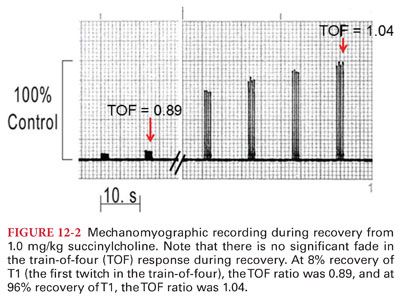
B. Depolarizing neuromuscular block (also called phase I block) is often preceded by muscle fasciculation. During partial neuromuscular block, depolarizing block is characterized by (a) decrease in twitch tension, (b) no fade during repetitive stimulation (tetanic or TOF), and (c) no posttetanic potentiation (Fig. 12-2).
V. Pharmacology of Succinylcholine
A. Structure–Activity Relationships for Succinylcholine
1. Succinylcholine is a long, thin, flexible molecule composed of two molecules of acetylcholine linked through the acetate methyl groups (Fig. 12-3).
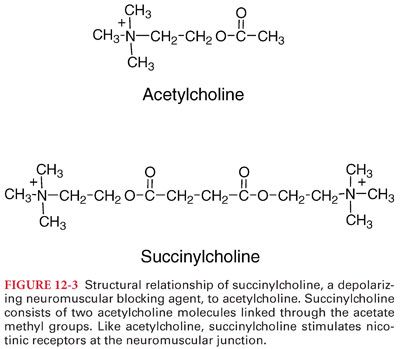
2. Like acetylcholine, succinylcholine stimulates cholinergic receptors at the neuromuscular junction and at nicotinic (ganglionic) and muscarinic autonomic sites, opening the ionic channel in the acetylcholine receptor.
B. Pharmacokinetics, Pharmacodynamics, and Pharmacogenomics of Succinylcholine
1. Succinylcholine has an elimination half-life of 47 seconds (95% confidence interval of 24 to 70 seconds), and the dose of succinylcholine causing on average 95% suppression of twitch height (the ED95) is approximately 0.3 mg/kg.
2. The usual dose of succinylcholine required for tracheal intubation in adults is 1.0 mg/kg (results in complete suppression of response to neuromuscular stimulation in approximately 60 seconds).
3. In patients with genotypically normal butyrylcholinesterase activity, time to recovery to 90% muscle strength following administration of 1 mg/kg succinylcholine ranges from 9 to 13 minutes.
4. The short duration of action of succinylcholine is due to its rapid hydrolysis by butyrylcholinesterase (plasma cholinesterase) to succinylmonocholine and choline.
a. There is little or no butyrylcholinesterase at the neuromuscular junction.
b. Butyrylcholinesterase influences the onset and duration of action of succinylcholine by controlling the rate at which the drug is hydrolyzed in the plasma before it reaches, and after it leaves, the neuromuscular junction.
C. Factors Affecting Butyrylcholinesterase Activity
1. Butyrylcholinesterase is synthesized by the liver and found in the plasma.
2. Butyrylcholinesterase is responsible for metabolism of succinylcholine, mivacurium, procaine, chloroprocaine, tetracaine, cocaine, and heroin. Neuromuscular block induced by succinylcholine or mivacurium is prolonged when there is a significant reduction in the concentration or activity of butyrylcholinesterase.
3. Neostigmine (and to a lesser degree edrophonium) causes a profound decrease in butyrylcholinesterase activity. Even 30 minutes after administration of neostigmine, the butyrylcholinesterase activity remains about 50% of control values.
D. Genetic Variants of Butyrylcholinesterase
1. Neuromuscular block induced by succinylcholine or mivacurium can be significantly prolonged if the patient has an abnormal genetic variant of butyrylcholinesterase.
2. The dibucaine number reflects quality of cholinesterase enzyme (ability to hydrolyze succinylcholine) and not the quantity of the enzyme that is circulating in the plasma.
a. In case of the usual butyrylcholinesterase genotype (E1uE1u), the dibucaine number is 70 or higher, whereas in individuals homozygous for the atypical gene (E1aE1a) (frequency in general population of 1 in 3,500), the dibucaine number is less than 30.
b. In individuals with the heterozygous atypical variant (E1uE1a) (frequency in general population of 1 in 480), the dibucaine number is in the range of 40 to 60.
c. In individuals with the homozygous atypical genotype (E1aE1a), the neuromuscular block induced by succinylcholine or mivacurium is prolonged to 4 to 8 hours, and in individuals with the heterozygous atypical genotype (E1uE1a), the period of neuromuscular block induced by succinylcholine or mivacurium is about 1.5 to 2 times that seen in individuals with the usual genotype (E1uE1u).
3. Phase II block may appear after prolonged or repeated administration of succinylcholine and has characteristics similar to nondepolarizing neuromuscular blockers (edrophonium or neostigmine do not consistently result in adequate antagonism of neuromuscular blockade). The alternative is to keep the patient adequately sedated and maintain artificial ventilation until the TOF ratio has recovered to 0.9 or more.
E. Side Effects of Succinylcholine
1. Cardiovascular Effects
a. Sinus bradycardia, junctional rhythm, and even sinus arrest may follow administration of succinylcholine. Cardiac dysrhythmias are most likely to occur when a second dose of succinylcholine is administered approximately 5 minutes after the first dose. Atropine is effective in treating or preventing bradycardia.
b. In contrast to actions at cardiac muscarinic cholinergic receptors, the effects of succinylcholine at autonomic nervous system ganglia may produce ganglionic stimulation and associated increases in heart rate and systemic blood pressure.
2. Hyperkalemia
a. The administration of succinylcholine is associated with approximately 0.5 mEq/dL increase in the plasma potassium concentration in healthy individuals, which is well tolerated and generally does not cause dysrhythmias. (Patients with renal failure are no more susceptible to an exaggerated hyperkalemic response.)
b. Succinylcholine has been associated with severe hyperkalemia in patient conditions associated with upregulation of extrajunctional acetylcholine receptors (e.g., hemiplegia or paraplegia, muscular dystrophies, Guillain-Barré syndrome, and burn).
3. Increased Intraocular Pressure
a. Succinylcholine usually causes an increase in intraocular pressure (peaks at 2 to 4 minutes after administration and returns to normal by 6 minutes).
b. The use of succinylcholine is not widely accepted in open eye injury (when the anterior chamber is open) even though succinylcholine has not been shown to cause adverse events.
4. Increased Intragastric Pressure. Administration of succinylcholine does not predispose to regurgitation in patients with an intact lower esophageal sphincter because the increase in intragastric pressure does not exceed the “barrier pressure.”
5. Increased Intracranial Pressure. The potential for succinylcholine to increase intracranial pressure can be attenuated or prevented by pretreatment with a nondepolarizing neuromuscular blocker.
6. Myalgias
a. Postoperative skeletal muscle myalgia, which is particularly prominent in the skeletal muscles of the neck, back, and abdomen, can occur after administration of succinylcholine, especially to young adults undergoing minor surgical procedures that permit early ambulation. Myalgia localized to neck muscles may be perceived as pharyngitis (“sore throat”) by the patient and attributed to tracheal intubation by the anesthesiologist.
b. Muscle pain occurs more frequently in patients undergoing ambulatory surgery, especially in women, than in bedridden patients.
c. Myalgia may best be prevented with muscle relaxants, lidocaine, or nonsteroidal antiinflammatory drugs. However, myalgias following outpatient surgery occur even in the absence of succinylcholine.
7. Masseter Spasm. An increase in tone of the masseter muscle may be an early indicator of malignant hyperthermia, but it is not consistently associated with malignant hyperthermia.
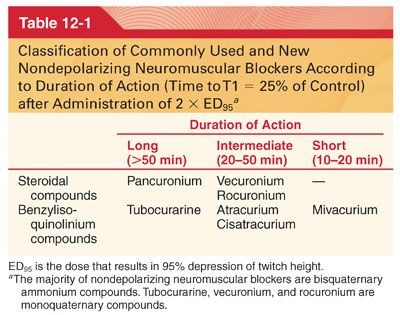
VI. Pharmacology of Nondepolarizing Neuromuscular Blockers (Tables 12-1 to 12-3)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


