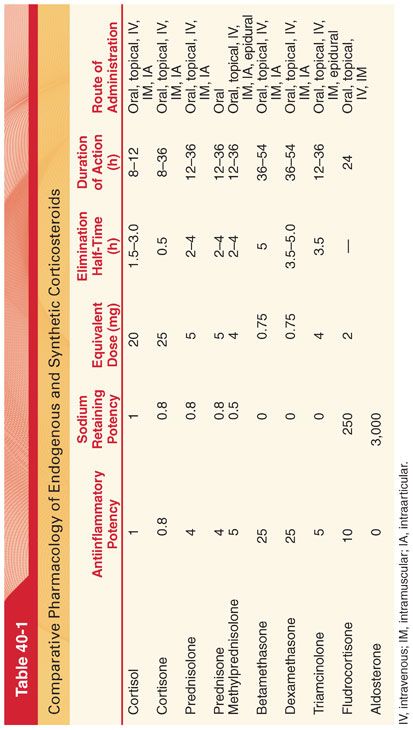
2. At the same time, mineralocorticoid effects and the rate of hepatic metabolism of these synthetic drugs are less than those of the natural hormones.
B. Mechanism of Action
1. Glucocorticoids attach to cytoplasmic receptors to enhance or suppress changes in the transcription of DNA and thus the synthesis of proteins. Glucocorticoids also inhibit the secretion of cytokines via posttranslational effects.
2. Mineralocorticoid receptors are present in distal renal tubules, colon, salivary glands, and the hippocampus. In contrast, glucocorticoids receptors are more widely distributed and do not bind aldosterone making these receptors glucocorticoid-selective.
C. Maintenance of Homeostasis. Permissive and protective effects of glucocorticoids are critical for the maintenance of homeostasis during severe stress.
1. Permissive actions of glucocorticoids occur at low physiologic steroid concentrations and serve to prepare the individual for responding to stress.
2. Protective actions of glucocorticoids occur when high plasma concentrations of steroids exert antiinflammatory and immunosuppressive effects. This protective response prevents the host-defense mechanisms that are activated during stress from overshooting and damaging the organism.
D. Pharmacokinetics
1. Synthetic cortisol and its derivatives are effective orally (see Table 40-1).
2. Water-soluble cortisol succinate can be administered intravenously (IV) to achieve prompt increases in plasma concentrations. More prolonged effects are possible with intramuscular (IM) injection.
3. Cortisone acetate may be given orally or IM but cannot be administered IV. The acetate preparation is a slow-release preparation lasting 8 to 12 hours. After release, cortisone is converted to cortisol in the liver.
4. Corticosteroids are also promptly absorbed after topical application or aerosol administration.
III. Synthetic Corticosteroids (see Table 40-1) (Figs. 40-1 and 40-2).
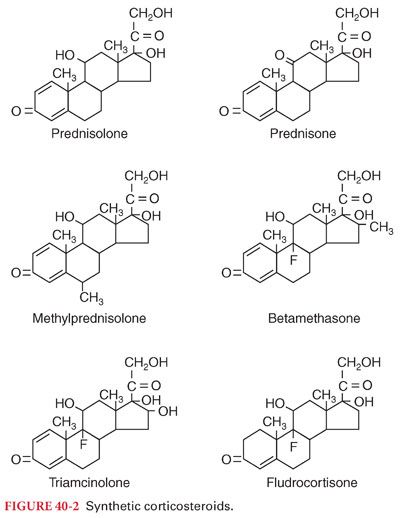
A. Prednisolone is an analogue of cortisol that is available as an oral or parenteral preparation. The antiinflammatory effect of 5 mg of prednisolone is equivalent to that of 20 mg of cortisol. Cortisol and prednisone are suitable for sole replacement therapy in adrenocortical insufficiency because of the presence of glucocorticoid and mineralocorticoid effects.
B. Prednisone is rapidly converted to prednisolone after its absorption from the gastrointestinal tract (antiinflammatory effect and clinical uses are similar to those of prednisolone).
C. Methylprednisolone is the methyl derivative of prednisolone. The antiinflammatory effect of 4 mg of methylprednisolone is equivalent to that of 20 mg of cortisol. The acetate preparation administered intraarticularly has a prolonged effect.
D. Betamethasone is a fluorinated derivative of prednisolone. The antiinflammatory effect of 0.75 mg is equivalent to that of 20 mg of cortisol. Betamethasone lacks the mineralocorticoid properties of cortisol (not acceptable for sole replacement therapy in adrenocortical insufficiency).
E. Dexamethasone is a fluorinated derivative of prednisolone and an isomer of betamethasone. The antiinflammatory effect of 0.75 mg is equivalent to that of 20 mg of cortisol. This corticosteroid is commonly chosen to treat certain types of cerebral edema.
F. Triamcinolone is a fluorinated derivative of prednisolone. The antiinflammatory effect of 4 mg is equivalent to that of 20 mg of cortisol. The hexacetonide preparation injected intraarticularly may provide therapeutic effects for 3 months or longer.
1. This drug is often used for epidural injections in the treatment of lumbar disk disease.
2. An unusual adverse side effect of triamcinolone is an increased incidence of skeletal muscle weakness. Anorexia rather than appetite stimulation, and sedation rather than euphoria may accompany administration of triamcinolone.
IV. Clinical Uses. The only universally accepted clinical use of corticosteroids and their synthetic derivatives is as replacement therapy for deficiency states. The safety of corticosteroids is such that it is acceptable to administer a single large dose in a life-threatening situation on the presumption that unrecognized adrenal or pituitary insufficiency may be present. Prednisolone or prednisone are recommended when an antiinflammatory effect is desired (antiinflammatory effect of corticosteroids is palliative because the underlying cause of the response remains yet suppression of the inflammatory response may be lifesaving in some situations). Masking of the symptoms of inflammation may delay diagnosis of life-threatening illness, such as peritonitis due to perforation of a peptic ulcer.
A. Deficiency States
1. Acute adrenal insufficiency requires electrolyte and fluid replacement as well as supplemental corticosteroids (cortisol is administered at a rate of 100 mg IV every 8 hours after an initial injection of 100 mg).
2. Management of chronic adrenal insufficiency in adults is with the daily oral administration of cortisone, 25.0 to 37.5 mg. A typical regimen is 25.0 mg in the morning and 12.5 mg in the late afternoon (mimics the normal diurnal cycle of adrenal secretion).
B. Allergic Therapy. Topical corticosteroids are capable of potent antiinflammatory effects and are the mainstay of allergic therapy. Unlike antihistamines that provide pharmacologic effects within 1 to 2 hours, topical corticosteroids may require 3 to 5 days of treatment to produce a therapeutic effect.
C. Asthma is an inflammatory disease of the lungs and inhaled glucocorticoids are often recommended as first-line therapy for controlling the symptoms.
1. Inhaled glucocorticoids have oropharyngeal side effects that include dysphonia and candidiasis.
2. Parenteral corticosteroids are important in the emergent preoperative preparation of patients with active reactive airway disease and in the treatment of intraoperative bronchospasm. Doses equivalent to 1 to 2 mg/kg of cortisol (or the equivalent dose of prednisolone) are commonly recommended. Preoperative corticosteroid administration 1 to 2 hours before induction of anesthesia is important because the beneficial effects of corticosteroids may not be fully manifest for several hours.
D. Antiemetic Effect
1. Dexamethasone prevents postoperative nausea and vomiting only when administered near the beginning of surgery, probably by reducing surgery-induced inflammation due to inhibition of prostaglandin synthesis.
2. Administration of higher doses (8 to 10 mg) of dexamethasone has a similar antiemetic effect to lower doses (4 to 5 mg). Dexamethasone is also effective in suppressing chemotherapy-induced nausea and vomiting.
E. Postoperative Analgesia
1. Glucocorticoids peripherally inhibit phospholipase enzyme that is necessary for the inflammatory chain reaction along both the cyclooxygenase and lipoxygenase pathways. As a result, glucocorticoids may be effective in decreasing postoperative pain but with a different side effect profile than nonsteroidal antiinflammatory drugs.
2. Perioperative IV dexamethasone at doses more than 0.1 mg/kg decreases acute postoperative pain and reduces opioid use, especially when administered preoperatively.
F. Cerebral Edema
1. Corticosteroids in large doses are of value in the reduction or prevention of vasogenic cerebral edema and the resulting increases in intracranial pressure that may accompany intracranial tumors and metastatic lesions and bacterial meningitis.
2. Dexamethasone, with minimal mineralocorticoid activity, is frequently selected to decrease cerebral edema and associated increases in intracranial pressure.
3. The administration of glucocorticoids to patients with severe head injury, cerebral infarction, and intracranial hemorrhage is not useful.
G. Aspiration Pneumonitis. Despite the absence of confirming evidence that corticosteroids are beneficial, it is not uncommon for the treatment of aspiration pneumonitis to include the empiric use of pharmacologic doses of these drugs.
H. Lumbar Disk Disease
1. An alternative to surgical treatment of lumbar disk disease is the epidural placement of corticosteroids. Corticosteroids may decrease inflammation and edema of the nerve root that has resulted from compression.
2. A common regimen is epidural injection of 25 to 50 mg of triamcinolone, or 40 to 80 mg of methylprednisolone, in a solution containing lidocaine at or near the interspace corresponding to the distribution of pain.
3. Injection of triamcinolone, 80 mg, into the lumbar epidural space of patients with lumbar disk disease results in acute suppression of plasma concentrations of adrenocorticotropic hormone (ACTH) and cortisol. Exogenous corticosteroid coverage during this potentially vulnerable (<1 month) period should be considered in patients undergoing major stress
I. Immunosuppression
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


