Nodal Marginal Zone B-cell Lymphoma
Pei Lin, MD
Key Facts
Clinical Issues
Age: 5th-6th decades
No evidence of extranodal or splenic lymphoma
Can transform to diffuse large B-cell lymphoma
Microscopic Pathology
Expanded marginal zones or replacement of lymph node by small cells with scattered large cells
Small cells can be centrocyte-like or monocytoid
Lymphoplasmacytoid or mature-appearing plasma cells can be prominent
Residual reactive follicles with hyperplastic germinal centers
Ancillary Tests
Positive for monotypic Ig (bright) and B-cell markers
In paraffin sections, only plasmacytoid cells express cytoplasmic Ig
Aberrantly express CD43 in ˜ 50% of cases
Usually negative for CD5, CD10, and CD23
Top Differential Diagnoses
MALT lymphoma secondarily involving lymph node
Lymphoplasmacytic lymphoma
Mantle cell lymphoma
CLL/SLL with plasmacytoid differentiation
Peripheral T-cell lymphoma
Diagnostic Checklist
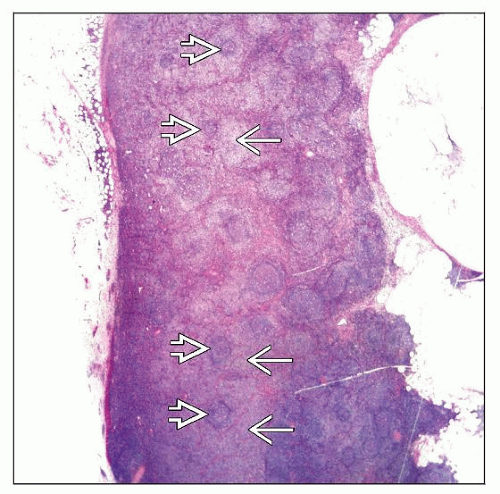
Often pale appearance at low-power magnification
Residual germinal centers surrounded by centrocyte-like and monocytoid cells
Scattered large cells present
TERMINOLOGY
Abbreviations
Nodal marginal zone B-cell lymphoma (NMZL)
Synonyms
Nodal marginal zone lymphoma
Monocytoid B-cell lymphoma
Parafollicular B-cell lymphoma
NMZL can be placed in any of 3 categories depending on large cell number (Working Formulation [1982])
Small lymphocytic plasmacytoid, diffuse small cleaved cell, or diffuse mixed small and large cell
Definitions
Primary nodal B-cell lymphoma histologically resembling lymph nodes involved by MZL of extranodal or splenic types
There can be no evidence of extranodal or splenic disease
CLINICAL ISSUES
Epidemiology
Incidence
Low, ˜ 2% of all non-Hodgkin lymphomas
Age
5th-6th decades
Median age around 60 years
Can occur in children
Gender
Female predominance
Presentation
Lymphadenopathy, localized or widespread
Systemic (B) symptoms in 1/3 of patients
In patients with localized disease, head and neck region is most often affected
Bone marrow involvement common (30-60% of patients in various studies)
Leukemic involvement (elevated WBC) is uncommon
Association with hepatitis C infection in Italy
Prognosis
Clinically indolent
> 60% of patients have overall survival > 5 years
Affected children have excellent long-term survival
Patients can undergo transformation to diffuse large B-cell lymphoma
Prognosis substantially worse
MICROSCOPIC PATHOLOGY
Histologic Features
Lymph nodes can be partially or completely effaced by lymphoma
Marginal zones expanded in cases with partial involvement
Neoplasm has diffuse pattern in completely replaced lymph nodes
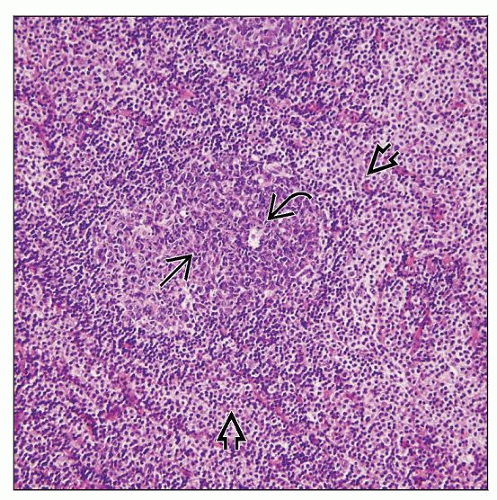
Cytologically, predominant cell type is small with variably irregular nuclear contours
Lymphoma cells commonly have abundant pale cytoplasm (so-called monocytoid features)
Lymphoid cells with plasmacytoid differentiation or plasma cells are common and can be numerous
Large cells are always present in varying numbers; can be numerous
Residual reactive follicles with hyperplastic germinal centers are common
Germinal centers often have numerous tingible body macrophages
Reactive follicles can be colonized by lymphoma (mimicking follicular lymphoma)
Bone marrow shows paratrabecular and nonparatrabecular pattern of involvement
Lymphoma aggregates often associated with follicular dendritic cells, CD21(+)
Predominant Pattern/Injury Type
Lymphoid, marginal zone
Predominant Cell/Compartment Type
Centrocyte-like or monocytoid cells, lymphoplasmacytoid cells or plasma cells
ANCILLARY TESTS
Immunohistochemistry
Neoplastic plasmacytoid lymphocytes and plasma cells express monotypic cytoplasmic Ig light chain
Aberrant expression of CD43 is common (˜ 50%)
Positive for pan-B-cell antigens (e.g., CD19, CD20, pax-5)
Bcl-2(+), CD10(-), Bcl-6(-), Cyclin-D1(-)
Usually negative for CD5 and CD23
Flow Cytometry
Usually express monotypic surface Ig
Brightly positive for pan-B-cell antigens (CD19, CD20, CD22) and negative for CD10
Negative for T-cell antigens (CD2, CD3, CD5, CD7, TCR-β)
CD43 is commonly expressed
Subset of cases can be CD23(+)
Rare cases can be CD5(+)
Cytogenetics
No consistent translocations identified
Trisomies of 3, 7, and 18 in subset of cases
PCR
Ig gene rearrangements are present
Ig genes are commonly mutated
May result in false-negative PCR results
No evidence of BCL1/IgH or IgH/BCL2 translocations
DIFFERENTIAL DIAGNOSIS
Extranodal Marginal Zone B-cell Lymphoma of Mucosa-associated Lymphoid Tissue (MALT Lymphoma)
Can be associated with autoimmune diseases
Involves extranodal sites: GI tract, lung, salivary glands, orbit, skin
Stomach most common site
Cytologically, can closely resemble NMZL
Chromosomal translocations are reported in subset of MALT lymphomas
t(11;18)(q21;q21)/API2-MALT1
t(14;18)(q32;q21)/MALT1-IgH
T(3;14)(p14.1;q32)/FOXP1-IgH
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree