INTRODUCTION
Improvements in implant design and materials have been responsible for significant advances in our ability to treat patients with complex orthopedic problems. Like all medical fields, orthopedic surgery has become a group of subspecialized fields in recent years.
Varus and valgus are descriptive terms frequently used for the characterization of angular musculoskeletal deformities. They refer to the direction of the apex of the deformity in relation to the midline of the body. When the apex points away from the midline, the deformity is termed varus; when the apex points toward the midline, the deformity is termed valgus. Knock-knees is an example of a valgus deformity, such that the apex is defined by the patient’s knees pointing toward the body’s midline. Conversely, “bow-legged” is an example of a varus deformity. These terms can also be applied to fractures such that the apex of the deformity is the fracture itself. Comminution describes a fracture that is significantly fragmented. A fracture is displaced when the main bony fragments are translated or separated from each other. Displacement can further be subcategorized into minimally, moderately, or completely displaced.
Open fractures define fractures with overlying wounds such that the fracture is exposed to the external environment. Open fractures can be obvious in significant trauma with substantial degloving of the soft-tissues, or they can be more subtle where only a small poke hole is visible with draining fracture hematoma. As a result, when patients are transferred from other hospitals or urgent care facilities, all splints should be removed, and the skin overlying all fractures must be carefully inspected for open injury. Open fractures are orthopedic emergencies and must be addressed with prompt surgical debridement and irrigation to minimize the subsequent development of infection and associated fracture nonunions.
Joint dislocations also warrant immediate treatment. Reduction refers to the maneuver used to restore proper alignment of a joint or fracture. Vascular structures spanning the joint or fracture may be damaged at the time of injury. Alternatively, these structures may be compressed or kinked due to the resulting deformity. Arterial pulses should always be assessed distal to a musculoskeletal injury and carefully documented. Often absent pulses are restored with reduction of a joint or fracture. If reduction does not successfully return pulses, the vessels are likely torn; early repair and reconstruction is often required to restore distal circulation to the limb. Vascular injuries repaired prior to fracture or joint reduction and stabilization, may be in danger of subsequent failure due to bony instability. Orthopedists can quickly stabilize fractures and dislocations using external fixation, providing a stable scaffold on to which necessary vascular repairs can be made.
Joint or fracture reduction may be treated by open or closed techniques. A dislocation or fracture is described as unstable if there is a high likelihood of subsequent deformation after reduction is performed. Following reduction, unstable fractures or dislocations may be stabilized by closed or open means. Closed treatment may involve traction, casts, splints, or braces; open techniques involve surgical exposure of the fracture or joint and reduction followed by maintenance of the reduction with internal or external fixation devices. The surgical treatment of an unstable fracture or dislocation is therefore described as “Open reduction with internal or external fixation.”
Splinting and casting are noninvasive ways of stabilizing fractures and maintaining reductions. Splints are typically made of plaster and are not circumferential, while casts are circumferential and can be made of either plaster or fiber-glass. Splints are best used for a short period of time (days up to one or two weeks) in acute scenarios shortly after injury or after an operation when swelling is a concern to avoid compartment syndrome. Casts are sturdier, used to maintain bones in appropriate alignment for extended periods of time (weeks to a few months). For example, a distal radius fracture may be reduced and placed in a sugar-tong splint with follow-up in clinic. At clinic follow-up, if the reduction is adequate and swelling has subsided, the splint can be overwrapped in a cast or transitioned to a new cast for continued closed treatment. After ankle fractures are surgically fixed with open reduction and internal fixation, they are often placed in a short-leg splint with stirrups postoperatively, followed by transitioning to short-leg cast for 4-6 weeks to protect the operative repair. There are many types of splints and casts depending on the type of injury being treated. Examples of splints include the volar forearm, sugar-tong, long-arm posterior, double sugar-tong, coaptation, short leg posterior with or without stirrups, and long-leg posterior. Splints can be augmented with a thumb spica or foot plate depending on the injury. Examples of casts include short-arm, long-arm, with or without thumb spica, as well as short-leg, long-leg, spicas.
Key elements of the history taking include the demographics of the patient (age, sex, and race), comorbidities, hand dominance (if there is an upper extremity injury), mechanism of injury, allergies to medication, and smoking or drinking history.
Examination begins with visualization of the injured extremity noting deformity, swelling, and or bruising. Careful skin examination is crucial to rule out wounds and the presence of open fracture. Neurovascular examination should be performed documenting motor and sensory function as well as strength of pulses (palpable, 1+, 2+, or identifiable by Doppler). Finally, careful secondary exam should be performed on all other joints and extremities testing for tenderness to palpation as well as range of motion. Distracting pain from the primary injury can often prevent a patient from realizing they have an injury elsewhere. Secondary examinations should be performed multiple times during the treatment course of the patient. As the pain from the primary injury subsides, patients may begin to appreciate additional injuries.
The following is list of conditions that require immediate orthopedic evaluation and treatment: compartment syndrome, open fractures, septic arthritis, and acute dislocations. Additionally, there are other injuries such as femoral neck fractures, that depending on the age of the patient and choice of treatment that require intervention as soon as possible. Each of these conditions will be elaborated on in the upcoming chapters.
Compartment syndrome is caused by increased pressure in a closed fascial space that initially leads to compromised perfusion followed by severe tissue damage. Nerves and muscles in the affected area can be significantly compromised in a matter of hours. Severe ischemia for 6-8 hours leads to muscle and nerve death leading to chronic debilitating dysfunction of the affected extremity. As a result, compartment syndrome is an orthopedic emergency requiring immediate evaluation and treatment. Compartment syndrome can occur after fracture, limb compression or crush, vigorous exercise, or burns.
Although, it most commonly occurs in the forearm and leg, it can occur in the foot, thigh, and arm. Compartment syndrome typically presents as a painful, swollen, tense extremity. Pain with passive range of motion of the digits and pain out of proportion are considered to be the most reliable early indicators of compartment syndrome. Clinical signs of compartment syndrome include the 5 Ps: pain, poikilothermia, pallor, paresthesias, and finally pulselessness. A change in pulses is a very late sign occurring after significant damage has already occurred. Of note, compartment syndrome can occur at intracompartmental pressures well below arterial pressure. Therefore, compartment syndrome can occur in a pink limb with normal pulses.
Compartment syndrome is a clinical diagnosis; many authors advocate that if compartment syndrome is suspected immediate fasciotomy should be carried out. In scenarios where patients are obtunded, intubated, or otherwise unable to express having pain, compartment pressure can be evaluated using a commercially available self-contained pressure monitor. If a commercial pressure monitor is not available, large bore catheter can be inserted in the compartment under sterile technique. The catheter is connected to a pressure monitor via intravenous tubing filled with sterile saline solution. Absolute pressure more than 30 mm Hg in any compartment, or a pressure within 30 mm Hg of the diastolic blood pressure in hypotensive patients are indications for surgical compartment release.
Fasciotomy should be carried out with complete release of the skin and fascia of the involved compartments. Adjacent compartments in the same limb are typically released as well. Compartment pressures are rechecked after release to ensure adequate decompression. The wounds are left open and covered with sterile dressings or a vacuum-assisted closure (VAC), and are subsequently treated with delayed primary closure or skin grafting days later.
An open fracture is a defined as an osseous disruption with a break in the overlying skin and soft tissues resulting in communication between the fracture, its hematoma, and the external environment. Any wound occurring on the same limb as a fracture must be carefully inspected to prove that it is not an open fracture. Open fractures have important soft tissue consequences: (1) contamination of the wound and fracture by the external environment, (2) crushing, stripping, and devascularization that results in soft tissue devitilization and subsequent increased infection susceptibility, (3) disruption of the soft tissue envelope may affect the type of fracture immobilization as well as adversely affect fracture healing due to the loss of osteoprogenitor cell contribution from overlying soft tissues, and finally (4) loss of function from damaged muscle, tendon, nerve, vascular, and ligamentous structures.
Open fractures are typically high energy injuries. One-third of patients with open fractures have multiple injuries. As a result, initial evaluation of the patient with an open fracture follows the ABCDEs: airway, breathing, circulation, disability, and exposure. Initial resuscitation is performed along with immediate treatment for any-potential life-threatening injuries. The head, chest, abdomen, pelvis, and spine are individually evaluated for injury. Injuries to the other extremities should be identified. Neurovascular exam for the injured limb should be carefully documented; the skin and soft tissues should be assessed as well. Wound hemorrhage should be managed with direct pressure rather than limb tourniquets or clamping which may disrupt perfusion to the rest of the limb. Exploration of the wound in the emergency department setting is not indicated if operative intervention is planned due to risk of further contamination and precipitation of additional hemorrhage. If surgical delay is anticipated, gentle irrigation with sterile normal saline may be undertaken. Only obvious foreign fragments that are easily accessible should be removed. Bone fragments should not be removed and disregarded, regardless of apparent nonviability. Sterile injection of joints can be performed to determine if there is communication with a nearby wound. The wound should be covered with a sterile normal saline soaked piece of gauze (iodine has fallen out of favor due to reports of tissue toxicity). Provisional reduction and splinting should be performed, follow by subsequent neurovascular examination to confirm no additional damage. Standard trauma survey includes radiographic evaluation of the spine, chest, abdomen, and pelvis. The injured extremity including the joint above and below, along with any other extremities suspected of injury should be evaluated with x-rays in anticipation of operative intervention.
Angiogram should be performed if vascular injury is suspected in the following scenarios: knee dislocation, cool, pale hand, or foot with poor distal capillary refill, high energy injury in an area of susceptible vessels (eg, Popliteal fossa), and documented ABI less than 0.9 in an extremity with an associated injury. Of note, evaluation of the contralateral limb may reveal underlying vascular disease as the cause of decreased ABI rather than acute injury.
Open fractures can be characterized using the Gustilo and Anderson classification: Grade I: clean skin opening is less than 1 cm, Grade II: Laceration is less than 1 cm but is less than 10 cm, soft tissue damage without significant fracture comminution or crush component; Grade IIIA: extensive soft tissue damage, Grade IIIB: extensive soft tissue injury with periosteal stripping or bone exposures requiring flap coverage, and Grade IIIC: concomitant vascular injury requiring repair.
Antibiotic treatment and tetanus prophylaxis should be addressed as soon as possible in the emergency department setting. Grade I and II fractures require treatment with a first-generation cephalosporin. Previously, grade III fractures mandated the addition of an aminoglycoside to cephalosporin; however, the most recent recommendations entail treatment with ceftriaxone. For farm injuries with gross contamination, add a penicillin in addition to ceftriaxone.
Operative intervention should be carried out for open fractures as soon as possible. Intervention less than 8 hours after injury has been reported to result in a lower incidence of infection and subsequent osteomyelitis. In the operating room, the wound should be extended proximally and distally to examine the zone of injury. Meticulous debridement of the soft tissues, including the skin, subcutaneous fat, and surrounding muscle should be carried out. Large skin flaps should be avoided as their development risks further devitilization. The fracture surfaces should be exposed and debrided. Fractures can be stabilized provisionally or definitively with external or internal fixation depending on the scenario and surgeon expertise. Pulsatile lavage irrigation should be carried out, followed by meticulous hemostasis. Fasciotomy should be considered as treatment for or prophylaxis against impending compartment syndrome. Historically, only the surgically extended portions of the wound were closed, followed by dressing the open wound with saline soaked gauze or VAC. Serial debridements should be performed every 24-48 hours until there is no evidence of remaining necrotic soft tissue and bone. Bone grafting and wound coverage using delayed primary closure, skin graft, rotational, or free muscle flaps can be performed at this time.
ORTHOPEDIC TRAUMA
There are more than 10,000 new spinal cord injuries each year. The ratio of male to female patients sustaining vertebral fractures is 4:1. For patients with spinal cord injury the overall mortality rate is 17% during the initial hospital stay. Unfortunately, delayed diagnosis happens frequently due to loss of consciousness secondary to trauma or intoxication with alcohol or drugs. As a result, suspicion for spinal cord injury should remain high in trauma patients who are unable to provide an accurate history.
The spinal cord occupies between 35% and 50% of the spinal canal depending on the vertebral level. The remainder of the canal is filled with cerebrospinal fluid, dura mater, and epidural fat. The caudal termination of the spinal cord, located dorsal to the L1 vertebral body and L1-L2 intervertebral disk, is called the conus modularis. The conus modularis gives off motor and sensory nerve rootlets, also known as the “cauda equina” or horse’s tail.
The spinal column consists of four major components that contribute to its stability: (1) the vertebral bodies, (2) the posterior elements (pedicles, laminae, spinous process, and interlocking paired facets at each level), (3) the intervertebral disk; and (4) and attached ligamentous tissues (interspinous ligaments, facet capsules, and ligamentum flavum).
The atlas is the first cervical vertebra (C1). Although it does not have a vertebral body, it has two large lateral masses which serve as weight-bearing articulations between the skull and the vertebral column. The tectorial membrane and the alar ligaments are key contributors to normal craniocervical stability. The axis is the second cervical vertebra, whose body is the largest in the cervical spine. The transverse atlantal (aka cruciform) ligament is the primary stabilizer of the atlantoaxial joint, with the alar ligaments providing secondary stability. There are five additional cervical vertebra (C3-C7).
The thoracolumbar spine consists of 12 thoracic vertebrae and 5 lumbar vertebrae. The thoracic region is naturally kyphotic (apex of bow is posterior), while the lumbar region is lordotic (apex of bow is anterior). The thoracic spine is much stiffer than the lumbar spine in flexion-extension and lateral bending, due to the additional stability provided by the rib cage as well as thinner intervertebral disks. As a result, due to its transition zone status, the thoracolumbar junction (T11-L1) is more susceptible to injury.
The spinal column can also be conceptualized as three columns with regards to its stability: (1) the anterior column (the anterior half of the vertebral body, anterior half of the intervertebral disk, and anterior longitudinal ligament), (2) the middle column (the posterior half of the vertebral body, posterior half of the intervertebral disk, and posterior longitudinal ligament), and (3) the posterior column (the facet joints, lateral masses, intraspinous ligaments, supraspinous ligaments, and spinous processes). In general, a one-column injury is relatively stable, while a three-column injury is significantly unstable, with increased risk of injury to the spinal cord.
The spinal cord roots exit the spinal canal through the intervertebral foramina. In the cervical spine, the C1 root exits above the C1 vertebral body; the C2 root exits below the C1 vertebral body. This pattern continues for the other cervical nerve roots ending with the C8 root exiting below the C7 body. In the thoracic and lumbar spine, each root exits under the pedicle with the same number. For example, the L4 nerve root exits under the L4 pedicle.
Clinical evaluation of the spine injury patient begins with the ABCDEs. All victims of trauma are suspected of having a spinal column injury until it proven otherwise. Initially, patients are placed in a c-collar and on a backboard until the patient’s spine can be assessed. A special backboard with head cutout should be used for children (6 years old or less) to prevent unintended neck flexion due to their proportionally larger head size and resulting prominent occiput.
The head-tilt-chin-lift maneuver should be avoided due to possible further disruption of the cervical spine. Airway and breathing are ensured by intubation and mechanical ventilation. Nasotracheal intubation is the safest method of airway control in the acute setting because it leads to less cervical spine motion compared with direct oral intubation.
Neurogenic shock with hypotension and bradycardia can occur in the setting of spinal cord injury. Initial resuscitation of the patient entails administration of isotonic fluids, as well as evaluating injuries to the head, chest, abdomen, pelvis, and extremities. The diastolic pressure should be kept above 70 mm Hg to maximize spinal cord blood flow. However, once the diagnosis of neurogenic shock is established, the blood pressure should be managed with vasopressors to prevent fluid overload.
If within 8 hours of injury, administer Methylprednisolone for complete or incomplete spinal cord injuries. An initial bolus of 30 mg/kg is administered over the first 15 minutes followed by 5.4 mg/kg/h over the following 24 hours (if steroids were started within 3 hours after injury) or 48 hours (if steroids were started within 3-8 hours after injury). Treatment with methylprednisolone has been shown to improve long-term motor recovery.
Sensory deficits caused by either cord or root level injuries can result in the rapid development of decubitus ulcers over insensate skin over high-pressure areas of the body (eg, the heels and ischium). As a result, timely assessment and removal of the patient from the spine board and onto an appropriate bed is critical.
Evaluating the spine includes logrolling the patient for visual inspection, palpation of the spinous processes for tenderness or diastasis, and performance of a rectal exam assessing resting tone, perianal sensation, and the bulbocavernosus reflex (squeeze of the glans penis or pull on urethral catheter results in contraction of the anal sphincter). Neurologic examination should also be performed assessing motor strength and dermatomal sensation. The motor strength testing and motor nerve roots match up as follows: shoulder abduction (C5), elbow flexion and wrist extension (C6), elbow extension and wrist flexion (C7), wrist extension and finger flexion (C8), finger abduction (T1), hip flexion (L2), knee extension L3, ankle dorsiflexion (L4), long toe extensors (L5), and ankle plantar flexors (S1). Careful evaluation and documentation of the patient’s neurologic status will allow the physician to determine the appropriate treatment plan and estimate the prognosis for functional recovery.
The cervical spine can be cleared clinically in patients if the following criteria are met: (1) no posterior midline tenderness, (2) full pain-free range of motion, (3) no focal neurologic deficit, (4) normal level of alertness, (5) no evidence of intoxication, and (6) no distracting injury. Radiographic evaluation is not required. The process of the clearing the thoracolumbar spine is similar; however, anteroposterior and lateral radiographs of the TLS spine should be routinely obtained for evaluation. If any of the above criteria are not met for clearing the cervical spine, due to its increased sensitivity compared to radiographs, CT scan with sagittal reconstructions of the cervical spine to rule-out injury has become the standard of care.
In addition to spinal trauma, other injuries should be assessed since they may influence the treatment of the patient. Suspicion of associated injuries is dependent on the mechanism and location of injury. Cervical Spine injuries can be associated with injuries to the vertebral artery. Flexion-distraction injuries (seat-belt injuries) of the thoracolumbar spine are associated with intra-abdominal injuries. Axial loading injury mechanisms that often result in burst fractures of the lumbar spine are also responsible for axial loading injury patterns in the lower lumbar spine and lower extremities. These include fractures of the pars interarticularis of the L5 vertebra, the tibial plafond, and the calcaneus.
It is important to note that any injury associated with progressive neurologic deficit warrants surgical intervention.
Neurologic injury can be described as complete (no sensation/motor caudal to the level of the spinal cord pathology) or incomplete (some neurologic function persists caudal to the level of injury). Four major patterns of incomplete spinal cord injury can occur: (1) Brown-Séquard Syndrome (hemicord injury with ipsilateral muscle paralysis, loss of proprioception, and light touch sensation, (2) Central Cord Syndrome (flaccid paralysis of the upper extremities and spastic paralysis of the lower extremities with sacral sparing, (3) Anterior Cord Syndrome (motor and pain/temperature loss controlled by the corticospinal and spinothalamic tracts with preserved light touch and proprioception controlled by the dorsal columns), (4) Posterior Cord Syndrome (rare, involves loss of deep pressure, deep pain, and proprioception with full voluntary power, pain, and temperature sensation), and (5) Conus Modularis Syndrome (T12-L1 injuries resulting in loss of voluntary bowel and bladder control with preserved lumbar root function).
Nerve root lesions can occur at any level accompanying spinal cord injury. These lesions may be partial or complete, resulting in radicular pain, sensory dysfunction, weakness, hyporeflexia, or areflexia.
Cauda Equina syndrome is caused by multilevel lumbosacral root compression within the lumbar spinal canal. Clinical presentation can include saddle anesthesia, bilateral radicular pain, numbness, weakness, hyporeflexia or areflexia, and loss of voluntary bladder or bowel function.
The motor and sensory examination outlined by the American Spinal Injury Association (ASIA) is one system to assess the impact on the patient of spinal cord injury. This grading system allows the patient to be assessed through scales of impairment and functional independence, evaluating remaining sensory and motor function. A thorough neurologic examination should be performed and documented when the patient is initially seen and at frequent intervals thereafter both to ensure that there is no further neurologic deterioration and to document the resolution of spinal shock.
Spinal shock is defined as spinal cord dysfunction due to physiologic disruption, resulting in hypotonia, areflexia, and paralysis distal to the level of injury. Resolution usually occurs within 24 hours with the return of reflex arcs caudal to the level of injury; the bulbocavernosus reflex is usually the first one to come back.
If a patient has a complete neurologic deficit after spinal shock has resolved, the chance for recovery of neurologic function below the level of injury is extremely poor. In contrast, patients with root level injuries (at or below the cauda equina) will recover from functionally complete injuries if they have not been transected and if initial compression by bone fragments, malalignment, or disk material has been relieved.
The sensory level is determined by the patient’s ability to perceive pinprick (using a disposable needle or safety pin) and light touch (using a cotton ball). Testing of a key point in each of the 28 dermatomes on the right and left sides of the body as well as evaluation of perianal sensation is necessary. The variability in sensation for each individual stimulus is graded on a 3-point scale:
0 = Absent
1 = Impaired
2 = Normal
NT = Not testable
In the cervical spine, the C3 and C4 nerve roots supply sensation to the entire upper neck and chest in a cape-like distribution from the tip of the acromion to just above the nipple line. The next adjacent sensory level is the T2 dermatome. The brachial plexus (C5-T1) supplies the upper extremities.
ASIA also recommends testing of pain and deep pressure sensation in the same dermatomes as well as evaluation of proprioception by testing the position sense of the both index fingers and both great toes.
The motor level is determined by manual testing of a key muscle in the ten paired myotomes from cephalad to caudal. The strength of each muscle is graded on a six-point scale:
0 = Complete paralysis
1 = Palpable or visible contraction
2 = Full range of motion of the joint powered by the muscle with gravity eliminated
3 = Full range of motion of the joint powered by the muscle against gravity
4 = Active movement with full range of motion against moderate resistance
5 = Normal strength
NT = Not testable
The grading system is as follows: (1) Grade A (complete impairment; no motor or sensory function is preserved below the neurologic injury level), (2) Grade B (incomplete; sensory but not motor function is preserved below the neurologic level and extends through the sacral segment S4-S5), (3) Grade C (incomplete; motor function is preserved below the neurologic level with key muscles having a muscle grade < 3), (4) Grade D (incomplete; motor function is preserved below the neurologic level of injury; most key muscles below the neurologic level have a muscle grade > 3), and (5) Grade E (normal: motor and sensory function is normal).
Plain radiographs can be used as the first imaging modality for the cervical spine, although CT scan of the cervical spine is becoming the initial test of choice due to its increased sensitivity and consistent ability to visualize the occipitocervical and cervicothoracic junctions. The standard series of radiographs includes an anteroposterior, lateral, and an open-mouth “odontoid” view. Eighty-five percent of all significant injuries to the cervical spine will be detected on the lateral view of the cervical spine. Radiographic markers of cervical spine instability include the following: compression fractures with more than 25% loss of height, angular displacement more than 11 degrees between adjacent vertebrae, translation more than 3.5 mm, and intervertebral disk space separation more than 1.7 mm. If the standard lateral view does not adequately visualize the C7-T1 junction, further studies such as a swimmer’s view, oblique views, or CT of this area are necessary. Flexion-extension views of the cervical spine can be performed if instability is still suspected in a patient with otherwise normal radiographic findings. Performance of these radiographs should be delayed in a patient with neck pain, as muscle spasm can mask instability.
All patients with significant injury and pain in the spinal area require anteroposterior and lateral x-rays of symptomatic regions of the thoracic and lumbar spine. CT can be used to evaluate canal compromise, and for preoperative planning MRI is useful for assessing the degree of neural injury and prognosis.
Patients with cervical spine injury may have impaired pulmonary function secondary to intercostal nerve paralysis. Mobilization of secretions by chest physical therapy and frequent suctioning are critical for preventing atelectasis and pulmonary infections. All patients with sensory deficits and paralysis are at high risk of developing pressure ulcers. Padding and suspension of high-risk pressure points (heels), frequent turning, and vigilant nursing care are necessary.
Patients with thoracolumbar spine fractures with or without spinal cord injury may have paralytic ileus secondary to sympathetic chain dysfunction. Oral intake should be limited to clear fluids initially, and gastric suction may be necessary if the degree or duration of ileus is significant.
The stress caused by the injury itself—in combination with systemic corticosteroid therapy—can increase the incidence of gastrointestinal ulceration and bleeding. High-dose corticosteroids can also contribute to the development of pancreatitis and infections.
Venous thromboembolic disease remains a significant problem in the management of patients with spinal injury. Pulmonary embolism is the most common cause of preventable death in hospitalized patients. Heparin can be used for DVT prophylaxis, until the patient’s mobility improves.
Occipital condyle fractures can be classified as follows: (1) type I (impaction of condyle, stable), (2) type II (shear injury associated with basilar or skull fractures; potentially unstable), (3) type III (condylar avulsion fracture, unstable). Treatment involves rigid cervical collar immobilization for 8 weeks for stable injuries and halo immobilization or surgical stabilization for unstable injuries.
Also known as craniovertebral dislocation, this is almost always fatal. Postmortem studies show this injury to be the leading cause of death in motor vehicle accidents. Rare survivors usually have severe neurologic deficits. Immediate treatment includes halo vest application with strict avoidance of traction. Long-term stabilization is done surgically with occipitocervical fusion.
Atlas fractures are rarely associated with neurologic injury. Instability due to transverse alar ligament insufficiency should be suspected with identification of bony avulsion or widening of the lateral masses on radiographic evaluation. These injuries can be classified as follows: (1) isolated bony apophysis fracture, (2) isolated posterior arch fracture, (3) isolated anterior arch fracture, (4) comminuted lateral mass fracture, and (5) burst fracture (fractures of the anterior and posterior ring). Stable fractures (posterior arch or nondisplaced fractures) may be treated with rigid cervical orthosis; unstable fractures require prolonged halo immobilization. Chronic instability or pain may be treated with C1-C2 fusion.
This injury is rare, but usually fatal when it occurs. This injury is diagnosed by visualizing the avulsed lateral mass fragment, an atlantodens interval (ADI) more than 3 mm in adults, atlantoaxial offset more than 6.9 mm on an odontoid radiograph, or direct visualization of the rupture on MRI. Survivors are treated with halo or C1-C2 fusion.
There is a significant association with other cervical spine fractures and a 5%-10% incidence of neurologic injury. The vascular supply to the odontoid arrives through the apex and the base of this bone with a watershed area in the neck. Odontoid fractures are classified as follows: (1) type I (oblique avulsion fracture of the apex), (2) type II (fracture at the junction of the body and the neck; high nonunion rate, which can lead to myelopathy), (3) type IIa (highly unstable comminuted injury extending from the waist of the odontoid to the vertebral body), and (4) type III (fracture extending in the cancellous body of C2 and possibly involving the lateral facets). Treatment entails cervical orthosis for type I fractures and halo immobilization for type III fractures. Treatment of type II fractures is controversial due to the high incidence of nonunion related to poor vascularity; halo or surgical intervention is advocated depending on patient factors.
These injuries are usually diagnosed via CT scan. Treatment varies from collar immobilization to late fusion for chronic pain.
Also known as the Hangman’s fracture, this injury may be associated with cranial nerve, vertebral artery or craniofacial injuries. Type I injuries are nondisplaced fractures without angulation, less than 3 mm of translation, and the C2-C3 disk is intact. Type II injuries are displaced fractures of the pars. Type IIa is a displaced pars fracture with disruption of the C2-C3 disk. Type III is a dislocation of the C2-C3 facet joints in addition to the pars fracture. Type I injuries are treated with rigid cervical orthosis, type II injuries are treated with halo immobilization, type III injuries are usually treated initially with halo immobilization followed by surgical stabilization.
Injuries for the remaining vertebrae from C3-C7 include teardrop fractures of the anterior portion of the vertebral body due to compression flexion, vertical compression (burst fractures), anterior dislocations due to distractive flexion, vertebral arch and lamina fractures due to compressive extension, distractive extension injuries resulting in posterior dislocations, and lateral flexion injuries resulting in translational dislocations.
“Clay shoveler’s fracture” is an avulsion fracture of the spinous processes of the lower cervical and upper thoracic vertebra.
“Sentinel fracture” is a fracture through the lamina on either side of the spinous process.
Treatment for each of these fractures includes the use of cervical orthoses, halo immobilization, traction, and surgery. Soft cervical orthosis does not provide any significant immobilization. It is used as needed for the patient’s comfort. Rigid cervical orthoses do not provide complete immobilization; this treatment mainly limits range of motion in the flexion-extension plane. Cervicothoracic orthoses are effective in flexion-extension and rotational control, but do not limit lateral bending very effectively. Halo immobilization offers rigid immobilization in all planes as does surgical treatment. Traction can be used to reduce unilateral or bilateral facet dislocations with neurologic deficits or to stabilize and indirectly compress the canal in patients with neural deficits from burst-type fractures. Traction is contraindicated in type IIa spondolisthesis injuries of C2 and distractive cervical spine injuries.
Choice of treatment depends on the type of injury and individual patient characteristics. In general, stable fractures can be managed with bracing, while unstable fractures require more rigid stabilization via halo application or surgical treatment.
The halo apparatus includes the metal ring and halo vest. The halo ring should be applied approximately 1 cm above the ears. Anterior pin sites should be placed above the supraorbital ridge, anterior to the temporalis muscle over the lateral 2/3 of the eyebrow to avoid the supraorbital nerve. Posterior sites are variable and are placed to maintain the horizontal orientation of the halo. Pin pressure should be 6-8 lbs in the adult. Pin care is essential. The halo vest relies on a tight fit that should be carefully maintained.
Anteroposterior and lateral radiographs of the Thoracolumbosacral spine are the standard initial evaluation. Abnormal interpedicular distance, height loss, and canal compromise should all be noted. Minor spine injuries include articular process fractures, transverse process fractures, spinous process fractures, and pars interarticularis fractures. Generally, these injures can simply be observed. Six significant injury patterns requiring treatment are described: (1) wedge compression fracture, (2) stable burst fracture, (3) unstable burst fracture, (4) chance fracture, (5) Flexion-distraction injury, and (6) translational injuries.
Based off of the three column theory of instability, compression fractures are fractures that only affect the anterior column. Compression fractures can be anterior or lateral. In general these fractures are stable injuries and are rarely associated with neurologic injury. Fractures are considered unstable if there is more than 50% loss of vertebral body height, angulation more than 20-30 degrees, or multiple adjacent compression fractures. Four subtypes are described based off of endplate involvement: type A (fracture of both endplates), type B (fracture of superior endplate), type C (fracture of inferior endplate), and type D (both endplates are intact). Stable fractures are treated with Jewett brace or thoracolumbar spinal orthosis (TLSO). Unstable fractures can be treated with hyperextension casting or with surgery.
Burst fractures are fractures that involve the anterior and middle columns of the spinal cord. Radiographs may show loss of posterior vertebral body height and splaying of the pedicles on the anteroposterior view. It is important to note that no direct relationship exists between the amount of canal compromise and the degree of neurologic injury. Treatment can entail tho TLSO bracing or hyperextension in casting for stable fracture patterns without neurologic compromise. If the TLSO fails to restore appropriate alignment on radiographs, surgery should be considered. Early surgical intervention restoring sagittal and coronal alignment should also be considered for fractures with loss of vertebral height more than 50%, angulation more than 20-30 degrees, scoliosis more than 10 degrees, and concomitant neurologic deficit. Surgical treatment options include decompression via a posterior or anterior approach with or without instrumentation.
Also known as Chance fractures, involve all three columns of the spinal cord. These fractures are also known as “seat-belt type injuries” due to the most common mechanism by which they occur and often are associated with abdominal injuries. Radiographically, one may appreciate increased interspinous distance on the AP and lateral views. Four types of Chance fractures are recognized: (1) type A (one-level bony injury), (2) type B (one-level ligamentous injury), (3) type C (two-level injury through the bony middle column, (4) type D (two-level through the ligamentous middle column). Treatment for type A fractures may entail TLSO; however, one should consider surgical stabilization for the other three fractures given their innate lack of stability.
Fracture-dislocations involve injury to all three columns with translational deformity. These injuries are often associated with neurologic injury and require surgical stabilization due to their unstable nature. There are three types of fracture-dislocations: (1) Flexion-rotation, (2) Shear, and (3) Flexion-distraction. Patients without neurologic injury do not require emergent surgery; however, patients whose fractures are stabilized within 72 hours of injury have a lower incidence of complications such as pneumonia and undergo a shorter hospital stay when compared to patients whose fractures are stabilized outside this time-frame.
Generally, fractures associated with low-velocity gunshot wounds are usually stable when a handgun is the weapon. These injuries are typically associated with a low infection rate and can be prophylactically treated with broad-spectrum antibiotics for 48 hours.
Any present neural injury, is usually secondary to “blast effect,” in which the energy of the bullet is absorbed and transferred to the soft tissues. As a result, decompression is usually not indicated. An exception to this rule is if the bullet fragment is found in the spinal canal between levels T12 and L5. Steroids after gunshot wounds to the spine are not recommended.
If there is a neurologic deficit, surgical decompression is indicated. This can be done either through an anterior approach with bone graft and internal fixation, a posterior costotransversectomy approach, or a combined anterior and posterior approach. The operative plan is individualized to the particular patient. Patients with incomplete neurologic deficits and unstable fractures or fracture-dislocations have the same stability requirements as patients without neurologic deficits. They are best managed with open reduction, instrumentation, and spinal fusion. Neural canal compromise should be managed as in the preceding paragraph.
No operative procedure has been devised that will achieve recovery in cases of complete neurologic deficit that has persisted beyond the stage of spinal shock. However, surgical stabilization is often necessary (1) because spinal instability may interfere with early mobilization and rehabilitation training and (2) because it may result in loss of function at a higher level by causing mechanical injury on the root or cord segment just above the level of injury.
Pelvic fractures are among the most serious injuries and account for 3% of all fractures. The mechanism is often high energy in nature; 60% result from vehicular trauma (eg, automobile, motorcycle, bicycle), 30% from falls, and 10% from crush injuries, athletic injuries, or penetrating trauma. Pelvic fractures are the third most commonly seen injury in fatalities due to motor vehicle accidents.
Life-threatening hemorrhage, deformity, neurologic injury, and genitourinary injury are all potential complications that must be identified and treated early in the setting of a pelvic fracture. Pelvic fractures pose a formidable clinical challenge. Hemodynamically unstable patients who present to the emergency department with pelvic fracture have a mortality rate of 40%-50%.
An understanding of pelvic anatomy is essential for identifying fracture patterns and complications. The pelvis is made up of three bones: two innominate bones joined anteriorly at the symphysis and posteriorly at the paired sacroiliac joints. The innominate bones are further subdivided into the ilium, ischium, and pubis.
The acetabulum is the portion of the pelvic bone that articulates with the femoral head to form the hip joint. It results from closure of the triradiate cartilage and is covered with hyaline cartilage. The innominate bone support of the acetabulum can be thought of as an inverted Y formed by two columns. The anterior column (iliopubic component) extends from the iliac crest to the pubic symphysis including the anterior wall of the acetabulum. The posterior column (ilioischeal component) extends from the superior gluteal notch to the ischial tuberosity including the posterior wall. The acetabular dome is the superior weight-bearing portion of the acetabulum at the junction of the anterior and posterior columns, including contributions from both.
The stability of the pelvis is dependent on its ligamentous attachments. A thick fibrocartilaginous disk joins the anterior aspects of the innominate bones to form the pubic symphysis. This joint acts as a supporting strut for the pelvis because the stability of the ring depends mostly upon the sacroiliac joints.
The posterior ligamentous structures supporting the sacroiliac joints can be divided into anterior and posterior complexes. The anterior sacroiliac joint ligaments are broad and flat and connect the iliac wing and the sacral ala. These ligaments primarily resist external rotation and torsional forces. The sacro-iliac ligaments provide most of the stability. Composed of the interosseous sacroiliac ligaments within the joint and the posterior sacroiliac ligaments spanning the sacrum between the posterior iliac spines, the posterior complex is considered to be the strongest ligament in the human body. The posterior sacroiliac complex resists shear forces between the sacrum and the ilium, clinically preventing displacement of the ilium onto the sacrum.
The pelvic floor contains two additional strong ligaments, the sacrospinous and the sacrotuberous ligaments. The sacrospinous ligament maintains rotational control while the sacrotuberous ligament is especially important in maintaining vertical stability of the pelvis. Additional stability is conferred by ligamentous attachments between the spine and the pelvis. The iliolumbar ligaments originate from L4 and L5 transverse processes and insert on to the posterior iliac crest. The lumbosacral ligaments originate from the transverse process of L5 and insert to the sacrum ala.
Pelvic stability can be defined as the ability of the pelvic ring to withstand physiologic forces without abnormal deformation. Pathologically, the pelvic ring fails under one or more of three basic modes. External rotation strains the pubic symphysis and the sacrotuberous, sacrospinous, and anterior sacroiliac joint ligaments. After roughly 2.5 cm of diastasis, the pelvic floor ligaments and the anterior sacroiliac ligaments begin to fail, giving rise to gross rotatory instability. Because the posterior ligament complex is largely intact, superior or posterior displacement of the involved hemipelvis does not occur. Combined external and shear forces are necessary to completely disrupt pelvic stability. Conversely, internal rotation places the pubic rami under compression and the posterior ligament complexes under tension. The rami often fail in their midportions with transverse fractures and sacral alar impaction. The pelvic floor ligaments remain intact, and gross posterior stability is maintained. Therefore, fractures involving torsional forces on the pelvis often have partial instability in the rotatory plane only, with maintenance of stability to other displacement.
Complete instability, however, occurs with disruption of both the anterior and the posterior ligamentous restraints. These injuries often present with widely displaced sacroiliac joints and multiaxial instability of the involved hemipelvis. Such fractures have components of superior and posterior displacement relative to the sacrum in addition to rotational displacement in the sagittal and horizontal planes.
Physical examination includes palpation of the pelvic bony landmarks, compression maneuvers to assess stability, rectovaginal examination looking for bony spikes protruding through the mucosa representing an open fracture, and looking for blood at the urethral meatus, or a high-riding prostate on rectal exam which may indicate genitourinary injury. If bladder or urethral injury is suspected, retrograde urethrogram should be considered. The mortality rate of open pelvic fractures is as high as 50%—compared with 8%-15% for closed fractures. A secondary musculoskeletal survey examining each of the other four limbs including distal vascular status and a thorough neurologic examination should be performed as well.
The anteroposterior radiograph required in all patients with blunt trauma rapidly identifies the major pelvic injury. The AP pelvis radiograph can be looked at in a systematic way: the pubic rami, pubic symphysis (looking for widening >2.5 cm), the iliopectineal lines (represents limit of the anterior column of the acetabulum) ilioischial lines (represents limit of the posterior column of the acetabulum), the anterior lip of the acetabulum, the posterior lip of the acetabulum, the radiographic roof of the acetabulum, the pelvic wings, the sacro-iliac joints, femoral head position (rule-out concomitant hip dislocation), associated fracture of the femoral head or femoral neck, and finally the lumbar spine. Disruption of the iliopectineal line, ilioischial line, the anterior lip, posterior lip, or the radiographic roof may be indicative of acetabular fracture. Suspected acetabular fractures should be further evaluated with Judet’s views (iliac oblique and obturator oblique). The iliac oblique (45-degree external rotation view) view better delineates the anterior column and posterior wall of the acetabulum, while the obturator oblique (45-degree internal rotation view) characterizes the posterior column and anterior wall of the acetabulum in greater detail. Inlet and outlet radiographs are often required to supplement the anteroposterior film. The inlet view (patient supine, the tube directed 60 degrees caudal) can be used to evaluate for any anterior-posterior instability, while the outlet view (patient supine, tube directed 45 degrees cephalad) will best show any vertical displacement. CT scan is recommended for any suspected pelvis fracture; this modality is especially good for evaluation of the acetabulum and posterior pelvis, including the sacrum and sacro-iliac joints.
Immediate care of the polytrauma patient with a pelvic fracture must address associated retroperitoneal hemorrhage, pelvic ring instability, and injuries to the genitourinary system and rectum as well as fractures open to the peritoneum. Cessation of blood loss, minimization of septic sequelae, and stabilization of the fracture, allowing early and safe patient mobilization, are the immediate treatment goals. Hemorrhage is the leading cause of death in patients with pelvic fracture, accounting for 60% of the deaths. Most of the blood loss is from the fracture site or injured retroperitoneal veins; only 20% of the deaths are associated with major arterial injury. An average blood replacement of 5.9 units has been reported.
General resuscitative principles are applied to stabilize the patient and provide adequate tissue perfusion. Once other sites of hemorrhage have been ruled out, active bleeding from a pelvic fracture may be controlled by wrapping a pelvic binder or sheet circumferentially around the pelvis. The sheet should enclose the bilateral anterior superior iliac spines and greater trochanters, and can be fixed in placed by clipping the two ends with a hemostat. Wrapping the pelvis in this way stabilizes major fracture fragments and closes down the volume of the pelvis, dramatically reducing active blood loss. If this fails to control hemorrhage, angiography or arterial embolization is indicated. Definitive internal fixation is usually required after hemorrhage has been controlled and the patient has been stabilized.
Fracture-dislocations of the pelvis should be treated with immediate closed reduction of the hip. Stability should be assessed by ranging the hip through a full arc of motion. Unstable hips should be rereduced and placed in skeletal traction. An Irreducible hip or new-onset sciatic nerve palsy after closed hip reduction requires immediate operative treatment.
Fractures of the pelvis may be classified according to the Young and Burgess system based off of mechanism of injury. AP compression (APC) injuries result from anteriorly applied force. APC-I characterizes less than 2.5 cm of symphyseal diastasis; vertical fractures of one or both pubic rami occur, however, the sacroiliac ligaments are intact imparting rotational and vertical stability. In an APC-II injury disruption of the anterior sacro-iliac ligaments results in greater than 2.5 cm of symphyseal diastasis that is rotationally unstable, but vertically stable due to intact posterior sacroiliac ligaments. APC-III injury occurs with complete disruption of the symphysis, sacrotuberous, sacrospinous, anterior, and posterior sacroiliac ligaments resulting in a pelvis that is rotationally and vertically unstable. Lateral compression (LC) injury results from a laterally applied force to the pelvis that leads to shortening of the anterior sacroiliac, sacrospinous, and sacrotuberous ligaments with resulting transverse or oblique fractures of the pubic rami. LC-I injury describes transverse fractures of the pubic rami with sacral compression on the side of injury without rotational or vertical instability. LC-II injuries describe the addition of a crescent iliac wing fracture on the side of impact with variable disruption of the posterior ligamentous structures resulting in rotational instability. LC-III describes an LC-I or LC-II injury on the side of impact with continuation of the force producing an external rotation or open book (APC) type injury on the contralateral side. Vertical shear (VS) injury due vertical or longitudinal forces caused by falls onto an extended lower extremity, impacts from above, or motor vehicle accidents with a lower extremity impacted against the dashboard or floorboard, typically results in complete ligamentous disruption, rotational and vertical instability, with a high incidence of neurovascular injury, and hemorrhage. Combined mechanical (CM) describes a combination of injuries often due to crush mechanism.
Pelvic fractures may also be classified according to instability using the Tile classification: type A (rotationally and vertically stable), type B (rotationally unstable and vertically stable, or type C (rotationally and vertically unstable). Common radiographic signs of pelvic instability include (1) displacement of the posterior sacroiliac complex more than 5 mm in any plane; (2) the presence of a posterior fracture gap rather than an impaction; and (3) the presence of an avulsion fracture of the transverse process of the fifth lumbar vertebra or the sacro-ischial end of the sacrospinous ligaments.
Type A fractures involve the pelvic ring in only one location and are considered stable. Type A1 fractures are avulsion fractures that usually occur at muscle origins such as the anterosuperior iliac spine, anteroinferior iliac spine, and ischial apophysis. These fractures most often occur in adolescents, and conservative treatment is usually sufficient. Rarely, symptomatic nonunions develop and can be best treated surgically.
Type A2 fractures are isolated fractures of the iliac wing without involvement of the hip or sacroiliac joints and are usually a result of direct trauma. Even with significant displacement, bony healing is expected and treatment is therefore symptomatic. Healing may be accompanied by ossification of the hematoma with exuberant new bone formation. Finally, type A3 fractures are isolated fractures of the obturator foramen and usually involve minimal displacement of the pubic or ischial rami. The posterior sacroiliac complex is intact, and the pelvis remains stable. Treatment is symptomatic, with early ambulation and weight bearing as tolerated.
Type B fractures involve breaks in the pelvic ring in two or more sites. This creates a pelvic fracture that is rotationally unstable but vertically stable. Type B1 fractures are open book fractures that occur from anteroposterior compression. Unless the anterior separation of the pubic symphysis is severe (> 6 cm), the posterior sacroiliac complex is usually intact and the pelvis is relatively stable to vertical forces. Significant associated injuries to the perineal and urogenital structures are often present and should always be looked for. For minimally displaced symphysial injuries (< 2.5 cm), only symptomatic treatment is needed. However, if conservative treatment is pursued, serial radiographs are required after mobilization is begun to monitor for subsequent increased displacement that may require surgery. For more displaced fracture-dislocations, reduction is done by LC using the intact posterior sacroiliac complex as the hinge on which the “book is closed.” Reduction can be maintained with the use of an external fixator; however, internal fixation with a symphyseal plate is currently favored. “Closing the book” decreases the space available for hemorrhage, increases patient comfort.
Type B2 and B3 fractures involve a lateral force applied to the pelvis, causing inward displacement of the hemipelvis through the sacroiliac complex and ipsilateral (B2) or, more often, contralateral (B3) pubic rami fractures. The degree of involvement of the posterior sacroiliac ligament complex will determine the degree of instability. The hemipelvis is infolded, with overlapping of the pubic symphysis. Reduction can be accomplished with external fixation, with internal fixation, or with both. External fixation facilitates nursing care but is not strong enough for ambulation. Definitive care usually is accomplished with internal fixation of both the anterior and posterior aspects of the pelvic ring. Major hemorrhage is associated with these fracture types.
Type C fractures are both rotationally and vertically unstable. They often result from a VS injury such as a fall from a height. Anteriorly, the pubic symphysis or pubic rami may be disrupted. Posteriorly, the sacroiliac joint may be disrupted and dislocated, or there may be a fracture through the sacrum or adjacent iliac wing. The hemipelvis is completely unstable, and there may be associated massive hemorrhage and injury to the lumbosacral pelvis. External fixation is insufficient to maintain reduction, but it may help to control hemorrhage and ease nursing care in the acute stage. Internal fixation is usually required as definitive treatment.
Fractures of the sacrum can be described using the Denis classification according to the location of the fracture in relation to the sacral foramen: Denis I: lateral to the foramen, Denis II: through the foramen, and Denis III: medial to the foramen. The incidence of neurologic injury increases with higher classification.
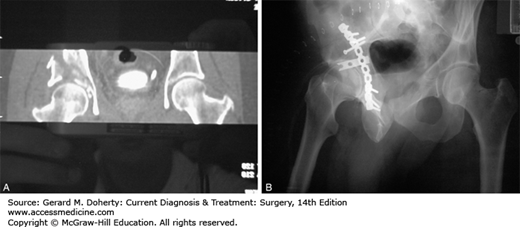
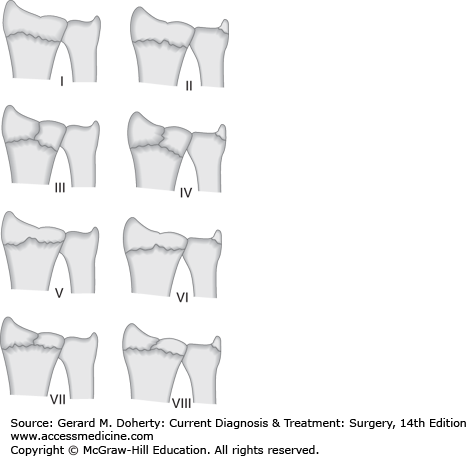
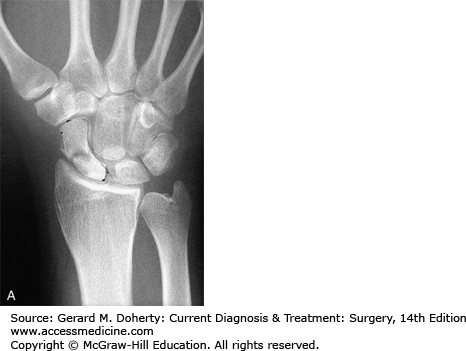
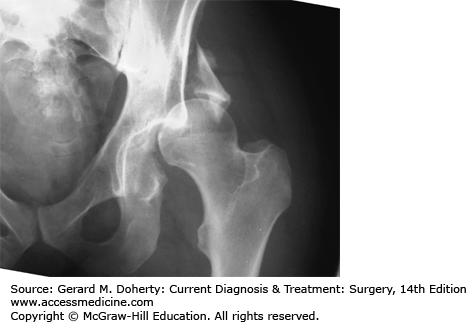
Fractures of the acetabulum (Figure 40–1) occur through direct trauma on the trochanteric region or indirect axial loading through the lower limb. The position of the limb at the time of impact (rotation, flexion, abduction, or adduction) will determine the pattern of injury. Comminution is common.
Figure 40–1.
Forty-year-old man who fell from a height, sustaining a posterior hip dislocation and an acetabular fracture of the weight-bearing dome. A. Coronal CT reconstructions showing large fragment of the superior dome of the right acetabulum. B. Oblique radiograph demonstrating concentric reduction of the hip and restoration of the articular surface after open reduction and internal fixation.
Letournel has classified acetabular fractures into ten different types: five simple patterns (one fracture line)-posterior wall, posterior column, anterior wall, anterior column, transverse and five complex patterns (the association of two or more simple patterns)-T-shaped, posterior column and posterior wall, transverse and posterior wall, anterior column/posterior hemi-transverse, and both column. This is the most widely used classification system as it allows the surgeon to choose the most appropriate surgical approach.
The goal of treatment is to achieve a spherical congruency between the femoral head and the weight-bearing acetabular dome and to maintain it until the bones are healed. As with other pelvic fractures, acetabular fractures are frequently associated with abdominal, urogenital, and neurologic injuries, which should be systematically sought and treated. Significant bleeding is often present and should be stopped as soon as possible.
The stabilized patient with protrusion (the femoral head is impacted through the fracture of the acetabulum into the pelvis) or unstable fracture-dislocation should be put in longitudinal skeletal traction through a distal femoral or proximal tibial pin pulling axially in neutral position. Postreduction x-rays are obtained. Operative indications for acetabular fractures include displacement (> 2-3 mm), large posterior wall fragments, interposed intra-articular loose fragment, femoral head fractures, unstable reductions, and an irreducible fracture dislocation by closed methods. The choice of approach is of primary importance, and more than one approach will sometimes prove necessary. Acetabular surgery uses extensile approaches and sophisticated reduction and fixation techniques and is best performed by pelvic surgeons.
Complications inherent to the injury include posttraumatic degenerative joint disease, heterotopic ossification, femoral head osteonecrosis, deep vein thrombosis, and other complications related to conservative treatment. Surgery is performed to prevent or delay osteoarthritis (OA), but it increases the possibility of complications such as infection, iatrogenic neurovascular injury, and increased heterotopic ossification. When the reduction is stable and fixation is solid, the patient can be mobilized after a few days with non–weight-bearing ambulation, and weight bearing may begin as early as 6 weeks. Prophylactic anticoagulation and aggressive pulmonary toilet are key elements of postoperative care.
Clavicle fractures are relatively common accounting for between 2% and 12% of all fractures. Clavicle fractures are characterized by location: medial, lateral, and middle third of the clavicle which is the most common type (80%). The most common mechanism of injury is fall on to the ipsilateral shoulder (87%); direct impact (7%) and falls onto an outstretched hand cause the rest. The clavicle is an S-shaped bone that serves as a strut bracing the shoulder in relation to the trunk, allowing the shoulder to function at maximum strength. The clavicle is stabilized by the acromioclavicular and coracoclavicular ligaments. The acromioclavicular ligaments prevent horizontal displacement while the coracoclavicular ligaments provide vertical stability. The middle one-third of the clavicle protects the brachial plexus, superior lung, subclavian and axillary arteries. As a result, it is critical to document a thorough neurovascular examination, and rule-out concomitant injuries such as brachial plexus palsy, vascular injury, and pneumothorax. It is also important to note the appearance of the skin as tenting may be an indication for surgery. Clavicle fractures are most often incidentally seen on the AP radiograph of the chest. Proximal third clavicle fractures can be further evaluated with computed tomography to differentiate between sternoclavicular dislocations from epiphyseal injury.
Clavicle fractures are classified into three groups: Group I: middle third fracture, Group II: distal third, Group III: proximal third. Group II fractures are subclassified into three types according to the location of the coracoclavicular ligaments relative to the fracture. Type I fractures are interligamentous, either in between the conoid and trapezoid ligaments or between the coracoclavicular and acromioclavicular ligaments, with the ligaments still intact. Because ligaments are attached to both the proximal and distal fracture segments, the fracture is typically nondisplaced or minimally displaced. Group II, type II fractures occur medial to the coracoclavicular ligaments or in between the conoid and trapezoid ligaments with the conoid ligament torn, such that the proximal fracture segment is predisposed to significant displacement. Group II, type III is a distal-third fracture of the articular surface of the AC joint without ligamentous injury.
Clavicle fractures are typically treated conservatively with a sling or figure of eight brace for 4-6 weeks until healing is appreciated radiographically and clinically (area no longer tender with palpation). Sling is typically preferred due to lower incidence of skin problems and increased patient comfort. Some degree of shortening and deformity is expected with closed treatment. However, shoulder dysfunction is rare and there is no scar. Strict indications for surgery include open clavicle fractures, associated neurovascular injury, and skin tenting concerning for impending open fracture. Some authors advocate fixing significantly displaced (> 1-2 cm) middle-third clavicle fractures and Group II, type II distal clavicle fractures, due to predisposition to nonunion which may result in cosmetic deformity and shoulder dysfunction.
The AC joint is diarthroidal with fibrocartilage-covered articular surfaces between the medial acromion and the lateral end of the clavicle. The AC ligaments blend with fibers from the deltoid and trapezius to provide strength to the joint. As described previously, the AC ligaments provide horizontal stability while the coracoclavicular ligaments provide vertical stability. The mechanism for dislocation of the acromioclavicular joint is most commonly direct impact caused by a fall on the tip of the shoulder. Thorough neurovascular examination along with standard trauma series of the shoulder (AP, scapular-Y, and axillary views) completes the standard workup. Stress radiographs in which 10-15 lb weights are strapped to the wrists and an AP radiograph is taken of both shoulders comparing coracoclavicular distances, to differentiate between partial grade I to II injuries and grade III AC separations.
Type I is a strain of the acromioclavicular ligament. Type II injury involves rupture of the acromioclavicular ligament and strain of the coracoclavicular ligament complex, with slight superior displacement of the superior clavicle type III injury involves rupture of both the acromioclavicular and the coracoclavicular ligaments, which causes marked superior migration of the lateral end of the clavicle types IV, V, and VI injuries involve detachment of the deltoid and trapezius from the distal clavicle in addition to disruption of the AC and CC ligaments with marked posterior, superior, and inferior displacement of the clavicle, respectively.
Type I, II, and III AC joint injuries are typically managed nonoperatively with a sling for approximately 4 weeks followed by gradual return to full activity. Most patients do not have significant dysfunction or any need to modify their activities. Surgical reconstruction may be indicated for types IV, V, and VI AC joint injuries. Type III injuries in young athletes or laborers who perform a lot of overhead work may be treated surgically.
Dislocation of the sternoclavicular joint is rare. The mechanism of injury is usually a motor vehicle accident or sporting injury. Physical examination and anteroposterior and anteroposterior-cephalic tilt x-rays may demonstrate asymmetry. However, computed tomography is diagnostic test of choice as it can distinguish fractures of the medial clavicle from SC dislocation and can show minor subluxation. Anterior dislocation is more common, but posterior dislocation can cause injury to the esophagus, trachea, great vessels, subclavian artery, carotid artery, and pneumothorax. Dislocations of the sternoclavicular joint in children are often associated with physical fractures.
Most injuries to the sternoclavicular joint may be treated with a ice for the first 24 hours and immobilization with a sling, sling and swathe, or figure-of-eight bandage. Posterior dislocations may require emergent reduction if there is associated vascular compression or injury to the trachea, esophagus, or lungs. Closed reduction of posterior dislocations has been described using shoulder retraction and a towel clip. Rarely, open reduction may be necessary.
Scapular fractures are classified by anatomic location: scapula body, neck, spine, acromion, coracoid, or glenoid. Scapular body fractures are often associated with other injuries such as subclavian vessel injury, aortic rupture, pneumothorax, rib fractures, brachial plexus injuries, and other soft tissue injuries associated with high-energy trauma. Fractures of the acromion and coracoid are rare. Glenoid fractures must be carefully evaluated for articular surface step-off and associated glenohumeral instability. These fractures may be caused by a blow on the shoulder or by a fall on the outstretched arm. Diagnosis with anteroposterior x-ray in the plane of the scapula and axillary x-ray may be supplemented by an axial view of the scapular body and transscapular {ss}Y{end}-view. CT scan may also be helpful if surgery is being considered.
Most scapular fractures are treated nonoperatively in a sling for 4-6 weeks. Associated injuries may need to be treated emergently and should not be overlooked. Surgical indications are controversial, but may include displaced intra-articular fractures involving more than 25% of the articular surface, scapular neck fractures more than 40 degree angulation or 1 cm of medial translation, scapula neck fractures with an associated displaced clavicle fracture, acromion fractures that cause subacromial impingement, and coracoid fractures that cause functional AC separation.
The shoulder (glenohumeral) joint is the most commonly dislocated joint in the body due to its freedom of motion and mobility in multiple planes. Diagnosis and management of this is presented in detail in the Sports Medicine section of this chapter.
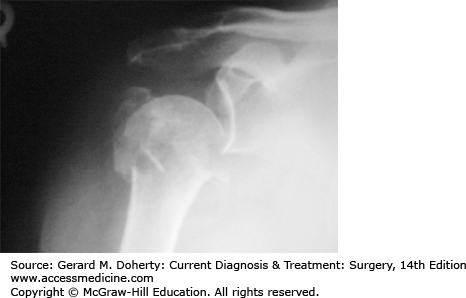
Fractures of the proximal humerus occur most commonly in elderly individuals with osteoporosis, after a fall initial assessment should seek to determine the cause of any related fall as well as the fracture pattern. Prodromal symptoms related to a syncopal episode, myocardial infarction, stroke, transient ischemic attack, or seizure are possible etiologies that should be investigated. Associated injuries include neurovascular injuries, dislocation, and rotator cuff tears. Axillary nerve function should be assessed testing sensation over lateral aspect of shoulder, overlying deltoid (motor testing is usually not possible, due to pain).
Diagnosis is established by standard shoulder trauma series (AP, lateral scapular Y, and axillary views). The axillary view is the best view for evaluating glenoid articular fractures and dislocations. If axillary view cannot be obtained due to pain, a Velpeau axillary view where the patient is left in a sling leaned obliquely backward 45 degrees over the cassette with the beam directed caudally is another option. Computed tomography can be used to further evaluate articular involvement, fracture displacement, impression fractures, and glenoid rim fractures.
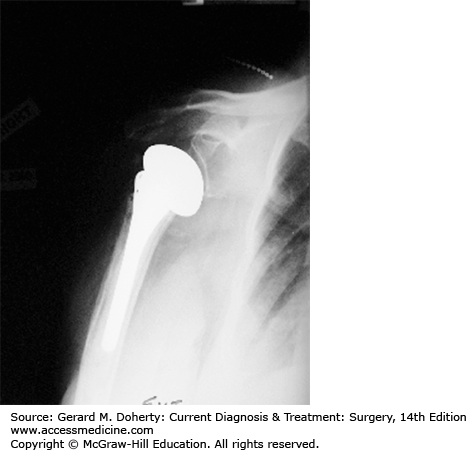
Proximal humerus fractures can be classified according to the system developed by NEER. There are four major parts of the proximal humerus: humeral head, humeral shaft, greater, and lesser tuberosities. A part is defined as displaced if there is more than 1 cm of fracture displacement, or more than 45 degrees of angulation. Most proximal humerus fractures are minimally displaced (< 1 cm and < 45 degrees of angulation) and can be treated in a sling with early gentle range of motion exercises. Displaced fractures usually require surgery. Surgical options include closed reduction and percutaneous fixation, open reduction and internal fixation, and prosthetic arthroplasty (Figures 40–2 and 40–3). Other indications for surgery include superior displacement of the greater tuberosity fragment of 5 mm or more which can lead to subacromial impingement, lesser tuberosity fractures that block internal rotation. Patients often lose some range of motion, but excellent pain relief and function can be attained. Long-term complications include shoulder stiffness and avascular necrosis of the humeral head (due to disruption of the arcuate branch off of the anterior circumflex humeral artery).
Most fractures of the shaft of the humerus result from direct trauma; indirect mechanism from fall on an outstretched arm is also a possibility. A careful neurovascular exam is required (radial nerve injury is most common). AP and lateral radiographs of the humerus, as well as shoulder and elbow series are mandatory to rule out the possibility of fracture or dislocation involving adjacent joints. Humerus fractures can be described descriptively: open versus closed, location (proximal, middle, and distal third), nondisplaced versus displaced, transverse, oblique, spiral, segmental or comminuted fracture, intrinsic condition of bone (osteopenic or not), and if there is any articular extension.
Most midshaft humeral fractures can be treated nonoperatively in a cast, splint, or brace. Alignment should be verified using AP and lateral x-rays with the patient standing. Twenty degrees of anterior angulation, 30 degrees of varus angulation, and up to 3 cm of bayonet apposition are acceptable for continued closed treatment. Other surgical indications include open fractures, concomitant vascular injury, pathologic fracture, “floating elbow” (concomitant fracture of the forearm bones), segmental fracture, intra-articular extension, and bilateral humeral fractures. Radial nerve injury most commonly occurs with middle third fractures. Most radial nerve injuries are the result of stretching or contusion; function usually returns in 3-4 months. Delayed surgical exploration is warranted if there is no evidence of recovery on EMG or nerve conduction velocity studies at this time.
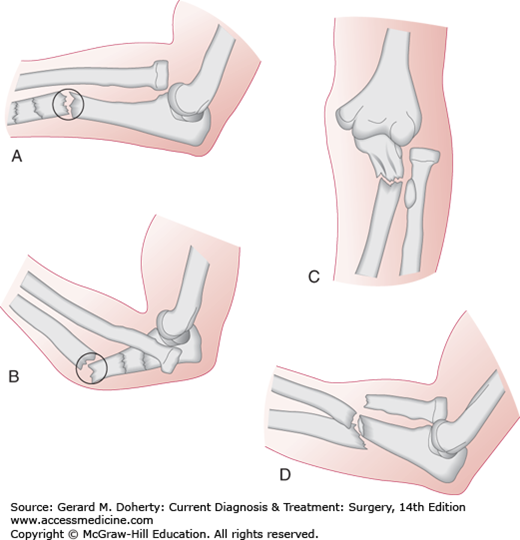
The elbow is a modified hinge joint consisting of three separate articulations: ulnohumeral, radiohumeral, and proximal radioulnar. The elbow joint is intrinsically stable with bony and soft tissue contributions. The trochlea-olecranon fossa, coronoid fossa, radiocapitellar joint, biceps, triceps, and brachioradialis provide anterior-posterior stability during flexion and extension. On the medial side of the elbow the anterior bundle of the medial collateral ligament (MCL) is the primary stabilizer to valgus stress, while the lateral ulnar collateral ligament is the primary stabilizer on the opposite side of the elbow preventing posterolateral instability. Normal elbow range of motion entails 0-150 degrees of flexion, 85 degrees of supination, and 80 degrees of pronation. Functional range of motion requires 30-130 degrees of flexion, 50 degrees of pronation, and supination. Elbow injury mandates careful examination of the entire upper extremity including shoulder and wrist, with thorough neurovascular examination. AP, lateral, and oblique radiographs are required to adequate visualize the elbow joint.
The distal humerus can be conceptualized as medial and lateral columns, each roughly triangular in shape and composed of a condyle articulating with the bones of the forearm and an epicondyle (distal part of the humerus that flares just above the elbow joint at the level of the supracondylar ridge) connecting to the shaft of the humerus. These fractures can be classified descriptively: intercondylar (most common), supracondylar fractures (extension or flexion type), transcondylar, condylar, capitellum, trochlea, lateral epicondyle, medial epicondyle, or fractures of the supracondylar process. These fractures can also be classified using the AO system based on the concept of column integrity and articular involvement. Type A fractures are extra-articular (epicondylar, supracondylar, transcondylar) fractures. Type B fractures only involve a portion of the articular surface (unicondylar or intercondylar). Type C fractures involve the entire distal articular surface.
Standard AP, lateral, and oblique radiographs should be obtained. Traction radiographs or computed tomography may provide better fracture pattern visualization for preoperative planning. On the lateral radiograph, the anterior or posterior “fat pad sign” representing displacement of the adipose layer over the joint capsule may be the only indication of a nondisplaced distal humerus fracture. The AP radiograph should be carefully scrutinized for an intercondylar split. If an intercondylar split is present, the amount of rotation, in addition to displacement and fracture comminution should be noted.
The patient can be initially managed with a posterior long-arm splint with the elbow flexed at 90 degrees and the forearm neutral. Nonoperative treatment is indicated for nondisplaced or minimally displaced fractures. Surgery is indicated for displaced fractures, vascular injury, or open fracture.
Supracondylar fractures are much more common in children. There are two types: extension (distal fragment is displaced posteriorly) and flexion (distal fragment is displaced anteriorly). Nondisplaced, minimally displaced, and severely comminuted fractures in the elderly with limited functional needs may be treated nonoperatively. Posterior splint immobilization is continued for 1-2 weeks after which gentle range of motion exercises are begun. The splint may be discontinued and weight bearing advanced after six weeks if signs of radiographic healing are appreciated. Surgical options include open reduction internal fixation with plates and screws. Total elbow replacement may be considered in elderly patients who were otherwise active with good preinjury function with severely comminuted fractures not amenable to ORIF.
Nonoperative treatment is indicated for nondisplaced or minimally displaced fractures or for debilitated elderly patients with poor function preinjury. Range of motion exercises should be initiated as soon as the patient is able to tolerate therapy. Surgical options include ORIF or total elbow arthroplasty.
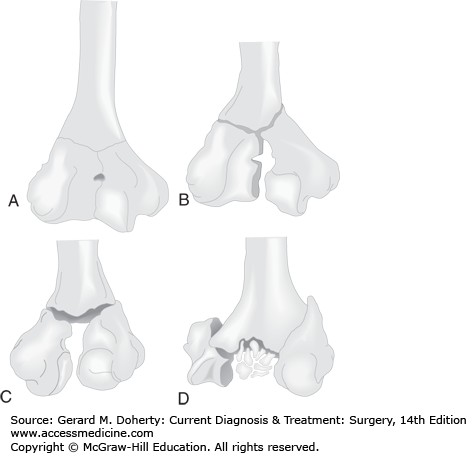
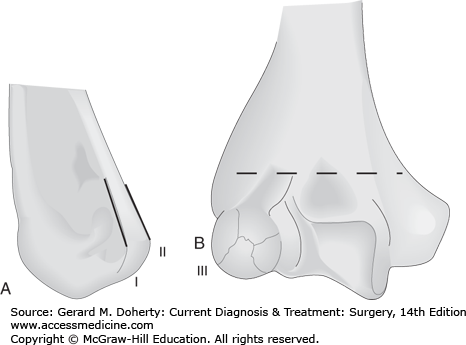
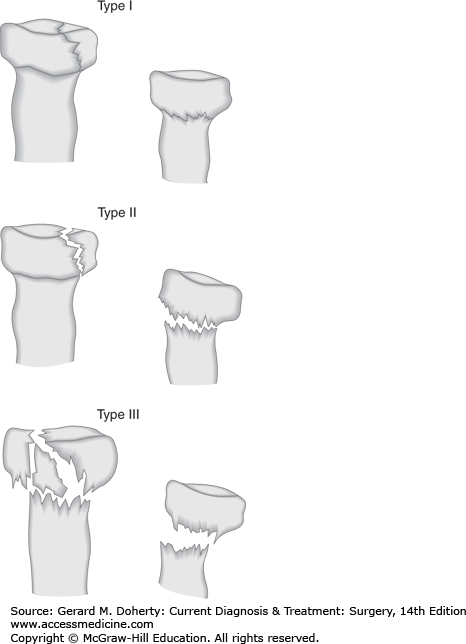
Intercondylar fractures are the most common type of distal humerus fracture in adults. Fracture fragments are often displaced due to opposing muscle forces on the medial (flexor mass) and lateral (extensor mass) epicondyles, causing rotation of the articular surfaces (Figure 40–4). Fractures can be classified as type I (nondisplaced), type II (slight displacement with no rotation between the condylar fragments), type III (displacement with rotation), and type IV (comminution of the articular surface). Nonoperative treatment with two weeks of immobilization followed by range of motion exercises is indicated for nondisplaced fractures. Type IV fractures in the elderly with osteopenic bone can be treated with the “bag of bones” technique which entails very short-term immobilization with early range of motion. Open reduction internal fixation with dual plates is the preferred surgical treatment. Early range of motion is critical to prevent stiffness, unless fixation is tenuous. TEA is another option.
Medial or lateral condyle fractures are rare in adults (Figure 40–5). Type I (Milch classification) fractures do not traverse the lateral trochlear ridge. Involvement of the lateral trochlear ridge (type II) leads to medial-lateral instability. Nonoperative treatment, entailing a posterior splint with elbow flexed to 90 degrees and the forearm supinated for lateral condyle fractures or pronated for medial epicondyle fractures, may be pursued for nondisplaced or minimally displaced fractures. Open or displaced fractures can be treated surgically with screw fixation with or without collateral ligament repair as needed.
Capitellum fractures are rare, representing less than 1% of all elbow fractures. Due to lack of significant soft tissue attachments, these fractures may result in a free articular fragment that may displace anteriorly into the coronoid or radial fossa causing a block to elbow flexion. These fractures typically result from a fall on an outstretched arm with the force transmitted through the radial head to the capitellum. Occasionally, radial head fracture may also be present. Capitellum fractures can be classified as follows (Figure 40–6): type I “Hahn-Steinthal” large osseous fragment with or without trochlear involvement, type II “Kocher-Lorenz” fragment articular cartilage with minimal subchondral bone attached, and type III (significant comminution). Nonoperative treatment, reserved for nondisplaced fractures, consists of immobilization in a posterior splint followed by elbow range of motion exercises. Surgical treatment entails ORIF with screws or excision for type II fractures, severely comminuted type I fractures or chronic missed fractures with limited range of motion.
Figure 40–6.
Fractures of the capitellum. The type I fracture involves a large portion of bone, often the entire structure. Type II is a shear fracture, often with minimal subchondral bone, and may displace posteriorly (A). A type III fracture is a comminuted fracture with varying amounts of displacement of the fracture fragments (B).
These fractures are extremely rare and associated with elbow dislocation. Nondisplaced fractures can be treated with posterior splint for three weeks, followed by elbow range of motion exercises. Displaced fractures are treated with ORIF; fragments not amenable to internal fixation can be excised.
Lateral epicondyle fractures can be treated with symptomatic immobilization with early range of motion. Nondisplaced or minimally displaced medial epicondyle fractures can be treated with immobilization in posterior splint with the forearm pronated, wrist and elbow flexed for 10-14 days. ORIF is indicated for displaced fractures, especially in the presence of ulnar nerve symptoms, valgus stress instability, wrist flexor weakness, and symptomatic nonunion.
The supracondylar process is osseous or cartilaginous projection arising from the anteromedial surface of the humerus. The ligament of Struthers which connects the supracondylar process to the medial epicondyle is a fibrous arch through which the median nerve and brachial artery passes. Most of these fractures are amenable to closed treatment with symptomatic posterior splint immobilization followed by early range of motion. Median nerve or brachial artery compression are indications for surgical exploration and release.
Elbow dislocation most commonly results from a fall on an outstretched hand. A careful neurovascular examination along with AP and lateral radiographs of the elbow are required. Simple elbow dislocation (no associated fracture) are classified according to the direction of displacement of the ulna relative to the humerus: posterior (most common type), posterolateral, posteromedial, lateral, medial, and anterior (Figure 40–7). Acute elbow dislocations should undergo closed reduction with patient under sedation and adequate anesthesia as soon as possible. For posterior dislocation, the reduction maneuver entails longitudinal traction with elbow flexion. Postreduction range of motion exam, neurovascular exam, and radiographs should be performed, followed by placement in a posterior splint with 90 degrees of flexion. A block to full range of motion may indicate an incarcerated fracture fragment or inadequate reduction. If reduction does not restore arterial flow, angiography, and immediate operative intervention are warranted. Postreduction films should be carefully evaluated for concentric reduction and associated fractures (medial or lateral epicondyle, radial head, coronoid process). Elbow dislocation with radial head and coronoid process fractures is known as the “terrible triad”, due to associated instability. Surgical intervention is indicated when the elbow cannot be held concentrically reduced position, redislocates, or if the dislocation is deemed unstable (if the elbow dislocates prior to reaching 30 degrees of flexion from a fully flexed position). Recovery of motion and strength may take 3-6 months. The most common complication is stiffness, associated with prolonged immobilization. Recently, the trend has been to immobilize elbows for one week postinjury, and then start range of motion exercises. If symptomatic heterotopic ossification is present, excision can be pursued 6 months or longer after injury.
The olecranon is the most proximal palpable portion of the ulna. The subcutaneous position of the olecranon causes it to be especially susceptible to direct trauma. Posteriorly, the triceps tendon envelops the articular capsule before it inserts on to the olecranon. As a result, displaced fractures of the olecranon represent a functional disruption of the triceps mechanism, resulting in loss of active elbow extension. Anteriorly, the olecranon forms the greater sigmoid (semilunar) notch of the ulna, which articulates with the trochlea. The most proximal anterior portion of the ulna is the coronoid process, which lends stability to the elbow joint.
Olecranon fractures may result from a direct blow (fall on to the tip of the elbow) resulting in a comminuted olecranon fracture, or fall onto an outstretched arm accompanied by a strong, sudden triceps contraction resulting in a transverse or oblique fracture. Careful neurovascular exam followed by AP and lateral radiographs should be part of the initial evaluation. A true lateral radiograph should be carefully scrutinized for the extent of the fracture, any displacement of the radial head (the radial head should point toward the capitellum in all views; if this is not the case subluxation or dislocation is present), degree of comminution and articular surface involvement. Olecranon fractures are classified based on fracture pattern (transverse, transverse-impacted, oblique, comminuted, oblique-distal, or fracture dislocation) or according to the Mayo classification: type I (nondisplaced or minimally displaced), type II (displacement without elbow instability), type III (fracture with features of elbow instability). The goals of treatment are to restore articular congruity, restoration, and preservation of the elbow extensor mechanism and range of motion.
Nondisplaced fractures or displaced fractures in the elderly with poor preinjury function can be managed with closed treatment in a long-arm splint or cast with the elbow flexed from 45-90 degrees. Careful follow-up with radiographs should be done at weekly intervals for at least 2 weeks. In general, there is sufficient stability at 3 weeks to allow early motion from full extension to 90 degrees of flexion, with progression of flexion at 6 weeks. Of note some authors are advocating earlier range of motion at one week out from injury to prevent stiffness.
Indications for surgery include any disruption of the extensor mechanism (any displaced fracture) or articular incongruity. Multiple surgical options are available, including intramedullary fixation, tension band wiring, plate and screws, and excision. Postoperatively the patient should be placed in a posterior splint with early range of motion.
The most frequent complication of these fractures is prominent implants that subsequently require removal after healing has occurred. Elbow stiffness and loss of fixation have also been reported.
The coronoid process is the anterior beak-shaped portion of the ulna, forming the buttress anteriorly of the greater sigmoid notch. The anterior portion of the MCL attaches here, as well as a portion of the anterior capsule, contributing to elbow stability.
Isolated fractures of the coronoid are uncommon and are more frequently associated with posterior elbow dislocations or other fractures about the elbow. The mechanism of injury is usually forced posterior displacement of the proximal ulna as with a dislocation or hyperextension force of the elbow. Oblique radiographs may aid evaluation of these fractures as they are sometimes difficult to see on lateral and anteroposterior views.
These fractures have been classified by Regan and Morrey based on the size of the fracture fragment (Figure 40–8): type I (coronoid process tip avulsion), type II (single or comminuted fragment involving 50% or less of the coronoid process), type III (a single or comminuted fragment involving > 50% of the process). Type I fractures can be treated with immobilization in flexion for 3 weeks (or less if the fragment and elbow are stable). Associated fractures should be treated as appropriate in each case with the goal of fracture stability for early range of motion. Isolated coronoid fractures without elbow instability can be treated in the same way as type I fractures. Unstable type II fractures and type III fractures usually require operative intervention.
Radial head fractures typically result from a fall on an outstretched arm causing an axial load collision between the radial head and capitellum. Patients typically present with limited elbow and forearm motion, along with pain with passive range of motion of the forearm. The forearm and wrist should be examined for any tenderness which may indicate the presence of an Essex-Lopresti type injury (radial head-fracture dislocation with associated interosseous ligament and distal radioulnar joint disruption). After documentation of neurovascular status, anteroposterior, lateral, and radial head view radiographs should be evaluated for fracture. Nondisplaced fractures should be suspected if a fat pad sign is present without obvious fracture. If Essex-Lopresti injury is suspected, additional radiographs of the forearm and wrist are indicated as well.
The Mason classification system is used to describe these fractures (Figure 40–9): type I (nondisplaced fractures), type II (marginal fractures with displacement), type III (comminuted fractures involving the entire radial head), and type IV (fracture associated with elbow dislocation).
Assessment of range of motion and stability to valgus stress is critical and can be performed after aspiration of the hemarthrosis and injection of lidocaine. This can be done through direct lateral needle insertion at the “soft spot” between the olecranon, radial head, and capitellum. Any mechanical block to motion should be carefully documented, as this can affect treatment decision-making.
Most isolated radial head fractures are treated with a brief period of immobilization in a sling followed by early range of motion 24-48 hours after the injury. Surgery is indicated for mechanical block to range of motion and type three fractures. A relative indication for surgery is displacement of a large fragment (> 2 mm); however, this is controversial. Surgical treatment options include ORIF, fragment excision with or without prosthetic replacement. Type IV injuries should be treated with closed reduction, followed by additional treatment based off of the above outlined criteria.
Forearm fractures are more common in men than women, secondary to a higher incidence of motor vehicle collisions, athletic injury, altercations, and falls from height experienced by men. The forearm acts as a ring: a fracture that significantly shortens the radius or ulna will cause disruption of the proximal radio-ulnar joint or distal radio-ulnar joint. The ulna acts as an axis around which the laterally bowed radius rotates during supination and pronation. The interosseous membrane occupies the space between the radius and ulna; it provides a significant contribution to forearm stability.
Clinical assessment includes careful neurovascular exam (median, radial, and ulnar nerves) and assessment of any open wounds (even superficial wounds) can expose an ulna fracture to the outside world due to its subcutaneous position. Practitioners should have a high index of suspicion for compartment syndrome, if pain out of proportion, tense compartments, or pain on passive stretch is present. Both-bone forearm fractures or fracture of one bone with concomitant injury to the elbow or wrist joint are more common than a fracture to either bone in isolation. As a result, it is crucial to obtain anteroposterior and lateral radiographs of the forearm that include both the wrist and elbow joints. The radial head must be aligned with the capitellum on all views to rule-out subluxation or dislocation.
Forearm fractures can be classified from a descriptive standpoint (closed vs. open, location, comminuted, segmental, multifragmented, displacement, angulated, and rotational alignment).
Radial shaft fractures can result from direct trauma or indirect trauma such as a fall on an outstretched hand. Although, isolated fractures of the proximal two-thirds of the radius are possible, a fracture of the distal one-third should raise high suspicion for concomitant injury to the distal radial-ulna joint (DRUJ). Nondisplaced fractures can be managed closed in a long-arm cast. Any displacement, loss of radial bow, or concomitant injury to the DRUJ is surgical indications. Fractures of the radius are typically fixed with open reduction internal fixation with 3.5 mm DCP plates.
This is a fracture of the shaft of the radius (most commonly the distal third) in conjunction with a distal radioulnar joint injury. Wrist pain on physical examination should arouse suspicion. The diagnosis should be confirmed radiographically. DRUJ disruption is suggested by the following radiographic findings: fracture at the base of the ulnar styloid, widening of the distal radioulnar joint space on the anteroposterior radiograph, subluxation of the ulna, and radial shortening greater than 5 mm relative to the distal ulna.
In adults, these injuries should always be treated surgically with open reduction and internal fixation, along with intraoperative evaluation of the DRUJ. After fixing the radius, if the joint is stable through full pronation and supination, only short-term immobilization in a splint is required to protect the incision. If the joint can be reduced but is unstable with rotation, additional surgical treatment is necessary. If there is a repairable ulnar styloid fracture, then open reduction with internal fixation of this piece will result in a stable DRUJ. If there is no ulnar styloid fracture but the distal radioulnar joint is reducible but unstable with rotation, then two 0.0625-inch Kirschner wires are used to pin the distal ulna to the radius in a reduced position (usually supination). With both open reduction with internal fixation of the ulnar styloid and the use of transfixing pins, the forearm should be immobilized in full supination in an above-elbow cast or brace for 4-6 weeks. The transfixing pins are removed prior to allowing forearm range of motion. Rarely, the distal radioulnar joint cannot be reduced. In this instance, a dorsal approach to the joint is used to extract interposed tissues (extensor carpi ulnaris is most common) blocking reduction.
Ulna night stick fractures usually results from a direct blow to the ulna along its subcutaneous border. Careful neurovascular examination and radiographs of the forearm including the wrist and elbow are essential. Radiographs should be carefully scrutinized for elbow dislocation; the radial head should point to the capitellum in all views or a Monteggia variant may be present. Nondisplaced or minimally displaced fractures may be treated acutely in a sugar tong splint. When swelling has subsided (after 7-10 days), the patient’s arm can be transitioned to a long-arm cast or functional brace. Displaced fractures (> 10 degrees of angulation or > 50% displacement of the shaft) are best treated surgically with open reduction internal fixation.
Monteggia’s fracture is a fracture of the proximal ulna with a radial head dislocation. Thorough neurovascular exam is necessary; injuries to the radial nerve or posterior interosseous nerve have been described. The Bado classification is based of the direction of the radial head dislocation: type I (anterior), type II (posterior), type III (lateral or anterolateral), and type IV (anterior dislocation with a fracture of the radius and ulna) (Figure 40–10).
Figure 40–10.
Monteggia’s fractures. The classification of Monteggia lesions by Bado. A. Type I: anterior angulation of the ulnar fracture and anterior dislocation of the radial head. B. Type II: posterior angulation of the ulnar fracture and anterior dislocation of the radial head. C. Type III: fracture of the proximal ulna metaphysis and lateral dislocation of the radial head. D. Type IV: anterior dislocation of the radial head and fracture of the radial and ulnar shafts. (Reproduced, with permission, from Browner B et al: Skeletal Trauma. Saunders, 1992.)
Closed reduction and casting of Monteggia fractures should only be attempted in children. These injuries are typically treated with open reduction internal fixation with plates and screws. Of note failure of the ulna to reduce may indicate annular ligament interposition. If open reduction of the radial head is necessary, consideration should be given toward repairing the annular ligament. Postoperatively, if the repair is considered stable, the patient can be placed in a posterior splint for 7-10 days, followed by beginning range of motion exercises.
Fractures of both radius and ulna are usually the result of high energy mechanisms (motor vehicle accidents or fall from a height). The fractures are most often displaced. Careful examination to rule out neurovascular injury and compartment syndrome should be performed. Radiographs of the entire forearm including the elbow and wrist are necessary.
Treatment for both-bone forearm fractures in adults consists of open reduction and internal fixation with compression plating using 3.5-mm dynamic plates. The goal of plate fixation is to restore: the normal ulnar and radial length, rotational alignment, and radial bow (which have been shown to be essential for rotation of the arm). With solid fixation, active range of motion of the forearm and elbow can be started at 10-14 days. Open fractures can also be treated successfully with these methods. However, if there is excessive soft tissue damage or wound contamination, the use of an external fixator may be a preferable option.
Complications of this fracture include nonunion, malunion, infection, neurovascular injury, compartment syndrome, synostosis, and loss of motion.
The distal radius has three articulations: the sigmoid notch which articulates with the ulna, and facets for the scaphoid and lunate bones. The base of the ulna styloid serves as an insertion point for the triangular fibrocartilage complex (TFCC) which is the primary stabilizer of the DRUJ. Normally, 80% of the axial load is supported by the distal radius and 20% by the ulna and TFCC. There are six dorsal compartments of the wrist that contain wrist and digital extensor tendons. On the volar surface, the pronator quadratus lies across the distal radius and ulna. Just anterior to the pronator quadratus are the contents of the carpal canal, containing nine digital flexor tendons and the median nerve. Anterior to the transverse carpal ligament lie the flexor carpi radialis, flexor carpi ulnaris, and palmaris longus muscles. Guyon’s canal contains the ulnar nerve and artery. It is bounded by the volar retinacular ligament and flexor retinacular ligament, the hook of the hamate radially, and the pisiform ulnarly.
Extrinsic ligaments connect the radius to the carpus and the carpus to the metacarpals. The proximal row of carpal bones consisting of the scaphoid, lunate, triquetrum, and pisiform bones, are attached to the distal radius via two sets of radiocarpal ligaments (volar and distal). The volar radiocarpal ligaments (radioscaphocapitate, radioschapolunate, radiolunate, and radiolunotriquetral) are stronger and confer more stability to the radiocarpal articulation when compared to the dorsal radiocarpal ligaments. The radiocarpal joint is the primary joint for wrist motion (70 degrees of flexion/extension, 20 and 40 degrees of radial and ulnar deviation, respectively).
Intrinsic ligaments connect carpal bone to carpal bone (eg, scapholunate, etc). The distal carpal row, consisting of the trapezium, trapezoid, capitate, and hamate, is connected to each other and the base of the metacarpals with strong extrinsic ligaments. As a result, the distal carpal row is relatively immobile. The lunate is the key to carpal stability; injury to the scapholunate or lunotriquetral ligaments leads to unstable motion of the lunate and generalized carpal instability. Disruption of the scapholunate ligament or scaphoid fracture can lead to excessive dorsiflexion of the lunate and triquetrum (dorsal intercalated segmental instability). Injury to the lunotriquetral ligament leads to volar flexion of the lunate (volar intercalated segmental instability). The space of Poirer (ligament-free area between the capitate and lunate) is a potential area of weakness.
Normal anatomic relationships include radial inclination of 23 degrees, 11 mm of radial length, 11-12 degrees of palmar tilt, a 0 degree capitolunate angle (straight line drawn from the shaft of the third metacarpal, through the capitate and lunate with the wrist in a neutral position), a 47 degree scapholunate angle, and less than 2 mm of scapholunate space.
The vascular supply to the wrist consists of the radial, ulnar, and anterior interosseous arteries intertwining to form a network of arterial arches on the volar and dorsal surfaces of the carpal bones. The radial artery gives off branches that supply the scaphoid volarly (supplies distal scaphoid) and dorsally (supplies proximal scaphoid). The lunate typically receives blood supply from dorsal and volar surface branches.
More than 450,000 distal radius fractures occur annually in the United States, representing one-sixth of all fractures treated in emergency departments. The incidence of distal radius fractures increases with old age and osteopenia.
The most common mechanism for a distal radius fracture is fall on to an outstretched dorsiflexed hand. High-energy mechanisms such as motor vehicle collisions and falls from height can result in highly displaced or significantly comminuted fractures in younger patients.
Patients typically present with a swollen, ecchymotic, tender wrist. Deformity of the wrist is variable with dorsal displacement of the distal segment (Colles fracture) being more common than volar (Smith-type fracture). The ipsilateral elbow and shoulder should be carefully evaluated for concomitant injury. Careful neurovascular examination is paramount including the motor and sensory median, ulnar, and radial nerve distributions (Motor: a-ok, finger spread, and thumbs up signs; Sensory: volar aspect of the thumb, index, middle fingers, volar aspect of the small finger, and dorsal aspect of the thumb). Particular attention should be given to median nerve function as carpal tunnel syndrome is a relatively common complication (13%-23%) due to traction injury, fracture fragment trauma, hematoma, or increased compartment pressure.
Posteroanterior and lateral views of the wrist should be obtained. Elbow and shoulder symptoms should also be evaluated radiographically. Contralateral wrist views may be used for comparison ulnar variance and the DRUJ. Computed tomography scan can be useful for further characterization of intra-articular involvement and preoperative planning. Normal radiographic relationships include the following averages: 23 degrees of radial inclination, 11 mm of radial length, and 11 degrees of palmar or volar tilt.
Distal radius fractures can be characterized descriptively—open versus closed, displacement, angulation, comminution, and loss of radial length. The Frykman classification organizes these fractures based on the degree of articular involvement as well concomitant fracture of the distal ulna (Figure 40–11). Higher classification fractures have worse prognoses.
AO/ASIF CLASSIFICATION OF DISTAL RADIUS FRACTURES
Type A: Extra-articular fractures
Isolated distal ulnar fracture
Simple radius fracture
Radial fracture with metaphysial impaction
Type B: Intra-articular complex fracture
Radial styloid fracture
Dorsal rim fracture
Volar rim fracture
Type C: Intra-articular complex fracture
Metaphysial fracture with radiocarpal congruity preserved
Articular displacement
Diaphysial-metaphysial involvement
Figure 40–11.
Frykman classification of distal radius fractures. Types I, III, V, and VII do not have an associated fracture of the distal ulna. Fractures III-VIII are intra-articular fractures. Higher classification fractures have worse prognoses. (Reproduced, with permission, from Green D, Hotchkiss R, Pederson W: Green’s Operative Hand Surgery. Churchill Livingstone, 1993.)
Emergent operative management is indicated for open fractures. Acute surgical intervention should be considered for distal radius fractures complicated by carpal tunnel syndrome that is not relieved with closed reduction.
All distal radius fractures should undergo closed reduction, even if surgical intervention is expected. The benefits of fracture reduction include limiting postinjury swelling, pain relief, and median nerve decompression. Although casting may be considered for nondisplaced or minimally displaced fractures with minimal swelling, a sugar-tong splint is generally preferred encompassing the dorsal and volar aspects of the wrist, limiting subsequent forearm rotation and possible fracture displacement. One week post injury the patient may be transitioned to a long-arm cast. If closed treatment is planned, radiographic evaluation should be done on a weekly basis for the first two to three weeks to monitor for displacement. Acceptable radiographic parameters for continued closed treatment include: radial length within 2-3 mm of the contralateral wrist, neutral palmar tilt (0 degrees), intra-articular step off less than 2 mm, and radial inclination less than 5-degree loss. Surgery is indicated if reduction with respect to the above stated parameters cannot be achieved or maintained.
Hematoma block, Bier block, or conscious sedation can be used to provide analgesia. Hematoma block offers the benefit of speed and does not require that the patient have been without oral intake for a significant amount of time. Conscious sedation offers the benefit of muscle relaxation facilitating reduction. Initially manual or fingertrap-assisted traction is applied facilitating reduction via ligamentotaxis. For dorsally tilted fractures, volar directed pressure is applied to the distal fracture segment. C-arm if available can be used to assess fracture reduction. Once reduction is adequate a well-molded long-arm (“sugar tong”) splint can be applied with the wrist in neutral and the metacarpaphalangeal joints free.
Many surgical options are available. Choice of operation is determined by several factors, including the fracture pattern, bone quality, and surgeon preference.
Reduction is achieved via closed means, followed by fixation typically with 0.0625-inch Kirschner wires. Interfragmentary technique entails wires used to stabilize a fracture and prevent collapse after reduction is achieved. With intrafocal technique where these wires are driven into the fracture site, used to lever the pieces achieving reduction, and then driven through the opposite cortex to maintain reduction. Postoperatively patients are placed in a splint or cast. The wires are typically removed after 6 weeks once bone healing is appreciated radiographically.
This technique uses ligamentotaxis to restore radial length and radial inclination, but it rarely restores palmar tilt. It is especially useful for treating very comminuted or intra-articular fractures where there are several small pieces. External fixation is also useful for treating open fractures with severe tissue compromise or as a temporizing measure when a patient has other critical medical issues that need immediate attention.
In recent years, volar plating has become much more popular compared to dorsal plating due to its advantages when treating distal radius fractures with significant dorsal comminution, as well as the extensor tendon complications associated with dorsal plating of the distal radius.
Stiffness of the wrist and digits is common. Patients should be instructed to begin range of motion exercises for the digits immediately after the fracture is initially treated. Include median nerve dysfunction, malunion, nonunion, stiffness, posttraumatic arthritis, tendon rupture, finger, wrist, and elbow stiffness. Articular congruity post surgical fixation is critical for avoiding the development of posttraumatic arthritis.
Also called a “chauffeur’s fracture,” “backfire fracture,” or “Hutchinson fracture” this is an avulsion fracture with extrinsic ligaments remaining attached to the styloid fragment. This injury is often associated with intercarpal ligamentous injuries such as scapholunate dislocation or perilunate dislocation. This injury often requires open reduction with internal fixation.
Fractures of the ulnar styloid are commonly seen in conjunction with distal radius fractures and can also be seen in isolation. Fractures of the tip of the ulnar styloid are often too small to fix. However, large fragments (the entire styloid from its base) may be indicative of a TFCC disruption that can lead to DRUJ instability. As a result, these displaced fractures should be treated with open reduction and internal fixation.
DRUJ dislocation is discussed earlier in the section describing the Galeazzi fracture. DRUJ dislocation can also occur with a simple distal radius fracture. Careful examination of radiographs and the distal radioulnar joint will keep the clinician from missing this injury in the face of a distal radius fracture.
Most carpal bone fractures occur in the proximal carpal row, with the scaphoid being the carpal bone most commonly fractured. Carpal bone fractures usually occur in younger people, often from high energy falls on an outstretched hand Wrist radiographs can be difficult to interpret, and careful scrutiny is necessary so as not to miss these injuries. In addition to the standard anteroposterior, lateral, and oblique views of the wrist, special radiographic views such as a scaphoid view (anteroposterior radiograph with the wrist supinated 30 degrees and in ulnar deviation), clenched fist view (to evaluate for carpal instability), or carpal tunnel view can often be helpful. Computed tomography is also useful to identify fractures if radiographs are inconclusive; MRI is sensitive for detecting occult fractures, osteonecrosis of carpal bones, and soft injuries including disruption of the scapholunate ligament or TFCC.
The scaphoid is the carpal bone most commonly fractured. Anatomically, the scaphoid is divided into proximal and distal poles, a tubercle, and a waist. The blood supply for the scaphoid comes largely from branches of the radial artery traveling from a distal to proximal location. As a result, fractures of the scaphoid at the waist or more proximal are particularly prone to nonunion or avascular necrosis.
Fractures of the scaphoid most commonly occur as a result of a fall on an outstretched hand. Patients typically present with pain on the radial side of their wrist and tenderness to palpation over the anatomic snuffbox. Physical examination maneuvers include the scaphoid lift test (reproduction of pain with dorsal-volar shifting of the scaphoid) and the Watson test (painful dorsal scaphoid displacement as the wrist is moved from ulnar to radial deviation with compression of the tuberosity). Radiographic evaluation includes a “scaphoid view,” in addition to the standard wrist series. Initial radiographs are nondiagnostic in up to 25% of cases. As a result, if clinical exam suggests a scaphoid fracture, it is appropriate to employ a trial of immobilization with repeat radiographs in 1-2 weeks. Additionally, technetium bone scan, MRI, or CT scan can be used to diagnose occult scaphoid fractures that continue to not be visualized on radiograph, despite persistent pain. Scaphoid fractures can be classified based on the pattern (horizontal oblique, transverse, vertical oblique), displacement (nondisplaced fractures with no step-off are considered stable, displaced fractures > 1 mm, scapholunate angulation > 60 degrees, radiolunate angulation > 15 degrees), and location (tuberosity, distal pole, waist, and proximal pole). Nondisplaced fractures should be treated in a long-arm thumb spica cast for 6 weeks. After 6 weeks, the patient’s wrist can be placed in a short-arm spica cast until the fracture is united. Expected time to union for distal third fractures is 6-8 weeks, 8-12 weeks for middle third fractures, and 12-24 weeks for proximal third fractures. Surgical indications include fracture displacement more than 1 mm, radiolunate angle more than 15 degrees, scapholunate angle more than 60 degrees, humpback deformity, or nonunion. Complications of scaphoid fractures include fracture nonunion or avascular necrosis (Figure 40–12). Patients with long-standing scaphoid nonunions go on to develop early arthritis of the radioscaphoid joint secondary to altered mechanics of the wrist.
The lunate is the carpal bone most likely to dislocate, but fractures are rare. Fractures usually result from a fall on an outstretched hand. Patients typically present with tenderness to palpation over the volar wrist overlying the distal radius and lunate with painful range of motion. Radiographs are usually not helpful due to overlapping densities of multiple bones; CT, MRI, or bone scan are usually required to make the diagnosis. Nondisplaced fractures can be treated in a short- or long-arm cast. Displaced or angulated fractures require surgical treatment. Osteonecrosis (Keinbock’s disease), can complicate this injury leading to advanced collapse and radiocarpal degeneration. Several surgical treatments are available for this sequella.
This fracture generally occurs from a direct blow to the area such as occurs when swinging a baseball bat or golf club that suddenly comes to an abrupt stop as it encounters a firm surface. Patients present with ulnar-sided hand pain over the hamate. Fracture will often not be seen on routine wrist and hand radiographs. A carpal tunnel view (20 degree supination oblique view of the wrist) should be obtained if this fracture is suspected. If the diagnosis is suspected clinically but the radiographs show no fracture, a CT scan may be helpful. Nondisplaced fractures may be treated in a short-arm cast for six weeks. Displaced fractures of the body can be treated with open reduction internal fixation with screws or wires.
Fractures can occur in any of the other carpal bones as well, but much less commonly. Triquetral avulsion or dorsal impaction fractures can occur from falls on the outstretched hand. Isolated fractures of the remaining carpal bones are rare and generally occur with high-energy trauma and other injuries.
Severe injury to the wrist causing damage to the complex ligamentous structures may lead to carpal bone dissociation, carpal dislocations, and fracture dislocations. The lunate is often called the “carpal keystone”; its ligamentous attachments to the radius and other carpal bones make a significant contribution to radiocarpal stability. A sequence of progressive perilunate instability starts with scapholunate disruption (stage I), then midcarpal or capitolunate disruption (stage II), lunotriquetral disruption (stage III), ending in disruption of the radiolunate joint leading to volar lunate dislocation (stage IV).
Scapholunate dissociation secondary to disruption of the scapholunate and the radioscapholunate ligament leads to altered kinematics of the wrist and early degenerative arthritis. Clinical findings include volar wrist tenderness/bruising, positive Watson test, pain with grasping, and decreased grip strength. Radiographically, widening of the scapholunate space more than 3 mm (“Terry Thomas” sign), or scapholunate angle more than 70 degrees on the lateral are indicative of scapholunate disruption. Closed reduction with an audible, palpable click followed by thumb spica immobilization for 8 weeks is the first line of treatment. Inability to obtain or maintain reduction is surgical indications.
Lunotriquetral dissociation occurs as a result of disruption of the radiolunotriquetral ligament. Patients typically present with swelling over the peritriquetral area and tenderness dorsally, typically 1-2 cm distal to the ulnar head. Radiographs may show disruption of the normal proximal carpal row contour; frank gapping of the lunotriquetral space is rarely seen. Treatment with a short arm cast for 6-8 weeks or closed reduction with pinning of the lunate to the triquetrum is warranted.
Carpal dislocations represent a continuum of perilunate ligamentous injury with frank lunate dislocation being the final stage. Patients present with severe wrist pain and swelling after trauma. Most dislocations can be diagnosed with adequate AP and lateral views of the wrist. With a perilunate dislocation, the lunate remains in its normal position, articulating with the distal radius, but is angled in a volar direction, and the rest of the carpus is dislocated. With lunate dislocation, on the lateral radiograph the lunate will be volar to the rest of the carpus and not in alignment with the distal radius. Treatment of carpal dislocations is accomplished with closed reduction of the midcarpal joint via traction combined with direct manual pressure over the capitate and lunate. Irreducible dislocations or unstable injuries should be treated surgically with open reduction internal fixation.
Ulnocarpal dissociation may result from disruption of the TFCC, where the lunate and triquetrum assume a supinated and palmar flexed position, while the distal ulna subluxes dorsally. Radiographs may show ulnar styloid avulsion or dorsal displacement of the ulna; MRI may demonstrate TFCC tear. Treatment requires operative repair of the TFCC and/or ORIF of large displaced ulnar styloid fragments.
Even with the best care, carpal bone and ligament injuries can be devastating, with long-term sequelae of pain, stiffness, and early arthritis.
Metacarpal and phalangeal fractures are relatively common comprising a significant portion of emergency department visits. The significant variation in mechanism of injury accounts for the large number of different types of fracture patterns seen in hand injuries. Axial load or “jamming” injuries often result in shearing articular fractures or metaphyseal compression fractures, sometimes with concomitant injury to the carpus, forearm, elbow, and shoulder due to force transmission. Injury mechanisms with a bending component result in diaphyseal fractures or joint dislocations. Individual digits or joints caught in clothing or equipment can result in spiral fractures or complex dislocations. Industrial settings with heavy objects predispose to crushing mechanisms of injury. The direction of fracture angulation depends on the deforming forces caused by attached muscle. The palmar and dorsal interosseous muscles arise from the metacarpal shafts, usually flexing the fracture causing apex-dorsal angulation. Proximal phalynx fractures typically angulate in the opposite direction, apex-volar. Middle phalynx fractures angulate variably, while distal phalynx fractures are usually comminuted tuft fractures resulting from crush injuries. Clinical evaluation includes documentation of the patient’s age, hand dominance, occupation, mechanism of injury, time of injury, exposure to contamination, and financial issues (workman’s compensation). Physical examination should document neurovascular status, and pay particular attention range of motion, angulation, and malrotation (best evaluated when the intervening joint is flexed to 90 degrees). Radiographic evaluation includes AP, lateral, and oblique radiographs of the hand and the specific injured digit. Fractures can be classified descriptively: open versus closed, location, fracture pattern (comminuted, transverse, spiral, vertical split, extra-articular versus intra-articular, stable versus unstable, and angulational or rotational deformity. Fractures of the small bones of the hand heal more rapidly than fractures of larger bones, and prolonged immobilization can cause stiffness and loss of motion that can be difficult or impossible to regain. As a result, fractures of the metacarpals and phalanges should not be immobilized for more than 3 weeks except under rare circumstances, due to subsequent development of stiffness. The safe position for splinting or casting of the hand is with slight wrist extension, the MP joints flexed 60-90 degrees, and the PIP and DIP joints extended. This “intrinsic plus” position, puts the ligaments of the hand on maximum stretch, avoiding posttreatment stiffness.
These types of fractures require special consideration. Open fractures of phalanges or metacarpals can be classified according to the Swanson, Stabo and Anderson classification: type I (clean wound without significant contamination or delay in treatment), type II (contamination with gross dirt/debris, human or animal bite, lake/river injury, barnyard injury or in patients with significant systemic illness such as diabetes, hypertension, rheumatoid arthritis [RA], hepatitis, or asthma). Type I injuries can be treated with primary internal fixation and immediate wound closure. Although type II injuries can be treated with primary internal fixation (no increase in infection rate); these injuries should not be closed primarily. Delayed closure is preferred to decrease infection risk.
Any laceration overlying a joint in the hand, particularly the metacarpal-phalangeal (MCP) joint must be suspected as being caused by a human tooth. Also known as a “fight bite,” these injuries should be assumed to have been contaminated with oral flora and treated aggressively with broad spectrum antibiotics including anaerobic coverage. Animal bites require antibiotic treatment that covers Pasteurella and Eikenella.
Fractures of the metacarpal can be subclassified as follows: epiphyseal fractures, collateral ligament avulsion fractures, oblique, vertical, and horizontal head fractures, comminuted fractures, and fractures with joint loss. Most of these fractures require anatomic reduction to reestablish joint congruity and avoid posttraumatic arthritis. Stable reductions of fractures may be splinted in the intrinsic plus position. If unstable, percutaneous pinning, ORIF, or external fixation are options.
Metacarpal neck fractures are typically caused by direct trauma with volar comminution and dorsal apex angulation. The most common metacarpal neck fracture is the “boxer’s fracture” of the fifth metacarpal, usually caused by the fist striking a stationary object. These fractures can typically be closed reduced successfully. The degree of acceptable deformity varies according to the metacarpal injured: less than 10 degrees for the second and third metacarpal, less than 30-40 degrees for the fourth and fifth metacarpals. Unstable fractures require surgical intervention with percutaneous pinning or open reduction internal fixation.
Nondisplaced or minimally displaced metacarpal shaft fractures can be reduced and splinted. Surgical indications include rotational deformity (all fingers should point toward the scaphoid when flexed), dorsal angulation more than 10 degrees for second and third metacarpals, and more than 40 degrees for fourth and fifth metacarpals.
Fractures of the base of the second, third, and fourth metacarpals are typically minimally displaced and treated with splinting and early range of motion. A reverse Bennett fracture is a fracture dislocation of the fifth metacarpal and hamate bones. This injury often requires ORIF.
Fractures of the thumb metacarpal base can be extra-articular or intra-articular. Extra-articular fractures are usually transverse or oblique, and amenable to closed reduction and casting. Unstable fractures may require percutaneous pinning. Intra-articular fractures come in two types: type I or Benett’s Fracture where a single fracture line separates the majority of the metacarpal from the volar lip fragment and type II also known as Rolondo’s fracture which is a comminuted intra-articular fracture usually with a “Y” or “T” pattern including dorsal and palmar fragments. Both type I and type II fractures are treated with closed reduction and percutaneous pinning or ORIF.
Intra-articular fractures can be classified as condylar fractures or fracture-dislocations. There are three types of condylar fractures: unicondylar, bicondylar, or osteochondral. Each of these fractures require anatomic reduction; ORIF should be performed for more than 1 mm displacement. Comminuted intra-articular fractures not amenable to surgical treatment, can be treated closed with early protected mobilization.
Fracture dislocations come in two varieties: volar lip fracture or dorsal lip fracture. Volar lip fracture (dorsal fracture-dislocation) treatment is controversial; if less than 35% of the articular surface is involved the injury may be treated with buddy taping, however, for more than 35% some recommend ORIF or volar plate arthroplasty if the fracture is comminuted while others recommend extension block splint if the joint is not subluxed. Dorsal lip fracture (volar fracture-dislocation) with less than 1 mm of displacement may be treated closed with splinting while more than 1 mm displacement requires operative intervention.
Extra-articular fractures of the phalanges should be initially treated with closed reduction with finger-trap traction and splinting. Unstable fractures should be treated surgically.
Intra-articular dorsal lip fractures may be complicated by an extensor tendon disruption resulting in a “mallet finger.” “Mallet finger” may also result from purely tendinous disruption, without fracture. For either scenario, treatment is controversial. Some recommend full-time extension splinting for 6-8 weeks, while others recommend surgical intervention. For professionals who work extensively with their hands, such as surgeons, full-time extension splinting is not practical. Closed reduction with percutaneous pinning is a good option.
Intra-articular volar lip fractures can be associated with a flexor digitorum profundus rupture resulting in a “jersey finger” often seen in football or rugby players, most commonly involving the ring finger. Treatment is typically surgical, especially if large displaced bony fragments are present.
Extra-articular fractures can be transverse, longitudinal, or comminuted (nail matrix injury very common). These fractures are usually treated with closed reduction and splinting that traverses the DIP joint, leaving the PIP joint free. Surgery is indicated for fractures with wide irreducible displacement, due to the increased risk of nonunion.
Nailbed injuries are easily missed in the context of distal phalynx fractures. When untreated, these injuries result in nail growth disturbances. Subungual hematomas are often indicative of nail bed injury. The nail plate should be removed and the hematoma drained. Nailbed disruptions should be carefully sutured with 6-0 chromic catgut under magnification. The nailplate should be replaced to keep the nail fold open; alternatively a piece of aluminum foil or xeroform gauze can be used.
Carpometacarpal dislocations are usually high energy injuries. Careful neurovascular examination is essential. These injuries usually require surgical intervention for maintenance of a stable reduction.
MCP joint dislocations are usually dorsal in direction, presenting with a hyperextended posture. Simple dislocations can be reduced by flexion of the joint without traction. Wrist flexion, causing the flexor tendons to relax, can be used to facilitate the reduction maneuver. Complex MCP dislocations with the volar plate interposed in the joint are irreducible. The pathognomonic radiograph finding is the appearance of the sesamoid in the joint space. Complex dislocations require surgery. Traction during reduction of simple dislocations should be avoided as simple dislocations can be converted into complex ones. Volar dislocations are rare; however, because they are particularly unstable, they often require surgical intervention.
Thumb MCPs are unique due to the multiplanar motion of the thumb MCP joint. With a one-sided collateral ligament injury, the phalynx tends to sublux volarly rotating around the opposite intact ligament. The ulnar collateral ligament of the thumb MP joint is the most commonly injured ligament in the digits. If the injury is acute, it is called a “skier’s thumb,” whereas chronic injury from repetitive trauma is known as a “gamekeeper’s thumb.” Nonoperative treatment with reduction and thumb spica splinting or casting is usually sufficient. A “Stener” lesion occurs when the ulnar collateral ligament avulses, and comes to rest dorsal to the adductor aponeurosis. The ulnar collateral ligament is not able to return to its normal insertion, preventing healing. As a result, Stener lesions and irreducible MCP dislocations require surgical intervention.
Proximal interphalangeal (PIP) joint dislocations include dorsal dislocation, pure volar dislocation, and rotatory volar dislocation. Once reduced, rotatory volar dislocations, collateral ligament ruptures, and dorsal dislocations congruent in full extension on the lateral radiographs can all begin active range of motion exercises immediately with adjacent digit strapping. Dorsal dislocations that continue to sublux on lateral radiograph, can be treated with a few weeks of extension block splinting. Volar dislocations with central slip disruptions are treated with 4-6 weeks of PIP extension splinting, followed by an additional 2 weeks of night-time splinting. Irreducible dislocations or unstable reductions may require surgical intervention.
Distal interphalangeal (DIP) dislocations and thumb IP joint dislocations can present late. Injuries are considered chronic after 3 weeks. Acute reduced dislocations may begin immediate active range of motion. Unstable dislocations should be immobilized in 30 degrees of flexion for 3 weeks. Complete collateral ligament injury should be protected from lateral stress for at least 4 weeks. Recurrent stability can be treated with Kirschner wire fixation. Chronic dislocation may be treated with open reduction to resect scar tissue, allowing for a tension free reduction. Transverse open wounds in the volar skin crease are not infrequent. Open dislocations require debridement to prevent infection.
Hip dislocations of the native hip are relatively rare, usually due to high energy injury such as a motor vehicle accident. Posterior hip dislocations (85%-90%) are more common than anterior (remaining 10%-15%). Ten to twenty percent of posterior hip dislocations can be complicated by sciatic nerve injury. Anterior hip dislocations are associated with a greater incidence of femoral head injury. Up to 50% of patients with a hip dislocation will sustain a concomitant fracture elsewhere (most commonly of the ipsilateral femur or pelvis).
The hip articulation is a ball-and-socket joint, formed by the femoral head and acetabulum. Forty percent of the femoral head is covered by the acetabulum. The labrum surrounding the acetabulum has the effect of deepening the hip joint, increasing its stability. The medial and lateral circumflex femoral arteries from the profunda femoral artery form an extracapsular vascular ring at the base of the femoral neck; ascending branches provide the primary blood supply to the femoral neck and head, along with a minor contribution from the ligamentum teres off of the obturator artery. The contribution of the medial and lateral circumflex arteries is often disrupted with hip dislocation, leading to long-term complications including avascular necrosis. The sciatic nerve exits the pelvis at the greater sciatic notch, traveling deep to the piriformis muscle, down the posterior aspect of the thigh.
A full trauma survey is essential due to the high energy nature of this injury. Patients typically present with severe discomfort and inability to move the injured extremity. The classic appearance of a posterior hip dislocation is shortened extremity with the hip flexed, internally rotated and adducted (Figure 40–13). Patients with an anterior dislocation hold their hip with marked external rotation, mild flexion, and abduction. Careful neurovascular examination is key. If the sciatic nerve is injured often the tibial nerve is preserved with the peroneal portion of the nerve showing the effects of injury. Radiographic evaluation includes an AP view of the pelvis as well as radiographs of the entire ipsilateral femur. Evaluate the femoral neck and acetabulum to rule-out concomitant fractures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree