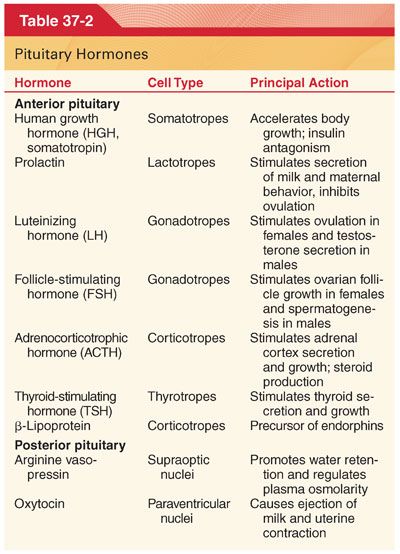
A. Anterior Pituitary (see Table 37-2)
1. Growth hormone (somatotropin; GH) stimulates growth of all tissues in the body (linear bone growth) and evokes intense metabolic effects (protein synthesis, mobilization of fatty acids, antagonism of insulin action, sodium and water retention; Fig. 37-1).
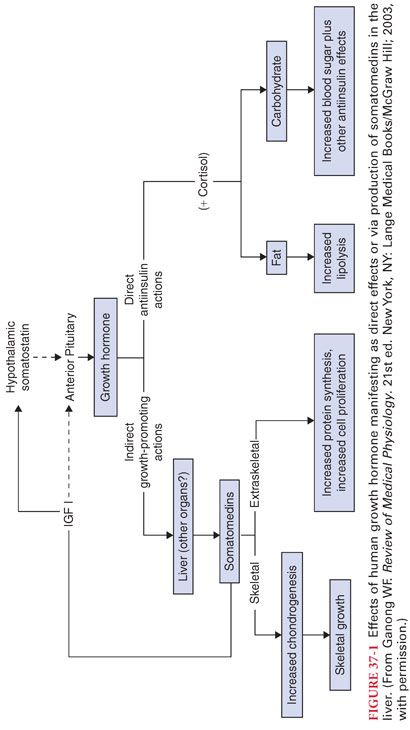
a. Releasing (GH-releasing hormone) and inhibitory (somatostatin) hormones, physiologic events (perioperative anxiety), and medications regulate GH secretion (Table 37-3).
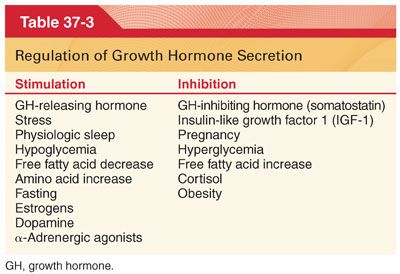
b. Large doses of corticosteroids suppress secretion of GH (inhibitory effects on growth observed in children receiving high doses of corticosteroids).
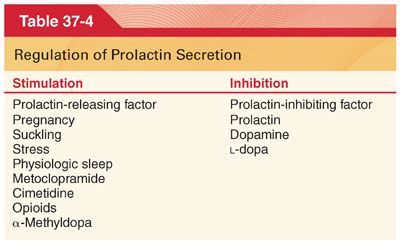
2. Prolactin promotes the growth and development of the breast in preparation for breast-feeding (Table 37-4). Preoperative anxiety also increases plasma concentrations of prolactin.
3. Gonadotropins (luteinizing hormone and follicle-stimulating hormone) are responsible for pubertal maturation and secretion of steroid sex hormones by the gonads of either sex.
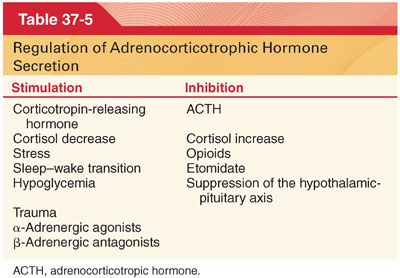
4. Adrenocorticotrophic hormone (ACTH) regulates secretions of the adrenal cortex, especially cortisol. Secretion of ACTH responds dramatically to stress under the control of corticotropin-releasing hormone from the hypothalamus, as well as a negative feedback mechanism from the circulating plasma concentration of cortisol (Table 37-5).
a. In the absence of ACTH, the adrenal cortex undergoes atrophy, but the zona glomerulosa, which secretes aldosterone, is least affected (hypophysectomy has minimal effects on electrolyte balance because of the continued release of aldosterone from the adrenal cortex).
b. Chronic administration of corticosteroids suppresses corticotropin-releasing hormone and leads to atrophy the hypothalamic-pituitary axis. Several months may be required for recovery of this axis after removal of the suppressive influence. In such patients, stressful events during the perioperative period might evoke life-threatening hypotension.
c. It is a common practice to administer supplemental exogenous corticosteroids (based on the magnitude of stress) to patients considered at risk for suppression of the hypothalamic-pituitary axis (little evidence, however, that supplemental corticosteroids in excess of normal daily physiologic secretion are necessary or beneficial intra- or postoperatively).
5. Thyroid-stimulating hormone (TSH) accelerates all the steps in the formation of thyroid hormones and causes proteolysis of thyroglobulin in the follicles of thyroid cells to release thyroid hormones into the circulation.
a. Secretion of TSH from the anterior pituitary is under the control of thyrotropin-releasing hormone from the hypothalamus as well as a negative feedback mechanism, depending on the concentrations of thyroid hormones circulating in plasma.
b. Hypothyroidism with increased plasma concentrations of TSH indicates a primary defect at the thyroid gland (primary hypothyroidism) and an attempt by the anterior pituitary to stimulate hormonal output by releasing TSH.
c. A defect at the hypothalamus or anterior pituitary is indicated by low concentrations of both TSH and thyroid hormones circulating in plasma (secondary hypothyroidism).
B. Posterior Pituitary. Arginine vasopressin (AVP) and oxytocin are transported in secretory granules along axons from corresponding nuclei in the hypothalamus to the posterior pituitary for subsequent release in response to appropriate stimuli.
1. Arginine Vasopressin. The physiologic functions of AVP include vasoconstriction, water retention, and corticotropin secretion. Decreases in blood volume, increased plasma osmolality, and decreased arterial pressure stimulate AVP release (Table 37-6).
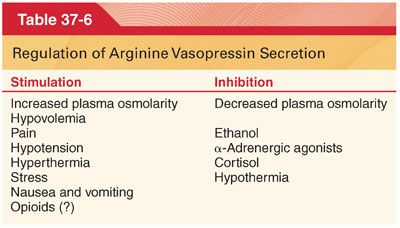
a. Administration of morphine, or other opioids, in the absence of painful stimulation does not evoke the release of AVP.
b. Decreases in urine output and fluid retention previously attributed to release of AVP during positive pressure ventilation of the lungs are more likely the result of changes in cardiac filling pressures that impair the release of atrial natriuretic hormone.
c. Destruction of neurons in or near the supraoptic and paraventricular nuclei of the hypothalamus from pituitary surgery, trauma, cerebral ischemia, or malignancy may decrease vasopressin release to cause central diabetes insipidus (diabetes insipidus from lack of vasopressin release during pituitary surgery is usually transient).
d. Unnecessary or excessive secretion of AVP with subsequent retention of water and dilutional hyponatremia may result from head injuries, intracranial tumors, meningitis, or pulmonary infections.
2. Oxytocin. Breast suckling and cervical and vaginal dilation stimulate oxytocin secretion. Large amounts of oxytocin cause sustained uterine contraction as necessary for postpartum hemostasis. Oxytocin has only 0.5% to 1.0% the antidiuretic activity of AVP and can be released abruptly and independently of AVP.
