Osteoblastoma
G. Petur Nielsen, MD
Andrew E. Rosenberg, MD
Key Facts
Clinical Issues
Benign bone-forming neoplasm > 2 cm in dimension
Diagnosed in young adults with male predominance of 2:1
Commonly arises in tubular bones and posterior elements of spinal column
Presents with pain and swelling, with neurologic symptoms in some spinal lesions
Treated by curettage or en bloc excision
Excellent prognosis with local recurrence rate of 20%
Image Findings
Expansile well-defined mixed lytic and blastic mass with sclerotic margins
Macroscopic Features
Well-circumscribed, gritty, tan-white, dark red mass
Usually 2-5 cm in size
Microscopic Pathology
Sharply demarcated from adjacent preexisting and reactive bone
Composed of haphazardly interconnecting trabeculae or sheet-like aggregates of woven bone rimmed prominently by metabolically active osteoblasts
Intertrabecular tissue consists of loose, richly vascular connective tissue
Variants contain cartilage, epithelioid osteoblasts, degenerative nuclear changes, and aneurysmal bone cyst-like changes
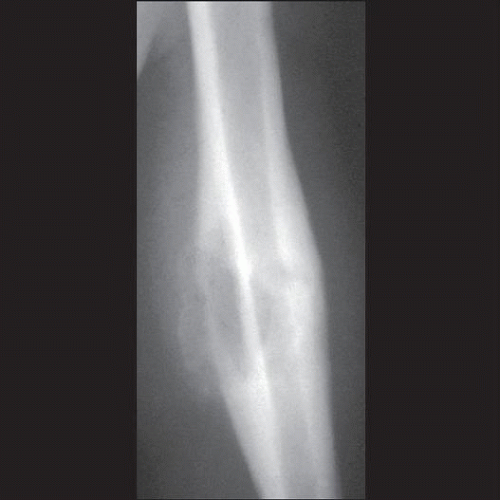 Radiograph of humerus shows a lytic osteoblastoma of the mid shaft surrounded by solid periosteal new bone. It extends into periosseous soft tissues where cloud-like neoplastic ossification is noted. |
TERMINOLOGY
Abbreviations
Osteoblastoma (OB)
Synonyms
Giant osteoid osteoma
Definitions
Benign bone-forming neoplasm composed of woven bone trabeculae lined by osteoblasts
Tumor > 2 cm in dimension
ETIOLOGY/PATHOGENESIS
Etiology
Cause unknown; not associated with any syndrome; no specific cytogenetic abnormality
CLINICAL ISSUES
Epidemiology
Incidence
Uncommon; accounts for 1% of primary bone tumors
Responsible for 3% of primary benign bone tumors
Age
Diagnosed in adolescents and young adults (2nd-4th decade)
75% younger than 25 years old at diagnosis
Mean age: 20 years
Gender
Males affected more frequently than females (2:1)
Site
Most commonly arise in tubular bones
Approximately 60% develop in appendicular skeleton
Frequently involve metadiaphyseal region of tubular bones
Centered in cortex and surface in 65% and located in medullary cavity in 35% of cases
12% occur in femur; 10% originate in tibia; 9% involve bones of foot and ankle
Axial skeleton frequently affected
30% arise in spinal column
Originate in posterior elements, especially lamina and pedicles; vertebral body involvement occurs secondarily
Cervical > lumbar > thoracic > sacral
Craniofacial bones involved in 10% of cases
Mandible most common location
Presentation
Pain, swelling, decreased range of motion
Tumors located in spine can cause neurological symptoms
Numbness, tingling, paraparesis, paraplegia
Small percentage associated with systemic “toxic” symptoms
Treatment
Curettage or selective en bloc resection
Radiation when located in inaccessible site
Prognosis
Curettage associated with local recurrence in approximately 20% of cases
Aggressive variant behaves similar to conventional type
Malignant transformation in osteoblastoma is exceptionally rare
IMAGE FINDINGS
Radiographic Findings
MR Findings
Well-delineated mass that is low to intermediate signal intensity on T1 and intermediate to high signal intensity on T2
Mineralized areas manifest as signal void (dark)
Tumor and edema enhance with contrast
CT Findings
Expansile lytic and sclerotic mass with circumscribed margins and surrounding reactive bone
Bone Scan
Intense uptake on scintography
MACROSCOPIC FEATURES
General Features
Solitary, well-circumscribed, tan-white, dark red, gritty
Rarely multifocal/multicentric
Cystic changes (aneurysmal bone cyst-like changes) prominent in 10% of cases
Delineated from soft tissues by periosteal shell of reactive bone
Size
Tumors range from 2-20 cm in dimension
Most tumors are 3-5 cm
MICROSCOPIC PATHOLOGY
Microscopic Features
Sharply demarcated
Neoplastic woven bone trabeculae deposited in haphazard, interconnecting, or sheet-like patterns
Bone rimmed by osteoblasts and scattered osteoclasts
Osteoblasts are ovoid or round, with moderate amounts of eosinophilic or purple cytoplasm, and eccentric nuclei with fine chromatin
Vascular connective tissue fills intertrabecular space
Scattered mitoses with no atypical forms
Necrosis usually absent or focal
Occasional cystic change mimicking aneurysmal bone cyst
Tumors composed of 75% epithelioid osteoblasts known as aggressive osteoblastoma
Epithelioid osteoblasts are large and polyhedral with abundant eosinophilic cytoplasm, vesicular nucleus, and prominent nucleolus
Cartilaginous variant (5%) contains well-formed hyaline cartilage
Pseudomalignant type contains osteoblasts with large, hyperchromatic, vacuolated nuclei that represent degenerative changes
DIFFERENTIAL DIAGNOSIS
Osteoid Osteoma
< 2 cm; characteristic clinical symptoms
Aneurysmal Bone Cyst
No haphazardly joining trabeculae of woven bone
Osteoblastoma-like Osteosarcoma
Grows with infiltrative pattern
DIAGNOSTIC CHECKLIST
Pathologic Interpretation Pearls
Tumor is well demarcated and neoplastic bone is rimmed by osteoblasts
SELECTED REFERENCES
1. Berry M et al: Osteoblastoma: a 30-year study of 99 cases. J Surg Oncol. 98(3):179-83, 2008
Image Gallery
Imaging Features
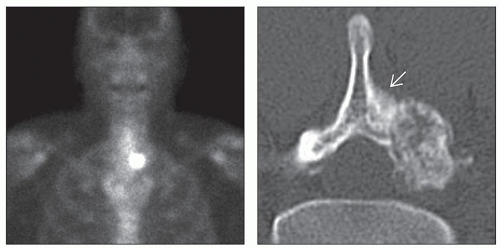 (Left) AP bone scan shows a small oval focus of intense isotope uptake on the left of T2. (Right) CT scan through osteoblastoma of pedicle and lamina of the vertebra demonstrates a well-circumscribed, expansile, oval mass, which contains substantial internal fine ossification. The tumor impinges upon the spinal canal. Thick periosteal reaction is present along the surface of the lamina and the base of the spinous process
 . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
