2. Patients not expected to resume adequate oral feedings within 7 to 10 days of surgery should begin nutritional support within 2 to 4 days postoperatively, within 1 to 2 days if they are in an intensive care unit.
III. Enteral nutrition is almost always preferred over parenteral nutrition. Goals include meeting and attenuating the metabolic response to stress, and in addition attenuating cellular injury, and modulating the immune response to injury. A variety of enteral solutions containing various amounts of protein (amino acids), carbohydrates (glucose), fat (medium and long chain triglycerides), micronutrients, macronutrients, and electrolytes are available.
A. Enteral tube feeding may be necessary when patients are unable to consume nutritionally complete, liquefied food orally. Most often, patients receive continuous infusions of enteral nutrition through a nasoenteric tube positioned in the stomach, duodenum, or jejunum. Surgical placement of an esophagostomy or gastrostomy tube may be indicated for long-term feeding. The rate of infusion is typically 100 to 120 mL per hour (slow rate of infusion prevents the dumping syndrome).
B. Side Effects
1. Enteral feeding is frequently stopped because of patient’s complaints (bloating or distention, emesis, high gastric residuals [usually 200 to 250 mL]). Osmotic diarrhea in this situation is a diagnosis of exclusion (Clostridia difficile). If clinically indicated, serum electrolyte levels should be measured to identify excessive loss or signs of dehydration.
2. Pulmonary aspiration is always a danger when enteral tube feeding is used. Patients should be maintained in a semi-sitting position (head of bed elevated 30 degrees) and in patients at the highest risk of aspiration, the feeding tube should be placed through the pylorus.
IV. Parenteral nutrition is indicated for patients who are unable to ingest or digest nutrients or to absorb them from the gastrointestinal tract. Parenteral nutrition using isotonic solutions delivered through a peripheral vein is acceptable when the patient requires less than 2,000 calories daily and the anticipated need for nutritional support is brief. When nutritional requirements are greater than 2,000 calories daily or prolonged nutritional support is required, a catheter is placed in the central venous system to permit infusion of a hypertonic (1,900 mOsm/L) nutrition solution.
A. Short-term parenteral therapy (3 to 5 days in patients without nutritional deficits) after uncomplicated surgical procedures is most often provided by hypocaloric, non-nitrogen glucose-electrolyte solutions.
B. Long-term (total) parenteral nutrition (IV hyperalimentation) is the technique of providing total nutrition needs by infusion of amino acids combined with glucose and varying amounts of lipids. These hypertonic solutions must be infused into a central vein with a high blood flow to provide rapid dilution. Because the solutions in current use are not nearly as hypertonic and hypercaloric as they once were, there is little concern about the patient becoming hypoglycemic if the infusion is discontinued abruptly but should be considered. Serum electrolytes, blood glucose concentrations, and blood urea nitrogen should be measured periodically during total parenteral nutrition. Tests of hepatic and renal function are also recommended but can be performed at less frequent intervals.
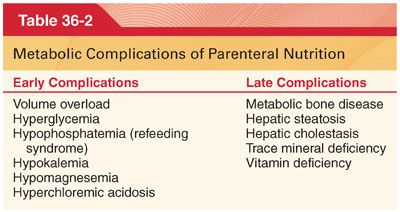
1. Side effects of total parenteral nutrition include infectious (catheter sepsis), mechanical (pneumothorax, catheter thrombosis), and metabolic complications (Table 36-2).
a. Sepsis. Total parenteral nutrition solutions infused through an IV catheter can support the growth of bacteria and fungi (spiking temperature most likely reflects contamination via the delivery system or catheter). In view of the hazard of contamination, the use of a central venous hyperalimentation catheter for administration of medications, as during the perioperative period, or for sampling of blood is not recommended.
b. Hyperglycemia. Blood glucose concentrations should be monitored until glucose tolerance is demonstrated, which usually occurs after 2 to 3 days of therapy as endogenous insulin production increases. Current guidelines suggest a target blood glucose concentration of 140 to 200 mg/dL and avoidance of targets below 140 mg/dL.
c. Hypoglycemia. Accidental, sudden discontinuation of the infusion of total parenteral nutrition solutions containing large amounts of glucose (catheter kink or disconnection) may cause hypoglycemia.
d. Metabolic acidosis may occur because most of the amino acids in TPN are administered as their chloride salts.
e. Hypercarbia. In a patient with inadequate respiratory reserve, respiratory failure can develop with aggressive nutritional support that increases carbon dioxide production.
2. Monitoring during Total Parenteral Nutrition. Access sites are observed for signs of infection. Substitution of sodium or potassium acetate (metabolized to bicarbonate) for sodium or potassium chloride may be helpful should signs of hyperchloremic metabolic acidosis appear. Vitamin K may need to be added to the TPN or administered intravenously based on measurement of prothrombin and plasma thromboplastin times.
V. Immunonutrition. Cellular immunity decreases during acute stress as may accompany multiple organ system failure, sepsis, and shock. Immunonutrition is an attempt to enhance immunity and cellular integrity by incorporating specific additives (omega-3 fatty acids, arginine to enhance lymphocyte cytotoxicity, purines as a precursor of RNA and DNA, and antioxidants) into enteral diets.
VI. Vitamins, Dietary Supplements, and Herbal Remedies
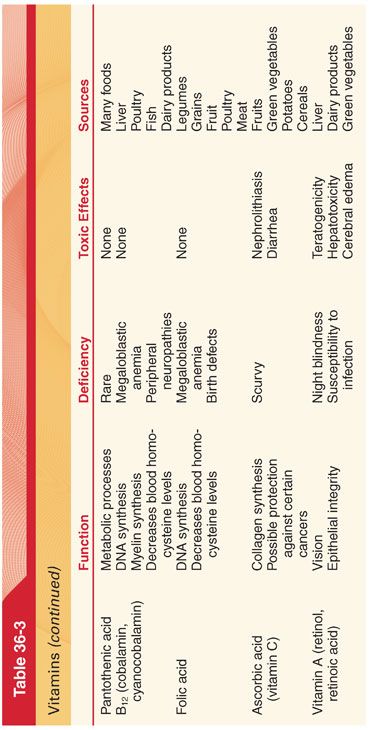
A. Vitamins are a group of structurally diverse organic substances (water soluble or fat soluble) that must be provided in small amounts in the diet for subsequent synthesis of cofactors that are essential for various metabolic reactions (Table 36-3).
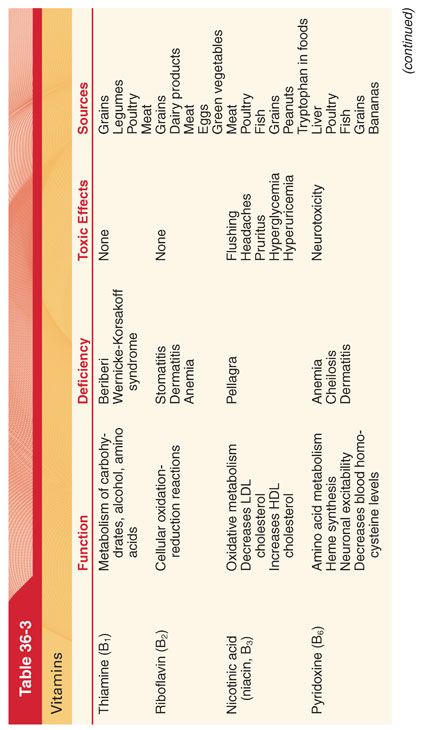
B. Water-Soluble Vitamins (Fig. 36-1)
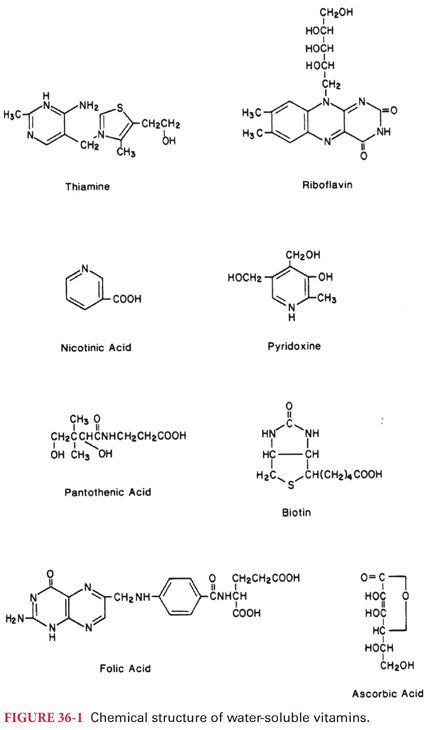
1. Thiamine (vitamin B1) is converted to a physiologically active coenzyme that is essential for the decarboxylation of α-keto acids such as pyruvate (increased plasma concentrations of pyruvate are a diagnostic sign of thiamine deficiency).
a. Causes of Deficiency. The requirement for thiamine is related to the metabolic rate and is greatest when carbohydrate is the source of energy (important in patients maintained by hyperalimentation in which the majority of calories are provided in the form of glucose).
b. Symptoms of deficiency (beriberi) include loss of appetite, skeletal muscle weakness, a tendency to develop peripheral edema, decreased systemic blood pressure, and low body temperature. Severe thiamine deficiency (Korsakoff syndrome), which may occur in alcoholics, is associated with peripheral polyneuritis. High-output cardiac failure with extensive peripheral edema reflecting hypoproteinemia is often prominent.
c. Treatment of Deficiency. Severe thiamine deficiency is treated with IV administration of the vitamin.
2. Riboflavin (vitamin B2). Riboflavin is converted in the body to one of two physiologically active coenzymes that primarily influence hydrogen ion transport in oxidative enzyme systems. Pharyngitis and angular stomatitis are typically the first signs of riboflavin deficiency. Treatment is with oral vitamin supplements that contain riboflavin.
3. Nicotinic acid (niacin, B3) is converted to the physiologically active coenzymes that are necessary to catalyze oxidation-reduction reactions essential for tissue respiration.
a. Symptoms of Deficiency. Chronic niacin deficiency is manifested by pellagra (tongue becomes red and swollen). In addition to dementia, motor and sensory disturbances of the peripheral nerves also occur, mimicking changes that accompany a deficiency of thiamine.
b. The relationship between nicotinic acid requirements and the intake of tryptophan explains the association of pellagra with tryptophan-deficient corn diets. Carcinoid syndrome is associated with diversion of tryptophan from the synthesis of nicotinic acid to the production of serotonin (5-hydroxytryptamine), leading to symptoms of pellagra. Isoniazid inhibits incorporation of nicotinic acid into nicotinamide adenine dinucleotide and may produce pellagra. Pellagra is uncommon in the United States, reflecting the supplementation of flour with nicotinic acid.
4. Pyridoxine (vitamin B6) is converted to pyridoxal phosphate that serves an important role in metabolism as a coenzyme for the conversion of tryptophan to serotonin and methionine to cysteine.
a. Symptoms of Deficiency. Pyridoxine deficiency is uncommon, and when present is associated with deficiencies of other vitamins, and if seen is more likely to be seen in the elderly, patients with alcoholism, and in patients who are severely malnourished.
b. Drug Interactions. Isoniazid and hydralazine act as potent inhibitors of pyridoxal kinase, thus preventing synthesis of the active coenzyme form of the vitamin (administration of pyridoxine decreases the incidence of neurologic side effects associated with the administration of these drugs).
5. Pantothenic acid is converted to coenzyme A, which serves as a cofactor for enzyme-catalyzed reactions that are important in the oxidative metabolism of carbohydrates, gluconeogenesis, and the synthesis and degradation of fatty acids. Pantothenic acid deficiency in humans is rare, reflecting the ubiquitous presence of this vitamin in ordinary foods as well as its production by intestinal bacteria.
6. Biotin functions as a coenzyme for enzyme-catalyzed carboxylation reactions and fatty acid synthesis. Seborrheic dermatitis of infancy is most likely a form of biotin deficiency.
7. Cyanocobalamin (cobalamin, vitamin B12) is a generic designation to describe several cobalt-containing compounds (cobalamins). Dietary vitamin B12 in the presence of hydrogen ions in the stomach is released from proteins.
a. Causes of Deficiency. Gastric achlorhydria and decreased gastric secretion of intrinsic factor are the most likely causes of vitamin B12 deficiency in adults. Surgical resection or disease of the ileum predictably interferes with the absorption of vitamin B12. Nitrous oxide irreversibly oxidizes the cobalt atom of vitamin B12 such that the activity of two vitamin B12–dependent enzymes, methionine synthetase and thymidylate synthetase, are decreased.
b. Diagnosis of Deficiency. The plasma concentration of vitamin B12 (cobalamin) is less than 200 pg/mL when there is a deficiency state. Measurements of gastric acidity may provide indirect evidence of a defect in gastric parietal cell function, whereas the Schilling test (radioactivity in the urine measured after oral administration of labeled vitamin B12) can be used to quantitate ileal absorption of vitamin B12.
c. Symptoms of Deficiency. Deficiency of vitamin B12 results in defective synthesis of DNA (symptoms of vitamin B12 deficiency manifest most often in the hematopoietic and nervous systems). Clinically, the earliest sign of vitamin B12 deficiency is megaloblastic (pernicious) anemia (may be so severe that cardiac failure occurs). Encephalopathy is a well-recognized complication of vitamin B12 deficiency manifesting as myelopathy, optic neuropathy, and peripheral neuropathy, either alone or in any combination. Folic acid therapy corrects the hematopoietic, but not nervous system, effects produced by vitamin B12 deficiency.
d. Treatment of Deficiency. In the patient with neurologic changes, leukopenia, or thrombocytopenia, treatment must be aggressive with intramuscular administration of vitamin B12 and oral administration of folic acid. Neurologic damage after pernicious anemia develops that is not reversed after 12 to 18 months of therapy is likely to be permanent.
8. Folic acid is transported and stored as 5-methylhydrofolate after absorption from the small intestine. Conversion to the metabolically active form, tetrahydrofolate, is dependent on the activity of vitamin B12. Virtually all foods contain folic acid, but protracted cooking can destroy up to 90% of the vitamin.
a. Causes of Deficiency. Alcoholism is the most common cause of folic acid deficiency, with decreases in the plasma concentrations of folic acid manifesting within 24 to 48 hours of continuous alcohol ingestion. Drugs that inhibit dihydrofolate reductase (methotrexate, trimethoprim) or interfere with absorption and storage of folic acid in tissues (phenytoin) may cause folic acid deficiency.
b. Symptoms of Deficiency. Megaloblastic anemia is the most common manifestation of folic acid deficiency. This anemia cannot be distinguished from that caused by a deficiency of vitamin B12 but is confirmed by the presence of a folic acid concentration in the plasma of less than 4 ng/mL.
c. Treatment of Deficiency. Folic acid is available as an oral preparation alone or in combination with other vitamins and either an oral preparation or as a parenteral injection. In the presence of megaloblastic anemia because of folic acid deficiency, the administration of the vitamin is associated with a decrease in the plasma concentration of iron within 48 hours, reflecting new erythropoiesis.
d. Leucovorin (citrovorum factor) is a metabolically active, reduced form of folic acid. After treatment with folic acid antagonists, such as methotrexate, patients may receive leucovorin (rescue therapy), which serves as a source of tetrahydrofolate that cannot be formed due to drug-induced inhibition of dihydrofolate reductase.
9. Ascorbic Acid (Vitamin C). Ascorbic acid acts as a coenzyme and is important in a number of biochemical reactions, mostly involving oxidation (synthesis of collagen, carnitine, and corticosteroids). Despite contrary claims, controlled studies do not support the efficacy of even large doses of ascorbic acid in treating viral respiratory tract infections. A risk of large doses of ascorbic acid is the formation of kidney stones resulting from the excessive secretion of oxalate.
a. Symptoms of Deficiency. Humans, in contrast to many other mammals, are unable to synthesize ascorbic acid, emphasizing the need for dietary sources of the vitamin to prevent scurvy (gingivitis, rupture of the capillaries with formation of numerous petechiae, failure of wounds to heal). Scurvy is encountered among the elderly, alcoholics, and drug addicts. Patients receiving TPN should receive supplemental ascorbic acid.
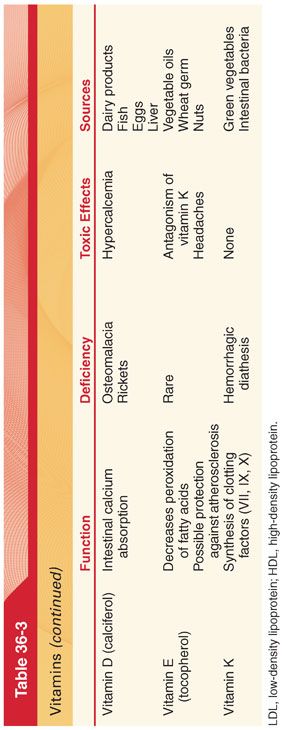
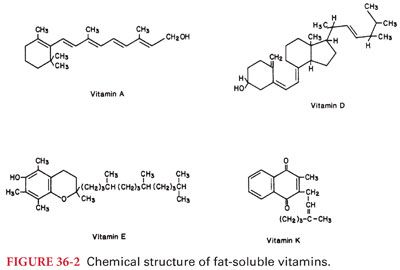
C. Fat-soluble vitamins (A, D, E, and K) are absorbed from the gastrointestinal tract and any condition that causes malabsorption of fat, such as obstructive jaundice, may result in deficiency of one or all these vitamins (Fig. 36-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