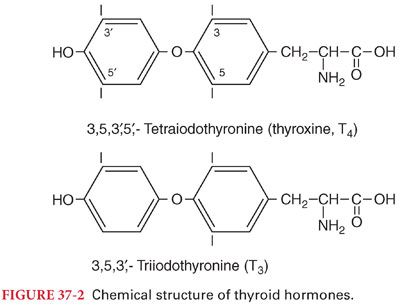
IV. Thyroid Gland. The thyroid gland maintains optimal metabolism for normal tissue function. The principal hormonal secretions of the thyroid gland are thyroxine (T4) and triiodothyronine (T3) (Fig. 37-2). In addition to thyroid hormones, the thyroid gland secretes calcitonin, which is important for calcium ion use. The thyroid hormones increase oxygen consumption in nearly all tissues, except for the brain (consistent with the minimal changes in anesthetic requirements [MAC]) that accompany hyperthyroidism or hypothyroidism. Cardiovascular changes are often the earliest clinical manifestations of abnormal thyroid hormone levels. Thyroid hormones are stored in combination with thyroglobulin. Stimulation of proteases by TSH results in cleavage of hormones from thyroglobulin and their release into the systemic circulation.
A. Mechanism of Action
1. When thyroid hormones enter cells, T3 binds to nuclear receptors. T4 also binds to these receptors but not as avidly and rather serves principally as a prohormone for T3.
2. Sympathomimetic effects that accompany thyroid hormone stimulation most likely reflect a greater number and sensitivity of β-adrenergic receptors to release of T4 and T3. When thyroid hormones accelerate metabolism, tissues vasodilate and blood flow delivers necessary oxygen and carries away metabolites and heat. As a result, cardiac output often increases but systemic blood pressure is unchanged because peripheral vasodilation offsets the impact of more blood flow.
3. Excess protein catabolism associated with greater secretion of thyroid hormones is the mechanism behind skeletal muscle weakness characteristic of hyperthyroidism.
4. The fine muscle tremor that accompanies hyperthyroidism stems from the sensitivity of neuronal synapses in the area of the spinal cord that controls skeletal muscle tone.
B. Calcitonin
1. Is a polypeptide hormone secreted by the thyroid gland that decreases the concentration of calcium ions in plasma by weakening the activity of osteoclasts and strengthening the activity of osteoblasts.
2. A total thyroidectomy and subsequent absence of calcitonin does not measurably influence the plasma concentration of calcium because of the predominance of parathyroid hormone.
V. Parathyroid Glands
A. The four parathyroid glands secrete parathyroid hormone (PTH) that regulates plasma concentration of calcium ions. Secretion of PTH is inversely related to plasma ionized calcium concentration. Small declines in the plasma concentration of calcium ions stimulate the release of PTH.
B. PTH exerts its effect on target cells in bones, renal tubules, and the gastrointestinal tract by stimulating the formation of cyclic adenosine monophosphate (cAMP). Because a portion of cAMP synthesized in the kidneys escapes into the urine, its assay serves as a measure of parathyroid gland activity.
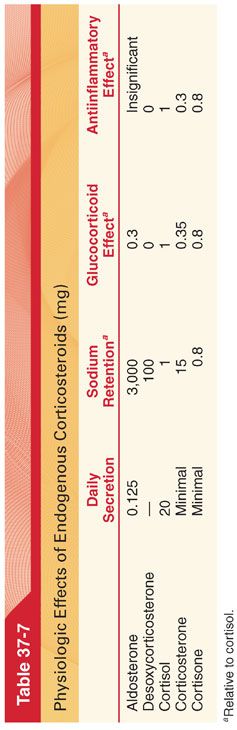
VI. Adrenal Cortex. The adrenal cortex secretes three major classes of corticosteroids: mineralocorticoids, glucocorticoids, and androgens. More than 30 different corticosteroids have been isolated from the adrenal cortex, but only two are important: aldosterone, a mineralocorticoid, and cortisol, the principal glucocorticoid (Table 37-7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


