Neurosurgical and Neurological Emergencies for Surgeons
Ekkehard Kasper
Clark Chen
Burkhard Kasper
Traumatic and Nontraumatic Head and Brain Injury
Traumatic Brain Injury: Blunt Versus Penetrating Trauma
Epidemiology of Traumatic Brain Injury
Before we commit ourselves to reviewing the management of traumatic brain injury (TBI), we need to understand that this problem remains a major public health issue in our times. To illustrate this point, I want to reiterate some facts about TBI in the United States as an introduction to the topic as reported by the Brain Trauma Foundation (www.BTF.org):
Brain injuries are most often caused by motor vehicle crashes, assaults, sports injuries, or even simple falls on the playground, at work, or in the home. An estimated 1.5 million moderate to severe head injuries occur every year in the United States and an additional estimated 1.6 million to 3.8 million sports-related TBIs occur each year. Every year, <52,000 deaths occur from TBI and it is the leading cause of death and disability in children and adults from ages 1 to 44 years. At least 5.3 million Americans, that is, 2% of the U.S. population currently live with disabilities resulting from TBI. In addition, moderate and severe head injuries are associated with an increased risk of developing Alzheimer’s disease.
Males are about twice as likely as females to experience this and hospitalization rates have increased from 79 per 100,000 in 2002 to 87.9 per 100,000 in 2003. Blasts are a leading cause of TBI among active-duty military personnel in war zones and veterans’ advocates believe that between 10% and 20% of Iraq veterans, or 150,000 and 300,000 service members, have some level of TBI. Of note, 30% of soldiers admitted to Walter Reed Army Medical Center have suffered TBIs.
Traumatic Head Injury Basics
What are the unique features of brain anatomy and physiology, and how do they affect patterns of brain injury?
The head is a rigid compartment filled with brain, cerebrospinal fluid (CSF), and blood.
Cerebral blood flow (CBF) in the healthy individual is autoregulated for systolic blood pressure (SBP) 80 to 160 mm Hg to generate an adequate cerebral perfusion pressure (CPP).
If autoregulation is intact, CBF is maintained constantly via a mean BP adjustment to generate a CPP of 50 to 60 mm Hg.
In moderate or severe brain injury cases, autoregulation is disrupted in a way that CBF varies greatly with mean BP.
The injured brain is more vulnerable to episodes of hypotension and metabolic imbalance which may cause secondary brain injury.
Intracranial Pressure
Besides hemodynamic parameters and confining metabolic conditions, intracranial pressure (ICP) is the single most important determinant of neurological function of the brain (Table 1).
Table 1 Intracranial Pressure | ||||||
|---|---|---|---|---|---|---|
|
Normal ICP is defined as the pressure (in cm H2O) that is measured within the skull, either in subarachnoid fluid, ventricles, or parenchyma. It corresponds to the hydrostatic pressure that must be applied to prevent the emergence of fluid through a puncture needle from the CSF in the horizontal body position. Normal ICP should reside below 15 cm H2O. An increase in ICP occurs when one of the intracranial compartments within the rigid skull is increased (1,500 to 1,700 mL total volume, which is made of around 80% brain parenchyma, 10% CSF, and 10% blood). An acute increase in ICP above tolerance is fatal.
Physiological variations occur and show age dependence, with children having lower values than adults, fluctuation with each pulse-pressure wave, fluctuation with respiration, and a correlation with body weight (obese patient showing higher values).
It must be noted that ICP cannot be predicted on the basis of imaging (head CT or MRI).
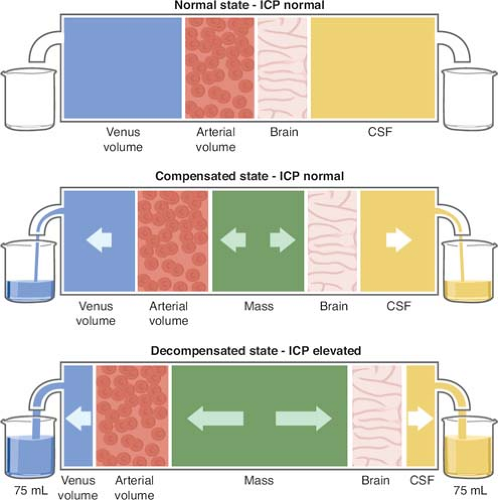
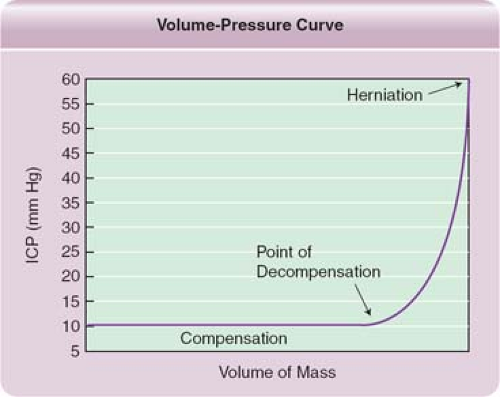
The Monro–Kellie doctrine (Figs. 1 and 2) states that the sum of all intracranial volumes will remain constant and that any increase in one of them or adding an intracranial mass will be offset by an equal decrease in one of its other components, otherwise it will cause an increase in ICP at the expense of the brain.
Icp Impact
In TBI, resulting increased ICP leads to decreased brain function and poor outcome.
Systemic hypotension and low O2-saturation adversely affect outcome via poor CPP and hypoxia (Table 2).
Table 2 Cerebral Perfusion Pressure (CPP) | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Primary and Secondary Brain Injuries
Primary and secondary brain injuries are the terms to classify brain injury processes. In TBI, primary injury occurs during the initial insult and results from the physical impact and energy transfer causing structural damage to the brain. Secondary injury is a consequence thereof. Its time course is more gradual, reflecting the involvement of distinct cellular processes to which both primary and secondary injuries, respectively, will contribute. Primary and secondary injuries occur in other brain insults such as spontaneous hemorrhage, stroke, or mass lesions too.
In TBI, primary injury (Table 3) happens from energy transfer at the moment of trauma and it manifests as concussion (injury without visible correlate on CT), contusion (with damage to tissue and vessels), or diffuse axonal shear injury. Normal physiological barriers such as the blood–brain barrier and connective tissue such as the meninges can be damaged, and cells may die in a nonspecific manner. Certain areas of the brain are more susceptible to injury either by location (fronto-basis and temporal tip in head-on collision deceleration injuries) or by structural features (myelinated fiber tracts vs. nonmyelinated fibers), and this type of structural injury is thought to be irreversible.
Since primary injury occurs at the moment of trauma, there is little that can be done for it; efforts to reduce disability and death from TBI are thought to be best aimed at secondary injury.
Table 3 Examples of Primary Brain Injury in TBI | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Secondary injury (Table 4) is delayed and results indirectly from the impact and comes via cellular processes as a consequence of the trauma. It is a well-known observation that many TBI victims do not die right away at the scene, but almost half of the TBI patients deteriorate during their hospitalization as a result of secondary injury, which ultimately may cause raised ICP and brain herniation.
Table 4 Causes of Secondary Brain Injury | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Since secondary injury occurs over time, it can be prevented in part by taking measures to prevent complications, and researchers are working actively to find drug therapies to limit or prevent the damage.
It is crucial to obtain as much of the history upon arrival of the Emergency Medical Services and particular attention must be paid to the mechanism of injury, initial on-scene examination, and time course of developing symptoms of concern.
Whenever there is significant impact, the index of suspicion of a life-threatening injury should be very high, even if the patient was doing rather well at the scene and looks good on arrival! Whenever there is significant injury to the head (e.g., enough to cause a fracture or bleeding), the concern for associated cervical spine injury should be high. So, actively search for neck pain and signs of radiculopathy or myelopathy! If the patient has sustained multisystem injury, the extent of injury and its initial management matters greatly for prognostic purposes.
Specific scenarios: In cases of motor vehicle accidents (MVA), questions about mechanism of injury should include a detailed account of vehicle speed (high/low), direction of impact (head on, rear ended, side/oblique impact), extend of external damage, possible passenger ejection, and death of or injuries to other participants. In cases of penetrating or blunt injury, ask about the type of assault weapon (e.g., firearm vs. golf club). Get as much information as possible from bystander accounts. It is important not to miss the body temperature in this assessment since hypothermia may depress neurological functions.
Examination
It may be of vital importance to obtain a description of the scenario and vital signs in addition to the first examination at the scene. When a patient is “found down,” ask about circumstantial evidence (alcohol, drugs, observed blood loss). How long was the patient unaccounted for? Was there loss of consciousness (LOC), evidence of seizure activity, or progressive obtundation? Did the patient act abnormally? Did the patient develop headache, nausea, vomiting, blurred vision, hearing loss, altered speech, or any other progressive symptom en route? If the patient became unconscious and arrived with a “blown pupil,” ask when it happened. If bilaterally, ask which side went up first and when.
As in all other trauma cases, assessment of the primary trauma team’s complete survey must be conducted first!
Observe the primary survey by the trauma team as they gather vital signs and make sure that all initial measures to limit secondary brain injury are being implemented (oxygen administered, adequate ventilation secured, and SBP >90 mm Hg maintained at all times).
Check for bradycardia, changes in breathing frequency, and hypertension (signs for increased ICP and Cushing’s response).
Make sure that the patient is being treated with full spine precautions—a hard board is used and the cervical spine is correctly immobilized with a hard collar or taped to the trauma board. Only in the setting of hypovolemic systemic shock (scalp blood loss can be massive!) and in cases of spinal cord injuries with florid neurogenic shock, you will see hypotensive responses despite increased ICP.
During the assessment of the trauma team’s survey, get information about medications given during transport (paralytics, narcotics, sedatives).
Have a quick look at the pupils and check for size and reactivity. A side-difference of >1 mm is considered nonphysiological, unless caused by a preexisting condition. Classify the status of the pupils since any newly dilated pupil >6 mm defines a neurosurgical emergency. Rapid acquisition of head CT-imaging in this setting (e.g., penetrating gunshot wound [GSW] to the
head) takes precedence over a detailed secondary trauma survey!
head) takes precedence over a detailed secondary trauma survey!
Traumatic Brain Injury: the Glasgow Coma Scale
Once the trauma survey has been conducted, evaluate the patient rapidly yourself before other diagnostic studies are done. Check the patient’s initial Glasgow Coma Scale (GCS) score to evaluate the patient’s level of consciousness via motor response, eye opening, and verbal response. This score has predictive and prognostic value (Table 5).
If the patient is stable and in reasonable neurological condition, obtain a focused examination:
Head: Observe the patient for external signs of trauma (raccoon’s eyes = periorbital edema and hematoma, retroauricular hematoma, and ecchymosis = Battle’s sign indicating a skull base injury). Check head and neck for wounds such as lacerations, abrasions, and contusions, and palpate for possible fractures. Do not probe lacerations concerning for open fractures until in the OR and after adequate imaging has been obtained. Inspect and palpate the globes to assess possible rupture. Corneal reflexes can be used to assess CN 5/7 function in the comatose patient. A fundoscopic/ophthalmoscopic examination is less valuable in the adult since ICP increase does not cause immediate optic nerve pallor and it is unlikely that one picks up a decrease in retinal venous pulsations in this ER setting. However, in pediatric patients and unclear mechanism of injury, evidence of retinal hemorrhage may point to abuse. Pharmacological dilatation must be avoided until ICP elevation has been ruled out. Check the external auditory canal (EAC) for hematotympanum and otorrhea/liquorrhea. Also inspect the nares for blood or CSF leakage/rhinorrhea. Lower cranial nerve injury is rare in the acute trauma patients, and if noticed later during hospitalizations, needs attention to assess the risk of aspiration.
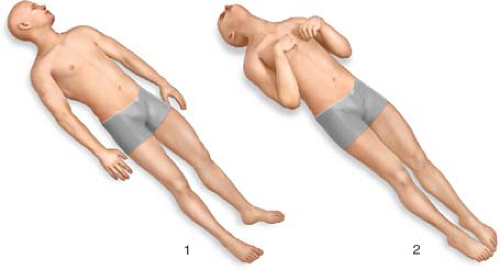
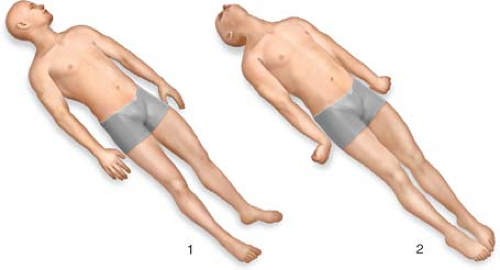
Body: Check for motor response in all four extremities; if the patient has decreased level of consciousness, painful stimuli are applied to elicit an adequate response. Learn to recognize the posturing responses to be able to distinguish decerebrate, decorticate, triple-flexion withdrawal (Figs. 3 and 4)
Table 5 TBI and GCS Scoring Table | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
In conversant patients also check the sensation from the head toward the toes and mark any possible level that correlates with a spinal cord injury. Check tactile stimulation as well as pain. You must perform a rectal examination to assess sphincter tone; in the comatose patient, this may be the only evidence for spinal cord injury. If the bulbocavernosus reflex is missing (reflecting acute myelopathy), the patient may show signs of spinal shock.
Check biceps and patellar reflexes as well as plantar responses (Babinski’s reflex). In acute spinal cord injury, the patient will present with dropped reflexes and mute toes. Only in rare cases of brain stem shear injury, one can find hyperreflexia in the acute setting.
Serial neurological examinations and serial imaging are necessary to diagnose delayed neurological status change and deterioration from secondary brain injury (Table 6).
Table 6 Classification of Injury Patterns | |
|---|---|
|
Initial Treatment Plan in the Er
Since TBI is a rather heterogeneous group of incidents, it has been extremely difficult to gather prospective randomized trial data and treatment recommendations from clinical studies in this scenario. However, a few fundamental and basic recommendations were derived from detailed analysis of retrospective data and prospective collection of data from cohorts that were followed long term.
Some priorities in guidelines are intuitive, for example, the systemically unstable patient needs to be treated first since systemic hypotension from hypovolemic shock in the multitrauma patient carries a poor prognosis in neurotrauma. Also, if there are any concerns for raised ICP or the GCS score is <9, the patient should have the treatment initiated imaging is obtained before, and then the time-consuming diagnostic studies are undertaken (see later).
Icp Treatment
After systemic stabilization (make sure only isotonic solutions are used), administer mannitol (around 1 g/kg BW) and furosemide (Lasix) (10 to 20 mg IV) and hyperventilate the patient (increase frequency and volume for goal pCO2 = 30) before you run off to radiology/CT for further studies.
The current existing guidelines for management of acute head trauma are contained by a publication of the Brain Trauma Foundation and the American Association of Neurological Surgeons (AANS) and can be obtained from the AANS or found via Weblink under: http://www.guideline.gov/content.aspx?id=10995.
Some points of interest need to be described when accepting or signing out a patient: single versus multiple wounds, LOC at the scene, GCS score at the scene, downtime until patient was found and treatment was initiated, seizures at the scene, and any accompanying systemic injury. Then focus on the actual neurological injury:
Document the mechanism of injury as nonpenetrating blunt trauma in which the bony confinements remain intact (e.g., strike with a baseball bat) versus penetrating trauma in which the bony integrity has been violated (GSW and stabs). It is helpful to realize that the energy transfer accounts for the devastation, so one should specify “high energy” versus “low energy” injury. On the basis of the initial GCS score, you can stratify the injury into mild, moderate, and severe (see Table 6).
Document the morphology: Surface and vault injuries: open versus closed, depressed versus nondepressed, with and without translocated fragments. Basilar injuries: with or without CSF leak, with or without cranial nerve palsy.
Once a CT of the head as been obtained, classify the injury pattern into bony and parenchymal: epidural/subdural/subarachnoid/intracerebral/focal or diffuse (see later).
Upon arrival, the patient will undergo some ER management in the hospital. Here are some conservative measures that can be initiated quickly and efficiently (Tables 7 and 8).
Table 7 First Set of Conservative TBI Treatment Measures (Before Imaging) | |
|---|---|
|
Table 8 Second Set of Conservative TBI Treatment Measures (After Imaging) | |
|---|---|
|
Strategy in the Trauma Bay:
Early intervention is the goal for all treatable conditions
Each patient with a significant impact or unclear story must be studied with imaging.
Comatose TBI patients (GCS score of ≤8) with normal CT scans may be watched during further workup.
All comatose TBI patients (GCS score of ≤8) with abnormal CT scans should receive invasive ICP monitoring.
This algorithm helps with earlier detection of intracranial lesions to prognosticate recovery and it improves outcome.
CT of the head is the study of choice in head trauma patients. All patients with a GCS score of <15 should obtain a CT scan for proper assessment. Patients who look perfect but have a significant mechanism of injury as well as patients on systemic anticoagulation and with syncopal events should also be imaged. In all patients with a lateralizing or localizing sign, the radiographic workup must be obtained emergently since it is highly specific and sensitive for bony injuries as well as blood and gives a chance to assess intracranial injuries in a timely fashion. (Timely means a significant head injury should be imaged within 15 minutes after arrival in the ER.) Most indications for surgical intervention can be made on the basis of CT results alone and do not require MRI, which is superior only for prognostic purposes in patients with shear injuries and diffuse axonal injury (Fig. 5; Tables 10 and 11).
Table 9 Dosing Table for Medications | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree