Open Cholecystectomy
Sean P. Montgomery
Preston B. Rich
DEFINITION
Removal of the gallbladder for benign disease using an open technique when the laparoscopic technique is not prudent.
DIFFERENTIAL DIAGNOSIS
Acute cholecystitis
Symptomatic biliary colic
Acalculous cholecystitis
Diseases that can present similarly and are not treatable by simple cholecystectomy include peptic ulcer disease, hepatitis, pancreatitis, cholangitis, gallbladder cancer, colitis, irritable bowel syndrome, and atypical appendicitis.
PATIENT HISTORY AND PHYSICAL FINDINGS
Biliary colic (symptomatic cholelithiasis) is typically a right upper quadrant (RUQ) or epigastric postprandial pain. Symptoms classically start 30 to 90 minutes after eating and association with high-fat meals may be described. Nausea and bloating are common. The pain typically will resolve within 6 hours. Pain lasting more than 6 hours and/or fever is suggestive of acute cholecystitis.
On physical examination, tenderness will usually be present in the RUQ. The presence of a Murphy’s sign (inspiratory arrest with RUQ palpation) is suggestive of acute cholecystitis.
IMAGING AND OTHER DIAGNOSTIC STUDIES
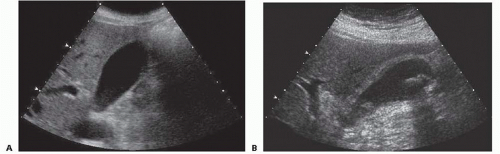
A fasting RUQ ultrasound is the “gold standard” for the diagnosis of gallstones and is frequently the only imaging necessary to diagnose acute cholecystitis. Gallstones are identified as mobile echogenic foci with posterior shadowing (FIG 1). Cholecystitis is suggested by gallbladder wall thickening (>3 mm), pericholecystic fluid, or inspiratory arrest elicited by placement of the ultrasound probe directly over the gallbladder (a sonographic Murphy’s sign). The sensitivity and specificity of ultrasound for calculous cholecystitis are around 82%.1 In critically ill patients with acalculous cholecystitis, the specificity drops significantly.
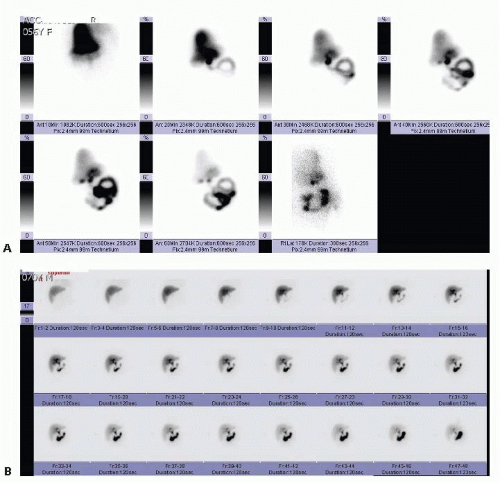
The other common imaging study used to diagnose gallbladder pathology is a nuclear medicine test called either hepatobiliary scintigraphy or a hepatobiliary iminodiacetic acid (HIDA) scan (commonly referred to as a HIDA scan.) In this test, a radiolabeled substrate is intravenously administered, taken up by the liver, and excreted into the biliary tree (FIG 2). If the substrate fails to fill the gallbladder within 1 hour, the sensitivity is 96% for acute cholecystitis.1 A HIDA scan will also provide information about obstruction of the common bile duct, as substrate will be seen accumulating in the duodenum if the duct is not obstructed. In the setting of hepatic failure or cholestasis, this study is not useful, as the liver often will not take up enough substrate to allow an adequate study. Gallstones are not revealed with this study, but rather, the presence or absence of cholecystitis is determined by assessing patency of the cystic duct regardless of the etiology. HIDA scintigraphy is generally performed if the clinical findings and ultrasound are inconclusive for calculous cholecystitis or in critically ill patients with suspected acalculous cholecystitis.2
SURGICAL MANAGEMENT
Preoperative Planning
The vast majority of patients will be appropriate candidates for a laparoscopic cholecystectomy. Conversion from laparoscopy due to variable anatomy or severe inflammation is the most common indication for the open procedure. Rare patients in whom a primary open cholecystectomy should be considered are the following:
Septic patients on vasoactive agents for hemodynamic support that have failed percutaneous drainage
Patients with complicated anterior abdominal walls and/or severe adhesions. Specifically, if there are large pieces
of prosthetic mesh in the umbilical and epigastric areas and/or prior RUQ surgery, laparoscopic completion of a cholecystectomy can be challenging.
The need for concomitant open common bile duct exploration
Positioning
The patient is positioned supine. Arms can be tucked by the side or extended out at right angles to the bed. An oral or nasal tube for gastric decompression is placed.
TECHNIQUES
INCISION
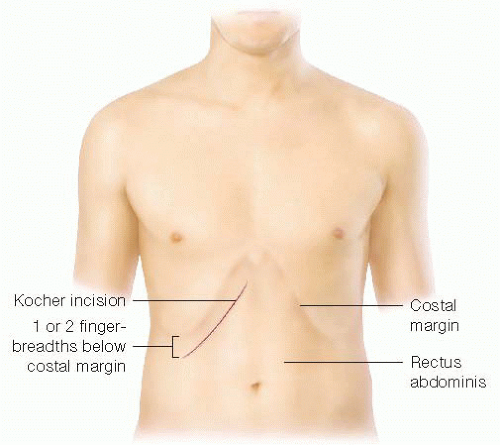
The gallbladder is most easily accessed through an oblique RUQ incision (FIG 3). The incision should be placed two fingerbreadths below the right costal margin to facilitate fascial closure. In patients with significant hepatomegaly, the incision may be moved inferiorly to two fingerbreadths below the palpable liver edge, but this should rarely be necessary. The incision is carried down to the fascia.
OPENING OF THE ABDOMINAL WALL
The anterior rectus fascia should be incised with electrocautery. A Kelly or other large clamp is placed under the lateral border of the rectus muscle, retracting it anteriorly, to facilitate division of the muscle with electrocautery. The superior epigastric vessels can be encountered, typically about halfway across the rectus. The vessels can be ligated or cauterized, or they can be reflected medially and preserved with the medial half of the rectus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree