107. You see that midazolam was the first drug given to the patient—actually right before she was transported into the OR. (The notation IVP next to midazolam means “IV push,” ie, a rapid bolus injection.) In addition to causing sedation, anxiety relief, and generally “smoothing” the induction of anesthesia, which of the following is the most likely effect you would expect to achieve as a result of premedicating with midazolam?
a. Potentiating the analgesic effects of the morphine
b. Preventing an intraoperative fall of blood pressure
c. Preventing seizures likely to be caused by the propofol
d. Prophylaxis of cardiac arrhythmias
e. Providing amnestic effects (suppressing recall of perioperative events)
108. The record shows that propofol was given for induction. What is/are the most likely adverse response(s) associated with the administration of this widely used drug?
a. Hypotension and respiratory (ventilatory) depression
b. Laryngospasm
c. Long-term memory loss
d. Malignant hyperthermia
e. Seizures
f. Unintended or excessively prolonged skeletal muscle paralysis
109. Assume that instead of inducing anesthesia with propofol, the nurse anesthetist used a parenteral barbiturate (eg, methohexital, thiamylal, and thiopental) with an extremely fast onset of action and short duration (sometimes called “ultrashort”). These barbiturate induction agents are effective, but are associated with a fairly high incidence of a certain and rather unique adverse effect. What best describes what that adverse effect is?
a. Hyperalgesia (heightened perception of pain)
b. Hypertensive crisis
c. Laryngospasm
d. Malignant hyperthermia
e. Seizures, typically monoclinic
110. The patient received an intravenous dose of ketorolac shortly before the wounds were closed and surgery was done. What is the most likely purpose for which it was given?
a. Control of anticipated postoperative nausea and vomiting
b. Postoperative pain control
c. Reversal of CNS depression caused by multiple depressant drugs
d. Reversal of drug-induced neuromuscular blockade (paralysis)
e. Suppression of wound inflammation
111. Ondansetron was administered about an hour before the anticipated end of surgery. What was the most likely reason for giving this to the patient?
a. Hasten recovery of consciousness while effects of anesthetics wear off
b. Intensify pain-relieving effects of other analgesics given to the patient
c. Lessen risks of postop urinary retention through effects on bladder musculature
d. Prevent or reduce the risk of postoperative paralytic ileus
e. Reduce the risk of postoperative nausea and vomiting
112. Two inhaled general anesthetics, A and B, have the following MAC values:
![]()
Based only on this information (note that we have not named any drugs), which statement is true?
a. Drug A has a longer duration of action than Drug B
b. Drug A is more soluble in the blood than Drug B
c. Drug B causes greater analgesia and skeletal muscle relaxation than Drug A
d. The concentration of drug in inspired air that is needed to cause adequate surgical anesthesia is higher for Drug B than for Drug A
e. The time to onset of adequate general anesthesia is 50 times longer for Drug B than for Drug A
113. A patient with Parkinson disease has signs and symptoms that can be considered “moderate” now, but they are worsening and not responding well to current drug therapy. The physician decides to empirically assess an antiparkinson drug that is a selective inhibitor of monoamine oxidase type B (MAO-B). What drug would that be?
a. Bromocriptine
b. Carbidopa
c. Phenelzine
d. Selegiline
e. Tranylcypromine
114. A patient who has been treated with levodopa is switched to a regimen with a product that contains levodopa plus carbidopa. What is the main action of carbidopa that provides the rationale for using it in this dual-drug approach?
a. Blocks ACh release in the CNS, thereby facilitating levodopa’s ability to restore a dopamine-ACh balance
b. Helps activate dietary vitamin B6, a deficiency of which occurs during levodopa therapy
c. Increases permeability of the blood-brain barrier to levodopa, giving levodopa better access to the CNS
d. Inhibits metabolic conversion of levodopa to dopamine outside the CNS
e. Reduces levodopa-induced hypotension by blocking vascular dopamine receptors
115. A 34-year-old man with mild anxiety and depression symptoms has heard about buspirone on TV and asks whether it might be suitable for him. According to the most diagnostic and treatment criteria, the drug would be appropriate, particularly for short-term symptom control. Which phrase correctly describes an important property of buspirone?
a. Associated with a withdrawal syndrome that, if unsupervised or controlled, may be fatal
b. Has a significant potential for abuse
c. Is likely to potentiate the CNS depressant effects of alcohol, benzodiazepines, and sedative antihistamines (eg, diphenhydramine), so such interactants must be avoided at all cost
d. Requires almost daily dosage titrations in order to optimize the response
e. Seldom causes drowsiness
116. A physician considers placing a patient on long-term (months, years) phenobarbital for control of a relatively common medical condition. For most of these indications, newer and arguably more efficacious drugs, which participate in fewer drug interactions, are available and preferred. For which one of the following uses, nonetheless, is this barbiturate still considered reasonable and appropriate?
a. Alcohol withdrawal signs/symptoms
b. Anxiety management
c. Certain epilepsies
d. Endogenous depression (adjunct to SSRIs)
e. Sleep disorders such as insomnia
117. One reason for the declining use of tricyclic antidepressants such as imipramine, and the growing use of newer classes, is the prevalence of common tricyclic-induced side effects or adverse responses. What side effect or adverse response, listed below, is most likely to occur with usual therapeutic doses of a tricyclic?
a. Anticholinergic (antimuscarinic) effects
b. Arrhythmias
c. Hepatotoxicity
d. Nephrotoxicity
e. Seizures
118. A 42-year-old woman develops akathisias, parkinsonian-like dyskinesias, galactorrhea, and amenorrhea, as a consequence of psychotropic drug therapy. What drug-receptor-based mechanism, occurring in the central nervous system, most likely caused these responses?
a. Blockade of α-adrenergic receptors
b. Blockade of dopamine receptors
c. Blockade of muscarinic receptors
d. Supersensitivity of dopamine receptors
e. Stimulation of nicotinic receptors
119. A patient on the trauma-burn unit received a drug to ease the pain of debridement and dressing changes for several severe burns. He experiences good, prompt analgesia, but despite the absence of pain sensation during the procedure his heart rate and blood pressure rise considerably, consistent with sympathetic nervous system activation by the pain and not affected by the analgesic drug. As the effects of the drug develop his skeletal muscle tone progressively increases. He appears awake at times because his eyes periodically open. As drug effects wear off he hallucinates and behaves in a very agitated fashion. Hallucinations, “bad dreams,” and periods of delirium recur over several days after receiving the drug. What drug was most likely given?
a. Fentanyl
b. Ketamine
c. Midazolam
d. Succinylcholine
e. Thiopental
120. A 17-year-old male was diagnosed with epilepsy after developing repeated episodes of generalized tonic-clonic seizures following a motor vehicle accident in which he received a closed-head injury. After treating acute seizures with the proper injectable drugs, he is started on a regimen of oral phenytoin, the daily dose titrated upward until symptom control and a therapeutic plasma concentration were reached. The elimination half-life of the drug during initial treatment was measured to be 24 hours, a value that is quite typical for otherwise healthy adults taking no other drugs.
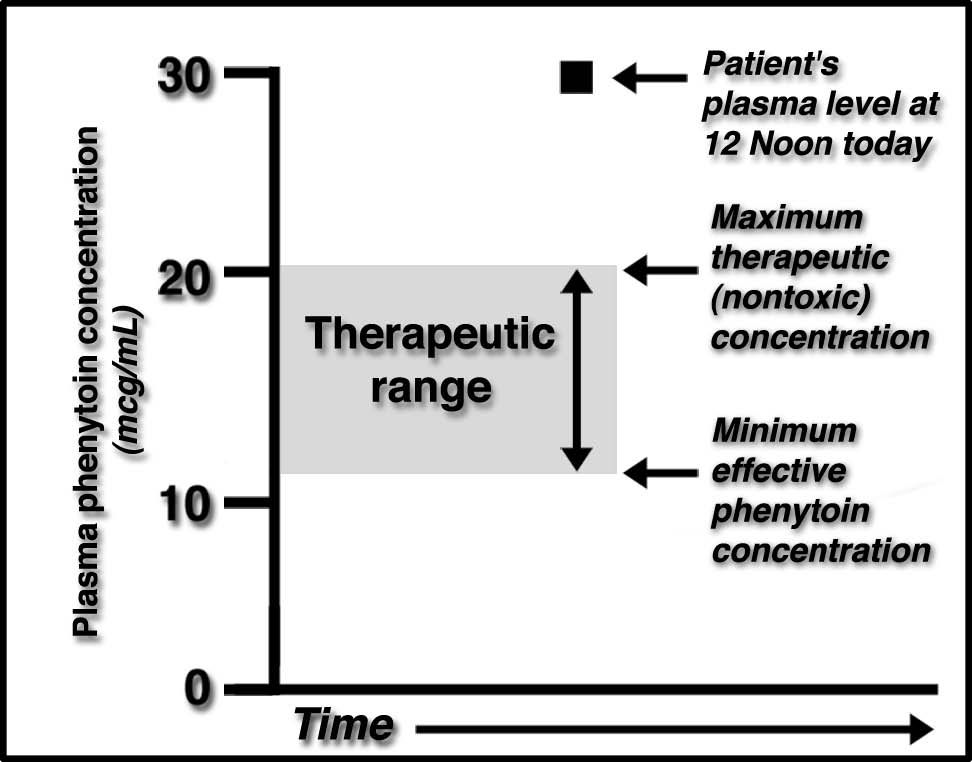
Today he presents in the neurology clinic with nystagmus, ataxia, diplopia, cognitive impairment, and other signs and symptoms consistent with phenytoin toxicity. A blood sample, drawn at noon, has a plasma phenytoin concentration of 30 mcg/mL. That value is 50% higher than typical peak therapeutic plasma concentrations, and twice the usual minimum effective blood level. These values are summarized in the figure below.
The attending orders discontinuation of further doses of phenytoin until plasma levels fall into the therapeutic range, and the patient is largely free of signs and symptoms of phenytoin toxicity. In the interim, what would you do or expect to occur next?
a. Administer flumazenil, which will quickly reverse signs and symptoms of phenytoin toxicity but may cause seizures to recur
b. Anticipate that elimination of phenytoin from the plasma will follow zero-order kinetics for several days
c. Give an amphetamine or other CNS stimulant to reverse generalized CNS depression due to the phenytoin excess
d. Give phenobarbital to induce the P450 system, thereby hastening phenytoin’s metabolic elimination
e. Plasma phenytoin concentrations will fall to 15 mcg/mL, in the middle of the therapeutic range, by noon tomorrow (24 hours later, per the usual half-life)
121. A 12-year-old boy has been treated with methylphenidate for the last 3 years. His younger sister finds the bottle of pills and consumes enough to cause significant toxicity. Which of the following findings would you most likely expect?
a. Hypertension, tachycardia, seizures
b. Hypotension, bronchospasm
c. Drowsiness, obtunded reflexes, diarrhea
d. Miosis, bradycardia, profuse salivation, sweating
e. Hypothermia, skeletal muscle weakness or paralysis, pupils that are not responsive to light
122. Meperidine is similar to morphine in many ways, but has some decided differences that are clinically relevant: with very high blood levels or with true overdoses, meperidine can cause significant adverse responses that simply aren’t seen with morphine or most other opioid analgesics. What is that rather unique effect of meperidine?
a. Constipation leading to paralytic ileus
b. Heightened response to pain (paradoxical hyperalgesia)
c. Intense biliary tract spasm
d. Psychosis-like state, possibly seizures
e. Respiratory depression, apnea, ventilatory arrest
123. Chlorpromazine and haloperidol can be considered prototypes of two relatively old but still-used antipsychotic drug classes: the phenothiazines and the butyrophenones, respectively. While many of the actions and side effects of these drugs are qualitatively similar, they are different quantitatively: that is, in terms of incidence and severity. Which effect or side effect typically occurs more frequently, is usually more severe, and has a relatively rapid onset, with haloperidol?
a. Extrapyramidal reactions
b. Intense atropine-like side effects
c. Lethal blood dyscrasias
d. Orthostatic hypotension
e. Urinary retention necessitating bladder catheterization
124. A patient is transported to the emergency department. A friend who accompanies the patient says “he was experimenting with ‘angel dust’”. What best describes the actions or other characteristics of this recreational drug, more properly know as phencyclidine?
a. Causes its peripheral and central effects via antimuscarinic properties
b. Causes significant withdrawal symptoms
c. Has strong opioid receptor-activating activity
d. Has amphetamine-like properties and is an hallucinogen
e. Overdoses should be treated with flumazenil
125. Package inserts for a drug caution against administering it concurrent with any other drug that can raise or lower sodium concentrations. The risks are inadequate or excessive effects of the drug, depending on the direction in which sodium concentrations change. This, of course, requires cautious use or avoidance (if possible) of the common diuretics. To which of the following drugs does this caution or warning apply?
a. Cholestyramine
b. Lithium (eg, lithium carbonate)
c. Nifedipine
d. Phenylephrine
e. Statin-type cholesterol-lowering drugs
126. A 31-year-old woman has been treated with fluoxetine for 5 months. She is diagnosed with another medical problem and receives one or more drugs that, otherwise, would be suitable and probably problem-free. She is rushed to the ED with unstable vital signs, muscle rigidity, myoclonus, CNS irritability and altered consciousness, and shivering. What add-on drug(s) most likely caused these responses?
a. Codeine for cough
b. Loratadine for seasonal allergies
c. Midazolam and fentanyl, used to ease discomfort from endoscopy
d. Sumatriptan for migraine
e. Zolpidem for short-term insomnia
127. A 72-year-old woman with a long history of anxiety that has been treated with diazepam decides to triple her daily dose because of increasing fearfulness about “environmental noises.” Two days after her attempt at self-prescribing, she is found extremely lethargic and nonresponsive, with markedly obtunded reflexes and reactions to painful stimuli. Respirations are 8/min and shallow. What drug should be given to reverse these signs and symptoms?
a. Dextroamphetamine
b. Flumazenil
c. Naltrexone
d. Physostigmine
e. Pralidoxime
128. A patient who has been treated for Parkinson disease for about a year presents with purplish, mottled changes to her skin. What drug is the most likely cause of this cutaneous response?
a. Amantadine
b. Bromocriptine
c. Levodopa (alone)
d. Levodopa combined with carbidopa
e. Pramipexole
129. A young boy who has been treated for epilepsy for a year is referred to a periodontist for evaluation and probable treatment of massive overgrowth of his gingival tissues. Some teeth are almost completely covered with hyperplastic tissue. Which drug was the most likely cause of the oral pathology?
a. Carbamazepine
b. Lorazepam
c. Phenobarbital
d. Phenytoin
e. Valproic acid
130. A patient with undiagnosed coronary artery disease is given a medication. Shortly thereafter she develops intense tightness and “crushing discomfort” of her chest. An ECG reveals ST-segment changes indicative of acute myocardial ischemia. Which drug most likely caused this reaction?
a. Clozapine
b. Pentazocine
c. Phenytoin
d. Sumatriptan
e. Zolpidem
131. Nitrous oxide is a common component in the technique of balanced anesthesia. It is used in conjunction with such other drugs as a halogenated hydrocarbon volatile liquid anesthetic, and usually included as 80% of the total inspired gas mixture. Which phrase best summarizes why nitrous oxide cannot be used alone for general anesthesia?
a. Almost total lack of analgesic activity, regardless of concentration
b. Inspired concentrations >10% tend to profound cardiac negative inotropic effects
c. MAC (minimum alveolar concentration) is >100%
d. Methemoglobinemia occurs even with low inspired concentrations
e. Such great solubility in blood that its effects take an extraordinarily long time to develop
f. Very high frequency of bronchospasm
132. A patient develops a severe and rapidly worsening adverse response to a drug. The physician orders prompt administration of antipyretics, IV hydration, and bromocriptine or dantrolene to manage symptoms and hopefully to prevent a fatal outcome. Which drug or drug group most likely caused these adverse responses?
a. Benzodiazepines, especially those used as hypnotics
b. Chlorpromazine
c. Levodopa
d. Phenytoin
e. SSRIs
133. Ropinirole is a relatively new drug that recently was approved to treat what’s commonly called restless leg syndrome (also known as Ekbom syndrome). The drug works as a dopamine receptor agonist in certain parts of the brain. Given this mechanism of action, what other disorder is, most likely, another indication for this drug?
a. Daytime anxiety
b. Hypersomnia (excessive sleepiness)
c. Parkinson disease
d. Schizophrenia
e. Status epilepticus
f. Treatment of severe pain
134. A patient in the neurology unit at your hospital develops status epilepticus, and at the time there is no good information about the etiology. What drug should be given first for the fastest suppression of the seizures?
a. Carbamazepine
b. Lorazepam
c. Phenobarbital
d. Phenytoin
e. Valproic acid
135. A patient has had a documented severe allergic reaction to ester-type local anesthetics. What other drug is a member of the ester class, and so would be the most likely to provoke an allergic or anaphylactic reaction if this patient received it?
a. Bupivacaine
b. Lidocaine
c. Mepivacaine
d. Prilocaine
e. Tetracaine
136. A 66-year-old woman is diagnosed with Alzheimer disease, with symptoms being described as mild-to-moderate. What pharmacologic approach is generally considered the most fruitful in terms of alleviating symptoms of early Alzheimer and probably slowing the course of the underlying brain pathology?
a. Activate a population of serotonin receptors
b. Block dopamine release or receptor activation
c. Inhibit acetylcholinesterase
d. Inhibit MAO
e. Dissolve cerebral vascular thrombi
137. Trihexyphenidyl is prescribed as an adjunct to other drugs being used to manage a patient with Parkinson disease. What is the most likely purpose or action of this drug as part of the overall drug treatment plan?
a. To counteract sedation that is likely to be caused by the other medications
b. To help correct further the dopamine-ACh imbalance that accounts for parkinsonian signs and symptoms
c. To manage cutaneous allergic responses that are so common with “typical” anti-parkinson drugs
d. To prevent the development of manic/hypomanic responses to other antiparkinson drugs
e. To reverse tardive dyskinesias if the parkinsonism was induced by an antipsychotic drug
138. A few years ago the FDA granted approval to market a new prescription drug (“drug X”) that will be administered in the form of a dermal patch (apply the patch to intact skin, the drug is absorbed from there).
Drug X belongs to a very old class of drugs that, when given by its usual route, orally, can interact with foods such as cheese and processed meats (and certain breads, other foods, and alcoholic beverages) leading to an interaction that can elevate blood pressure to severe and sometimes fatal levels. After more than a decade of testing, the FDA approved its use for adults. In its lowest dose, no dietary restriction(s) are required.
Based on this information, how is drug X most likely classified and what is its most likely clinical use?
a. Amphetamine-like agent for ADD/ADHD
b. Barbiturates used for daytime anxiety
c. Benzodiazepine for anxiety and sleep
d. MAO inhibitor for depression
e. Morphine-like analgesic for severe/chronic pain
139. The pediatrician writes a prescription for a combination (of several drugs) product that contains dextromethorphan, which is an isomer of a codeine analog. The patient is a 12-year-old boy. What is the most likely purpose for which the drug was prescribed?
a. Control mild-moderate pain after the lad broke his wrist playing soccer
b. Manage diarrhea caused by food-borne bacteria
c. Provide sedation because the child has ADD/ADHD
d. Suppress severe cough associated with a bout of influenza
e. Treat nocturnal bed-wetting
140. Many legal jurisdictions have imposed various restrictions on over-the-counter sale of products, mainly oral decongestants, that contain pseudoephedrine. That is because pseudoephedrine can be rather easily used to synthesize which highly psychoactive and abuse-prone drug?
a. Methamphetamine
b. Morphine
c. Oxycodone
d. Pentazocine
e. Phencyclidine (PCP)
141. The anesthesiologist prepares to administer several drugs to a patient as part of normal pre- and intraoperative care. What drug lacks, as its normal spectrum of action, the ability to cause generalized CNS depression or the patient’s level of consciousness, or lacks any intrinsic analgesic effects?
a. Droperidol
b. Midazolam
c. Vecuronium
d. Propofol
e. Thiopental
142. A 26-year-old woman has been on antidepressant therapy for several months. Today she complains of missing her period and having galactor-rhea, and your careful assessment suggests that she has developed some dyskinesias (mild tremors, for example) not unlike those you would typically associate with a phenothiazine or butyrophenone (eg, haloperidol) antipsychotic drug. Pregnancy tests are negative. What drug most likely to have caused these findings?
a. Amoxapine
b. Citalopram
c. Fluoxetine
d. Sertraline
e. Tranylcypromine
143. A patient has been taking an oral monoamine oxidase inhibitor (MAOI), but that fact is unknown to the health team who is now taking care of her, for unrelated medical conditions, in the hospital. The patient receives a drug that leads to a fatal response characterized by profound fever, delirium, psychotic behavior, and status epilepticus. It was found to have occurred because of an interaction with the MAOI. Which, most likely, was this second drug or the drug class to which it belongs?
a. Barbiturate
b. Diazepam
c. Meperidine
d. Morphine
e. Phenytoin
144. A young woman is taken to the emergency department by some of her friends. It seems they were out on “bar night” and someone slipped something into her alcoholic beverage, the first and only one she consumed that night. She is now extraordinarily drowsy and has little recall of what happened between the time she sipped her drink and now. Someone overheard another bar patron talking about “roofies.” You suspect her drink was spiked with Rohypnol, the lesser-known generic name of which is flunitrazepam. A positive response (ie, symptom improvement) to what drug that you give would confirm your suspicion?
a. Diazepam
b. Flumazenil
c. Ketamine
d. Naltrexone
e. Triazolam
145. In deciding on pharmacotherapy for many patients you’ve diagnosed with depression, you’ve usually considered starting with an SSRI or, in some cases, a tricyclic. Today you assess a patient and suspect endogenous depression. While discussing treatment options they refer to a drug by name and ask you about it; they’ve seen many advertisements for it in magazines and on TV. The drug (generic name) is bupropion. In what main way does bupropion differ from either or both the SSRIs or tricyclics?
a. Higher incidence of CNS depression, drowsiness
b. Higher incidence of weight gain
c. Less drug-induced sexual dysfunction
d. Much more common and severe falls of resting blood pressure and orthostatic hypotension
e. More severe and more frequent peripheral anticholinergic (atropine-like) side effects
f. Stronger inhibition of monoamine oxidase
146. A 33-year-old woman patient treated with haloperidol is seen in the emergency department (ED). Her husband describes complaints of rapidly worsening fever, muscle stiffness, and tremor. Her level of consciousness is diminishing. Her temperature is 104°F, and her blood creatine kinase (CK) level is elevated. What is the most likely explanation for these findings?
a. Allergic response to her medication
b. Neuroleptic malignant syndrome (NMS)
c. Overdose
d. Parkinsonism
e. Tardive dyskinesia
147. Nearly all the drugs used as primary therapy, or as adjuncts, for the treatment of Parkinson disease or drug-induced parkinsonism exert their desired effects directly in the brain’s striatum. Which one exerts its main effects in the gut, not in the brain?
a. Amantadine
b. Benztropine
c. Bromocriptine
d. Carbidopa
e. Selegiline
148. You have a patient with severe postoperative pain who is not getting adequate analgesia from usually effective doses of morphine. The physician orders an immediate switch to pentazocine (at usually effective analgesic doses). What is the most likely outcome of stopping the morphine and immediately starting the pentazocine?
a. Abrupt, added respiratory depression
b. Acute development of physical dependence
c. Coma
d. Seizures
e. Worsening of pain
149. The chosen pharmacologic approach to managing a patient with mild and recently diagnosed parkinsonism will be to enhance specifically the activity of endogenous brain dopamine by inhibiting its metabolic inactivation. What drug works primarily by that mechanism?
a. Benztropine
b. Selegiline
c. Trihexyphenidyl
d. Bromocriptine
e. Chlorpromazine
150. Chlorpromazine has been prescribed for a patient with schizophrenia, and the patient has been taking the drug, at usually effective doses, for about 6 months. Today he comes to the hospital with other medical conditions that require surgery and the administration of other drugs, and we decide it is unwise to stop the chlorpromazine and run the risk of psychotic behavior while we perform other interventions. What other signs/symptoms that the patient may also have or acquire as the result of surgery and drug therapy are most likely to be affected beneficially by the continued use of chlorpromazine?
a. Epilepsy and the risk of seizures
b. Hypotension
c. Nausea and vomiting
d. Urinary retention caused by abdominal surgery
e. Xerostomia (dry mouth) caused by antimuscarinic drugs used to prevent intra-operative bradycardia
151. There are, rightfully, concerns about cocaine abuse, and too many deaths have occurred from smoking “crack” cocaine or injecting or nasally inhaling the drug. What statement best describes the main mechanism by which cocaine exerts its deleterious effects in the central nervous system or in the periphery?
a. Directly activates, as an agonist, both α- and β1-adrenergic receptors
b. Enhances neuronally mediated adrenergic receptor activation by inhibiting neuronal norepinephrine reuptake
c. Inhibits catecholamine inactivation by inhibiting MAO and catechol-O-methyltransferase
d. Produces bradycardia and vasodilation, leading to hypotension and acute heart failure, by blocking neuronal NE release
e. Stimulates autonomic nerve conduction effectively, leading to increased neuronal norepinephrine release
152. One approach to managing hyperprolactinemia is to administer a drug that has relative selectivity, as an agonist, for central (as an agonist) dopamine D2 receptors. What drug works in that manner?
a. Bromocriptine
b. Chlorpromazine
c. Fluphenazine
d. Haloperidol
e. Promethazine
153. We perform a meta-analysis on the ability of various antipsychotic drugs to cause constipation, urinary retention, blurred vision, and dry mouth—all of which reflect significant blockade of muscarinic receptors in the peripheral nervous systems. What drug most likely caused these unwanted effects?
a. Chlorpromazine
b. Clozapine
c. Haloperidol
d. Olanzapine
e. Sertraline
154. It is obvious that morphine should always be administered “with care.” However, one of its expected effects that occur only while the drug is being given makes it particularly dangerous to administer to certain patients unless “special measures” can be taken to prevent this adverse effect. Which comorbidity weighs against using morphine, unless you first take precautions to prevent adverse consequences from occurring?
a. Acute pulmonary edema
b. Closed-head injury
c. History of epilepsy
d. Hypertension
e. Recent/evolving myocardial infarction
155. A 66-year-old woman has terminal cancer, and is in hospice. She is receiving round-the-clock opioids, at rather high doses, but still reports what she describes as significant burning, shooting pain. The physician believes it is neuropathic. Increasing the dose of opioids may be helpful, but that option is ruled-out at this time because doing so is likely to suppress ventilation excessively. In addition, the patient does not want the excessive grogginess that is apt to occur with more opioid on board. Although the patient is not at all hypertensive, the physician prescribes as an analgesic adjunct that is far more widely used as an antihypertensive drug. What is the most likely adjunctive drug she prescribed?
a. Captopril
b. Clonidine
c. Hydrochlorothiazide
d. Labetalol
e. Prazosin
156. A patient is on long-term methadone therapy as part of a holistic plan to curb their opioid addiction and abuse. What phrase best describes a characteristic of this drug?
a. Causes pentazocine-like activation of κ receptors and blockade of μ receptors
b. Has greater oral bioavailability than morphine, especially when oral administration is started
c. Remarkably devoid of such typical opioid analgesic side effects as constipation and respiratory depression
d. Useful for maintenance therapy in opioid- (eg, heroin-) dependent individuals, but lacks clinically useful analgesic effects
e. When abruptly stopped after long-term administration, causes a withdrawal syndrome that is more intense, but briefer, than that associated with morphine or heroin withdrawal
157. A mom gets a note from her 10-year-old daughter’s teacher that the child recently started experiencing numerous albeit brief episodes of “just staring into space” throughout the school day. The mother realizes she’s noticed the same in her girl at home. After a trip to the pediatrician, and referral to a neurologist, a diagnosis of absence epilepsy is made. What drug is generally considered the preferred starting drug for this type of epilepsy in an otherwise healthy child?
a. Diazepam
b. Ethosuximide
c. Lorazepam
d. Methylphenidate
e. Phenytoin
158. A 43-year-old woman becomes hypertensive and suffers a fatal acute coronary syndrome shortly after starting therapy on a drug. Autopsy shows little in the way of coronary atherosclerosis, but ECG changes noted just before her death revealed significant myocardial ischemia in the myocardium served by the left anterior descending and circumflex coronary arteries. The cause of death is thought to involve coronary vasospasm. What drug most likely precipitated this event?
a. Bromocriptine for Parkinson disease
b. Ergotamine given to abort a migraine attack
c. Morphine for post-trauma analgesia
d. Phenoxybenzamine used for carcinoid syndrome
e. Phenytoin to manage generalized tonic-clonic seizures
159. Promethazine, a phenothiazine derivative with substantial anti-emetic, antitussive, and H1-histamine receptor blocking activity, has a clinical profile quite similar to diphenhydramine. Recently the FDA mandated a “black box warning” for this widely used drug. The FDA now warns against use of the drug, in all doses and forms, for children aged 2 years or younger. Fatalities have occurred in these young patients, even in response to dosages that previously were considered therapeutic and safe. What is the most likely cause of death from promethazine in these patients?
a. Complete (third degree) heart block followed by asystole
b. Hypertensive crisis, intracranial hemorrhage
c. Parkinsonian-like dyskinesias, including tardive dyskinesias
d. Severe and refractory diarrhea leading to fluid and electrolyte loss
e. Ventilatory depression, apnea, excessive CNS depression
160. A 55-year-old undergoes surgery. She receives several drugs for pre-anesthesia care, intubation, and intraoperative skeletal muscle paralysis; and a mixture of inhaled and parenteral agents to provide balanced anesthesia. Toward the end of the procedure she develops a rapidly progressing fever, hypertension, hyperkalemia, tachycardia, muscle rigidity, and metabolic acidosis. Which drug combination is most likely to have elicited this reaction?
a. Fentanyl and midazolam
b. Midazolam and morphine
c. Nitrous oxide and etomidate
d. Propofol and midazolam
e. Succinylcholine and isoflurane
161. A 30-year-old woman with partial seizures is treated with vigabatrin. What is the specific mechanism of action of this GABA-related anticonvulsant?
a. Blocked neuronal reuptake of released GABA
b. Directly activated postsynaptic GABA receptors
c. Increased neuronal GABA release
d. Inhibited catabolism of released GABA
e. Stimulated neuronal GABA synthesis by acting as a metabolic precursor
162. A 24-year-old woman has a history of epilepsy that is being treated with phenytoin. She is healthy otherwise. She becomes pregnant. What would you do throughout the remainder of her pregnancy, in addition to providing otherwise proper perinatal care?
a. Add valproic acid
b. Discontinue all anticonvulsant medication
c. Increase daily dietary iron intake
d. Prescribe daily folic acid supplements
e. Switch from the phenytoin to phenobarbital
163. A patient is transported to the emergency department by ambulance after repeated episodes of fainting. The cause was attributed to severe drug-induced orthostatic hypotension due to α-adrenergic blockade from one of the drug’s main side effects. What drug was the most likely cause of this problem?
a. Buspirone
b. Chlorpromazine
c. Diphenhydramine
d. Haloperidol
e. Zolpidem
164. Clozapine, as an example of the “atypical antipsychotics,” seldom is used as first-line (initial) therapy of schizophrenia. Compared with the older “traditional” antipsychotics, it is associated with a much higher risk of a serious adverse response. What is that greater risk?
a. Agranulocytosis
b. Extrapyramidal side effects (parkinsonism)
c. Hypoglycemia
d. Hypotension, severe
e. Ventilatory depression or arrest
165. You’re at the end of the first week of your M3 ob-gyn clerkship. You are about to go into the delivery room to see your first childbirth. You’ve reviewed her chart and see that she was taking, for the duration of pregnancy, a drug that is not absolutely contraindicated in pregnancy (ie, not category X). You note that about 1 month before she was prescribed daily oral vitamin K supplements. The baby is born and promptly gets an injection of vitamin K. Knowing what you do about vitamin K, you correctly reason that these measures were taken to reduce the risks of excessive or abnormal bleeding, caused by drug-induced impairments of hepatic vitamin K-dependent clotting factors, in the newborn. What drug did the mother most likely receive during pregnancy, assuming that it was not in pregnancy category X?
a. Bupropion
b. Diazepam
c. Methadone
d. Phenytoin
e. Warfarin
166. When carbidopa is administered along with levodopa for Parkinson disease, we increase the bioavailability of levodopa by inhibiting the formation of dopamine in the gut. However, the carbidopa-induced inhibition of dopa decarboxylase favors the peripheral metabolism of levodopa to another metabolite that competes with levodopa for transport across the blood-brain barrier. This is catalyzed by catechol-O-methyltransferase (COMT). If your goal is to inhibit COMT, and so increase the central bio-availability and effects of levodopa, what drug would you choose?
a. Donepezil
b. Entacapone
c. Selegiline
d. Tacrine
e. Trihexyphenidyl
167. A patient has a long history of excessive alcohol consumption. He was arrested several times for drunk driving and was referred to a physician for therapy. The physician prescribed a drug to stifle further alcohol ingestion, to be used along with other interventions. The doctor properly instructed the patient not to consume any alcohol, not to use alcohol-containing mouthwashes, nor even apply alcohol-based toiletries, because alcohol may cause a disturbing, if not dangerous, interaction with his medication. The patient ignored the advice and decided to have a beer. Within minutes he develops flushing, a throbbing headache, nausea, and vomiting. Which drug was he most likely taking to curb his alcohol use?
a. Naltrexone
b. Diazepam
c. Disulfiram
d. Phenobarbital
e. Tranylcypromine
168. A patient with endogenous depression is started on a drug that selectively inhibits neuronal serotonin (5-HT) reuptake and has minimal effect on the reuptake of norepinephrine or dopamine. What drug best fits this description?
a. Amitryptyline
b. Bupropion
c. Fluoxetine
d. Imipramine
e. Venlafaxine
169. A 29-year-old man uses an oral benzodiazepine and alcohol to satisfy his addiction to CNS depressants. During the past week, he has been incarcerated and is not able to obtain the drugs. He is brought to the medical ward because of the onset of severe anxiety, increased sensitivity to light, dizziness, and generalized tremors due to drug withdrawal. On physical examination, he is hyperreflexic. Which drug would be the best choice to diminish his withdrawal symptoms?
a. Buspirone
b. Chloral hydrate
c. Chlorpromazine
d. Lorazepam
e. Trazodone
170. A 50-year-old man has been consuming large amounts of ethanol on an almost daily basis for many years. One day, unable to find any ethanol, he ingests a large amount of methanol (wood alcohol) that he had bought for his camp lantern. What drug would administer to best treat underlying biochemical consequences of the methanol poisoning?
a. Diazepam
b. Ethanol
c. Flumazenil
d. Phenobarbital
e. Phenytoin
171. Many news reports have told of a large number of deaths of opioid abusers who purchased and self-administered illicit drugs that contained lethal amounts of fentanyl. One patient who received this fentanyl-laced drug presents in your emergency department, barely alive. What drug would you administer first, with the best hope that it can promptly reverse the lethal effects of the fentanyl?
a. Diazepam
b. Flumazenil
c. Naloxone
d. Naltrexone
e. Phenytoin
172. A 10-year-old boy has nocturnal enuresis. His parents take him to a clinic that specializes in management of this condition. The physician writes an order for a low dose of imipramine. After a couple of weeks on the drug, the episodes of bed-wetting decrease dramatically. What is the most likely mechanism by which the imipramine provided benefit?
a. Alleviates depression signs and symptoms by increasing neuronal catecholamine reuptake
b. Blocks muscarinic receptors in the bladder musculature
c. Causes sedation such that the boy sleeps through the night without voiding
d. Reduces renal blood flow, glomerular filtration, and urine output
e. Releases antidiuretic hormone (ADH)
173. A patient is transported to your emergency department because of a seizure. A review of his history reveals that he has been treated by different physicians for different medical conditions, and there has been no dialog between them in terms of what they’ve prescribed. One physician prescribed a drug for short-term management of depression. Another prescribed the very same drug, marketed under a different trade name, to help the patient quit smoking cigarettes. What drug was most likely prescribed by both doctors, and was the most likely cause of the seizures?
a. Bupropion
b. Chlordiazepoxide
c. Fluoxetine
d. Imipramine
e. Lithium
174. About 1 year ago you diagnosed schizophrenia signs and symptoms in a 23-year-old otherwise healthy man. As a result of intensive psychotherapy, careful titration of chlorpromazine dosages, and remarkably good compliance on the patient’s part, he is well enough to return to work. Several months later, at a scheduled visit, you observe numerous signs and symptoms of drug-induced parkinsonism, and the patient reports rather distressing symptoms of akathisias (inner restlessness, jitteriness, etc). However, typical manifestations of schizophrenia seem to be well controlled. Which approach is most likely to alleviate the motor and subjective parkinsonian responses, and pose the lowest risk of causing schizophrenia signs and symptoms to reappear?
a. Add a catechol-O-methyltransferase inhibitor (eg, tolcapone)
b. Add a centrally acting cholinesterase inhibitor (eg, donepezil or tacrine)
c. Add benztropine
d. Add levodopa or levodopa plus carbidopa
e. Switch from chlorpromazine to haloperidol
175. A patient with Parkinson disease starts therapy with a drug that acts in the CNS as an agonist for dopamine receptors. It has no direct effects on dopamine synthesis, neuronal reuptake, or metabolic inactivation. What drug fits this description the best?
a. Amantadine
b. Apomorphine
c. Belladonna
d. Bromocriptine
e. Selegiline
176. A patient develops profound fever, skeletal muscle rigidity, and autonomic and systemic electrolyte imbalances as part of a severe adverse response to a psychoactive drug. The working diagnosis is neuroleptic malignant syndrome. In addition to administering dantrolene in an attempt to restore some semblance of normal skeletal muscle function, what other drug is most likely to be given to help provide additional symptom relief?
a. Benztropine
b. Bromocriptine
c. Diazepam
d. Flumazenil
e. Naloxone
f. Propranolol
177. A patient diagnosed with depression had been taking amitriptyline for several months. During a visit to his physician he reported difficulty sleeping, so the MD prescribed trazodone, to be taken once daily, at bedtime. The dosages of both the amitriptyline and the trazodone were clearly within the therapeutic range. Several weeks later the patient died. The attorney hired by the deceased man’s patient, as part of a wrongful death suit, contacted several “expert witnesses” who stated that the amitriptylinetrazodone combination caused a lethal serotonin syndrome. Based only on the information presented here, what is your most reasonable conclusion?
a. An interaction between trazodone and an SSRI, each at proper dosages, is unlikely to cause the serotonin syndrome.
b. The trazodone-SSRI combination is absolutely contraindicated, and should never have been prescribed.
c. Trazodone would be appropriate only if the patient were taking a monoamine oxidase (MAO) inhibitor or for depression.
d. Sumatriptan should have been prescribed to prevent the development of the serotonin syndrome.
e. Trazodone should never be prescribed to help patients go to sleep, whether or not they are depressed or are taking antidepressants.
Central Nervous System Pharmacology
Answers
106. The answer is b. Apologies for starting the chapter on CNS pharmacology with a question that definitely focuses on the autonomic nervous system. However, the question is helpful as yet another way to recognize the connections between ostensibly different areas of pharmacology and drug therapy. The description of guanfacine’s autonomic effects are extraordinarily similar to those of clonidine, which is generally considered the prototype of the “centrally acting antihypertensive drugs.” Clonidine and guanfacine act as postsynaptic α-adrenergic agonists (specifically, α2A; in the CNS, probably on prefrontal cortical neurons in terms of the effects on ADHD and anxiety; and in the medullary “cardiovascular control center” in terms of peripheral autonomic effects. Indeed, the overall “dialing-down” of sympathetic outflow, which accounts for guanfacine’s main autonomic action, also accounts for its much older use as an antihypertensive drug.
None of the responses described for guanfacine are qualitatively or mechanistically similar to those expected with atropine (a) or any other drug with strong muscarinic receptor blocking activity. Phentolamine (c), the prototype peripherally acting α1– and α2-adrenergic blocker, would cause miosis (by unmasking opposing parasympathetic influences on pupil size), although as described in the question it would have no effect on airway smooth muscle (which is affected by drugs that either work directly on β2 adrenergic, or muscarinic-cholinergic, receptors). And, unlike the situation with guanfacine or clonidine, phentolamine will markedly antagonize vasopressor effects of α-agonists such as phenylephrine. Finally, phentolamine would not cause falls of resting heart rate or stroke volume, since both of those functions are regulated by activation of β1-adrenergic receptors in various parts of the heart.
Prazosin (d) is a peripherally acting and selective α1 antagonist. Some of the effects of guanfacine are similar to those of prazosin, but there are three effects that were noted and that would argue against prazosin being the correct answer: (1) prazosin will indeed block the vasopressor responses to phenylephrine or any other drug that activates α-adrenergic receptors; (2, 3) it will not interfere with β-mediated increases of heart rate or stroke volume, whether mediated by the baroreceptor reflex or otherwise. In contrast, propranolol (d; or any other β-blocker that lacks vasodilator activity) would lower resting heart rate and also blunt baroreceptor-mediated increases of heart rate and stroke volume.
107. The answer is e. (Brunton, pp 466t, 527-560; Katzung, pp 40t, 373-381.) Benzodiazepines as a class tend to cause short-term memory loss following administration. The intensity of the effect depends on the unique drug (common and intense with midazolam, which has a fast onset and short half-life; and flunitrazepam [Rohypnol, known on the street mainly as “roofies”], for example), the drug’s pharmacokinetics, and the dose and administration route.
The memory loss does not affect recall of prior events but rather events occurring shortly after the drug is given. This antegrade amnesia is valuable in settings such as described in the scenario, where many unpleasant and anxiety-provoking events may occur between preop medication, the trip to the operating room, and other unpleasantries that might occur before the patient is anesthetized. (The patient here had absolutely no recall of events occurring within about 30 seconds after the midazolam was given, up to about an hour after she regained consciousness in the OR. Many patients who receive midazolam for endoscopic procedures such as colonoscopy or bronchoscopy also lack recall.)
Midazolam intensifies the overall sedative and mental clouding effects of opioids, but does not potentiate analgesia (a). It does not prevent or reverse hypotension (b), and if the dose is too large or it is administered too quickly, the drug may actually lower blood pressure in its own right. Midazolam has some anticonvulsant effects but it is seldom used for that purpose (lorazepam is one benzodiazepine that is routinely used for certain seizures, particularly status epilepticus). More importantly the question stated “…seizures likely to be caused by propofol,” but propofol rarely causes seizures (c). Benzodiazepines are not arrhythmogenic nor do they have antiarrhythmic activity (d).
108. The answer is a. (Brunton, pp 538t, 541-542; Katzung, pp 438-441.) Hypotension and respiratory/ventilatory depression is a common side effect with propofol and, indeed, with most other classes of CNS depressants injected for either anesthesia induction or maintenance. Laryngospasm (b) sometimes and rather uniquely applies to injection of rapidly acting barbiturate induction agents (see the next question). Memory loss (c)—specifically short-term antegrade amnesia—is associated with certain benzodiazepines (here, the midazolam, previous question).
Propofol does not cause malignant hyperthermia (d), or interact with other medications (those listed in the MAR, or others) to cause it. Malignant hyperthermia is mainly linked, in the surgical setting, to the combined use of a halogenated hydrocarbon inhaled anesthetic (particularly halothane, the use of which is declining) and a neuromuscular blocker (typically succinylcholine more so than a curare-like nondepolarizing agents). Propofol does not cause seizures (e); of the injectable induction agents, seizures are mainly a problem with etomidate. Finally, aside from generalized suppression of the CNS, propofol causes no significant or clinically relevant effects on skeletal muscle, and tends not to cause nausea or emesis (when used alone) that is common with other reasonable alternatives.
109. The answer is c. (Brunton, pp 539-540; Katzung, pp 441-442.) Laryngospasm is associated with the barbiturate IV induction agents, whether the drug is an oxybarbiturate (methohexital) or a thiobarbiturate (thiamylal, thiopental, others; “thio” refers to a sulfur atom replacing an oxygen atom at a certain point in the molecule). The mechanism is not known for sure, but the phenomenon is, and the laryngospasm may be sufficient in a small number of cases to make airway intubation difficult. The barbiturates also cause ventilatory depressant effects (centrally mediated), but in the situation described here that is not worrisome, because the patient is receiving mechanical ventilation.
Barbiturates lack analgesic effects (at blood levels not far lower than lethal). They can actually increase the sensation of pain (hyperalgesic effect, a) when therapeutic doses of oral agents (mainly phenobarbital nowadays) are given (inappropriately) to patients with pain and who are not being treated with true analgesic drugs suitable for the degree of pain the patient has. This is one of the reasons why barbiturates—and benzodiazepines for that matter—should never be used as analgesics. Note, however, that when the fast-acting injectable barbiturates are given at usual induction/anesthetic doses the hyperalgesic effect does not occur; in addition, this patient got other proper analgesics (morphine, ketorolac).
Barbiturates, whether given parenterally or orally, and regardless of their pharmacokinetics, tend to lower blood pressure (not raise it, answer b; the probable sites of action are both central and directly on the heart). Barbiturates used as IV induction agents tend to lower blood pressure significantly and sometimes excessively. Malignant hyperthermia (d) is a serious adverse perioperative response that is associated with the combined administration of skeletal neuromuscular blockers (typically succinylcho-line) and certain inhaled halogenated hydrocarbon anesthetics (eg, halothane). Barbiturates do not interact or cause malignant hyperthermia in their own right. All the barbiturates have anticonvulsant activity (dose-dependent and also dependent on which barbiturate is being used), and they do not cause myoclonus or other types of seizures (e). The higher risk of myoclonic seizures is mainly associated with etomidate, which is another IV induction agent. (Etomidate-induced seizure risk can be reduced by premedication with an opioid or a benzodiazepine.)
110. The answer is b. (Brunton, pp 529, 967t, 986; Katzung, pp 638t, 642, 655.) Although ketorolac is usually presented in a chapter on NSAIDs, it has very weak (and not clinically useful) anti-inflammatory activity. However, it provides excellent analgesia that has been described as equivalent to that provided by usual starting doses of an opioid (eg, morphine) when pain is “moderate” and relatively short lived. The mechanism probably involves inhibited prostaglandin synthesis (as with all NSAIDs) and does not involve activation of any opioid receptors. The drug has no antiemetic effects (a); does not affect ventilatory rate or depth (c); has no effect on skeletal neuromuscular transmission or the effects of neuromuscular blockers (d). Unlike most opioids, ketorolac also lacks adverse effects on the biliary tract, usually making it a good choice for patients with nephrolithiasis or other conditions that trigger gall bladder/bile duct spasm and pain.
Ketorolac is not suitable, alone, for severe pain (when an opioid truly is indicated) nor for chronic pain. In surgical settings such as the one described here it is used as a supplement to an opioid. What are the advantages of ketorolac, whether used alone or as a supplement, compared with an opioid? Ketorolac’s analgesia is not accompanied by typical opioid-like ventilatory depression; hypotension; sedation, mental clouding or euphoria; nor a potential for dependence or abuse. It is often used as an opioid supplement precisely because the main alternative approach—simply giving a higher dose of morphine—could lead to excessive ventilatory depression and hypotension.
Despite the relative lack of anti-inflammatory activity, the main adverse responses to ketorolac are similar to those of traditional NSAIDs on the GI tract: the potential for gastric ulceration, potentially with GI bleeding or hemorrhage; for renal impairment; and for prolonged bleeding due to antiplatelet effects (weak and not therapeutically useful). These adverse effects are most likely to occur with long-term use, which is why ketorolac should be used only for short-term pain control (no more than 5 days). Most of the contraindications that apply to traditional NSAIDs apply to ketorolac, for example, peptic ulcer disease (active or a risk thereof); renal dysfunction; active bleeding (especially intracranial); pregnancy; and prior hypersensitivity.
Notes: You should know about ketorolac because it is used widely in general surgical settings such as described in the question; in orthopedics; and in oral surgery and other settings where “good” short-term analgesia is needed and it is best to minimize or avoid other unwanted effects of opioids.
When ketorolac was first approved, many practitioners used it frequently and prescribed it for chronic pain control. (Some described prescribing the drug “like candy.” After all, it provided excellent pain control with no opioid-like problems.) Not long thereafter prescribers realized the strong ulcerogenic actions of the drug, and so new guidelines and warnings were made to restrict use of the drug to no more than several days in a row.
111. The answer is e. (Brunton, pp 1341-1343; Katzung, pp 287, 1098-1099.) Ondansetron, like a related drug, dronabinol, is used to manage drug-induced nausea and vomiting that can occur postoperatively or in response to emetogenic drugs (eg, many anticancer drugs). It is a serotonin receptor (5-HT3) blocker that acts mainly in the medullary chemoreceptor trigger zone and on vagal afferents (inhibited) to parts of the upper GI tract.
Ondansetron has no general CNS or cortical stimulating effects that would help restore consciousness, alertness, or awareness of time and place (a); no analgesic-intensifying effects (b); no significant effects on the bladder (c); and does not reduce the risk of paralytic ileus (d) because vagal tone to intestinal smooth muscles is suppressed.
112. The answer is d. (Brunton, pp 540-542, 546-547; Katzung, pp 431-436.) MAC (minimum alveolar concentration) is an expression of inhaled anesthetic “potency.” It is defined as the minimum inspired concentration needed to abolish a specified painful response in 50% of treated patients. (Thus, it is much like the ED50, measured in a population dose-response curve, for most other drugs.) Obviously, giving a drug at a dose that suppresses a response in only half the treated patients is not desirable, so inhaled anesthetics are typically given at a dose more than the MAC. (Recall, too, that MAC is not absolute: it can change depending on the use of other anesthesia adjuncts and such other factors as body temperature, ventilatory rate, presence of other diseases, etc.)
A drug’s MAC gives us no useful and invariable information about onsets or durations of action (a, e). You cannot state correctly that drug Y (MAC ≈ 100%) causes greater analgesia and/or skeletal muscle relaxation than another drug any more than we can say that a drug with an ED50 of 5 mg causes a greater response than one with an ED50 of 1 mg. It all depends on the dose given, not the MAC or ED50.
113. The answer is d. (Brunton, pp 398, 408, 614t, 618; Katzung, pp 488f, 490, 499.) Two of the important types of MAO are: (1) MAO-A, which metabolizes norepinephrine and serotonin and other biogenic amines, and is the predominant hepatic form of the enzyme; and (2) MAO-B, which metabolizes dopamine and other monoamines in the brain. Selegiline is a selective inhibitor of MAO-B. It therefore inhibits the breakdown of dopa-mine and prolongs the therapeutic effectiveness of levodopa (endogenous or that provided pharmacologically) in parkinsonism. The risks of serious drug interactions in patients taking nonselective MAO inhibitors (eg, phenelzine, tranylcypromine), such as hypertensive crisis in response to mixed- and indirect-acting sympathomimetics (tyramine, pseudoephedrine, and amphetamines) are much less (but still possible) with selegiline.
Bromocriptine (a) is a dopamine receptor agonist. Carbidopa (b) inhibits the peripheral metabolism of levodopa by DOPA decarboxylase. Both are useful in the treatment of some cases of idiopathic (but not antipsychotic drug-induced) parkinsonism. Phenelzine (c) and tranylcypromine (e) are nonselective MAOIs. Combining them with L-dopa may lead to a potentially fatal hypertensive crisis, and thus they are not used in the therapy of parkinsonism. A similar interaction may occur with tyramine-rich foods and beverages; and with catecholamine-releasing sympathomimetics (ephedrine, pseudoephedrine, amphetamines, and amphetamine-like drugs). As a result of these common and potentially lethal interactions, non-selective MAO inhibitors are rarely used for anything unless no other usually effective therapies work adequately or are otherwise contraindicated.
114. The answer is d. (Brunton, pp 536-537, 614t; Katzung, pp 485, 499.) When levodopa is administered orally, the vast majority of the administered dose (about 90%) is metabolized in the gut to dopamine by DOPA decarboxylase. However dopamine cannot cross the blood-brain barrier, and so only a fraction of the parent drug gets into the CNS, to be metabolized and cause its desired effects there. Carbidopa inhibits DOPA decarboxylase in the periphery, reducing peripheral metabolism of levodopa to dopamine and “sparing” a bigger fraction of the administered levodopa dose so it can be metabolized in the nigrostriatum. By reducing peripheral conversion of levodopa to dopamine, the adjunctive use of carbidopa often enables management of parkinsonian signs and symptoms with doses of levodopa much lower than would be needed in the absence of carbidopa. One additional benefit of that is a reduction in the number and severity of peripheral side effects of the levodopa (or, more precisely, its metabolite, dopamine).
Adding carbidopa to a regimen involving levodopa only may also help (at least transiently) combat such problems as dopamine’s “on-off phenomenon” and “end-of-dosefailure.” The on-off phenomenon is characterized by frequent, abrupt, and dramatic changes between what appears to be good symptom control to episodes that look like parkinsonian signs and symptoms weren’t improved at all (much like what happens when switching the lights on and off). With end-of-dose failure, symptom control between doses gets progressively less progressively sooner. For example, a patient who had good symptom control up to an hour or so before the next scheduled levodopa dose may gradually experience loss of that control 2 hours, 3 hours, or even much more, before they were to take their next dose.
Carbidopa, whether considered in its own right or in the context of coadministration with levodopa has no effects (inhibitory or stimulatory) on ACh release (a). Vitamin B6 deficiencies of the vitamin do not occur in response to therapy with either or both drugs (b); and it is important to note that ingesting large amounts of that vitamin, whether as part of the diet or in the form of supplements, will antagonize the desired effects of levodopa with or without added carbidopa. Carbidopa does give “better access” of levodopa to the CNS, but that effect has nothing to do with increasing blood-brain barrier permeability to dopamine (c). It is due, as noted, to increased concentrations of levodopa in the circulation due to inhibited peripheral conversion to dopamine. Carbidopa has no beneficial effects on dopamine-induced blood pressure changes, and has no ability to block dopamine receptors in the vasculature (e) or anywhere else.
115. The answer is e. (Brunton, p 349; Katzung, pp 283-285, 374, 376, 387.) Buspirone is an attractive drug for managing mild short-term anxiety. Among the reasons (and especially when compared with more traditional anxiolytics, such as benzodiazepines) are a lack of sedation (buspirone is not a CNS depressant); very little (if any) potentiation of the effects of other CNS depressants, including alcohol; no known abuse potential (it is not regulated by the Controlled Substances Act) or tendency for development of tolerance; and no major withdrawal syndrome. One major drawback is a slow onset of symptom relief (a week or two), and typically it takes about a month from the onset of therapy for antianxiety effects to stabilize. (Knowing this slow onset, one should resist the temptation to titrate the dosage upward, to hasten or increase the drug’s effects, prematurely.)
You should recall that long-term benzodiazepine administration is associated with withdrawal phenomena (and, depending on the use, dose, exact drug, and other patient-related factors, the syndrome can be severe). Thus, one can envisage a switch from a benzodiazepine to buspirone. Because buspirone lacks CNS depressant effects and its effects take some time to develop, one should start the buspirone several weeks before stopping the benzodiazepine and then taper the benzodiazepine dose once it’s time to stop the drug.
116. The answer is c. (Brunton, pp 593-594; Katzung, p 411.) Phenobarbital’s role in the primary management of all of the named conditions has waned dramatically, and appropriately, as newer drugs, with fewer risks of drug interactions and tolerance development, have come on the market. The only use in the options provided in the question, for which phenobarbital is still considered reasonable for long-term therapy in some patients, is for managing certain epilepsies (mainly as an alternative to phenytoin). The seizure types include, mainly, partial seizures and generalized tonic-clonic seizures. Benzodiazepines are almost always preferred, and used, for managing alcohol withdrawal (a) and therapy of anxiety (b). Benzodiazepines, or the benzodiazepine-like agents zaleplon or zolpidem, are almost always turned to for insomnia (e). Phenobarbital—and other barbiturates for that matter—have no beneficial effects on depression signs and symptoms (d), and they are not properly used alone or in combination with an SSRI (or tricyclic or atypical antidepressant).
Major reasons for selecting a benzodiazepine over a barbiturate include fewer drug-drug interactions (phenobarbital is a classic P450 inducer that hastens the elimination of many other drugs that are metabolized by the P450 system); a lesser risk of generalized risk of CNS depression (somnolence, etc); lower risk of dependence; withdrawal syndromes that are typically less severe or dangerous; lower risk of fatal ventilatory depression with oral overdoses (and the availability of flumazenil, the specific benzodiaze-pine antagonist, to treat them); and less narrowing between lethal and effective doses (better therapeutic index or margin of safety) as use continues.
Note that even though benzodiazepines may be preferred, treatment for such problems as anxiety and insomnia should be kept as short as possible.
117. The answer is a. (Brunton, pp 225-235, 400-403; Katzung, pp 526-527, 531-534, 536-537.) The most common side effects associated with tri-cyclic antidepressants are their antimuscarinic effects, which may occur and often be prominent in over 50% of patients. Clinically, these effects may manifest as dry mouth, blurred vision, constipation, tachycardia, dizziness, and urinary retention. These are, of course, some of the typical and common side effects associated with atropine or any other drug with substantial antimuscarinic effects. At therapeutic plasma concentrations these drugs usually do not cause changes in the ECG (b)—but with severe overdoses lethal arrhythmias often do occur. These drugs are not particularly hepatotoxic or nephrotoxic (c, d); seizures are not likely to occur unless the patient has a history of seizure disorders or massive overdoses have been taken.
Note: In terms of tricyclic toxicity, ie, with overdoses, you might want to recall what some students learn as the “Three Cs:” coma, cardiotoxicity (mainly arrhythmias that are often difficult to treat), and convulsions. In addition, all the other manifestations of “atropine poisoning” will develop and usually be severe. This is an extremely difficult situation to treat, and to treat successfully, when the cause is a tricyclic antidepressant.
118. The answer is b. (Brunton, pp 356-357, 611, 614t; Katzung, pp 501-520.) Unwanted extrapyramidal side effects produced by antipsychotic drugs (eg, chlorpromazine, as the exemplar of the phenothiazines; and, more so, by haloperidol as the prototype of the butyrophenones) include Parkinson-like syndrome, akathisia, dystonias, galactorrhea, amenorrhea, and infertility. These side effects are due to the ability of these agents to block dopamine receptors. The phenothiazines also block muscarinic and α-adrenergic receptors, which are responsible for other effects in both the CNS and (especially) in the periphery. The incidence and severity of these autonomic side effects is much greater with low-potency antipsychotics (eg, chlorpromazine and other phenothiazines) than with the high-potency butyrophenones (eg, haloperidol).
119. The answer is b. (Brunton, pp 542-544; Katzung, pp 444-446, 550.) The scenario describes most of the classic responses to ketamine, a “dissociative anesthetic”: analgesia; an ostensibly light sleep-like state; a trancelike and cataplectic state (including increased muscle tone); and activation of most cardiovascular/hemodynamic parameters. The various psychosis-like emergence reactions are the main disadvantages to using a drug that, otherwise, causes many of the desired elements of balanced anesthesia, usually without the need for complicated and expensive anesthesia administration devices or personnel. Ketamine undergoes significant metabolism in humans, with about 20% of the absorbed dose recovered as metabolites. The only other drug listed that provides adequate analgesia is fentanyl (a). Midazolam (c; benzodiazepine), succinylcholine (d; depolarizing neuro-muscular blocker), and thiopental (e; thiobarbiturate) lack analgesic activity; moreover, if any cardiovascular or autonomic changes were to occur in response to any of those drugs, they would be better characterized as depression, not activation.
120. The answer is b. (Brunton, pp 591-593, 845, 1012, 1524, 1528, 1873t; Katzung, pp 40t, 407-409, 427.) The hepatic enzymes responsible for phenytoin metabolism (mainly CYP2C9) become saturated at plasma drug concentrations above approximately 10 to 15 mcg/mL, which are clearly within the typical therapeutic range yet well below maximum or peak therapeutic levels. At daily dosages associated with or below those 10 to 15 mcg/mL values, dose increases give relatively proportional increases in plasma drug concentrations, and phenytoin elimination follows usual first-order kinetics (a constant fraction of drug is eliminated with the passing of each half-life). Once the metabolic capacity is exceeded (as it has in our patient, which may arise with intentional or inadvertent increases in the daily dose), small increases in dosage lead to disproportionately large increases of plasma concentrations (and effects) because, in essence, “drug in greatly exceeds drug out:” zero-order kinetics now describes the drug’s elimination, such that a constant amount (not fraction) of drug is eliminated per unit time. Therefore, the first-order half-life does not apply; elimination is slower, and the plasma concentration will be much greater than 15 mcg/mL (half of 30 mcg/mL; ans. e) 24 hours after the initial blood sample is taken.
The figure below shows an approximation of the relationship between plasma phenytoin levels and daily doses (the placement of the curve can vary from patient to patient along the x-axis). From the rapid rise in the curve at dosages above about 300 mg/day you can deduce a significant reduction of clearance rates owing to slowed metabolism (since metabolism is the main pathway for phenytoin’s elimination).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree