37. Anatomic, neurochemical, and pharmacologic studies of nerves a, c, e, f, and h indicate that they share one common property. Which statement below correctly summarizes what that is?
a. Are cholinergic, activate postsynaptic muscarinic receptors
b. Are cholinergic, activate postsynaptic nicotinic receptors
c. Cannot release their neurotransmitter(s) in the presence of atropine
d. Have the ability to activate all the adrenergic and all the cholinergic nerves
e. Recycle their neurotransmitter after each action potential, rather than synthesizing new transmitter de novo
38. Multidisciplinary assessments of nerve d, a “typical” postganglionic sympathetic nerve, indicate that it is quite different from all the other nerves shown in the peripheral nervous system schematic. Which statement describes that difference?
a. Atropine selectively blocks activation of receptors by the neurotransmitter released from nerve d
b. It causes bronchodilation (airway smooth muscle relaxation) when it is activated
c. It is adrenergic (or noradrenergic if you wish to use that term instead)
d. The primary neurotransmitter synthesized by nerve d is epinephrine
e. When nerve d is physiologically activated by an action potential, actions of its released neurotransmitter are terminated mainly by hydrolysis in the synaptic cleft
39. Reuptake (into the nerve) is the main physiologic process for terminating the postsynaptic activity of a peripheral nervous system neurotransmitter. To which nerve does this process apply?
a. Nerve a
b. Nerve b
c. Nerve c
d. Nerve d
e. Nerve e
f. Nerve f
g. Nerve g
h. Nerve h
40. Nerve d, the more typical postganglionic sympathetic nerve, is activated by a normally generated action potential followed by neurotransmitter release into the synapse. On which receptor type does the neurotransmitter it releases act? Remember: You can select only one answer.
a. α1 adrenergic
b. α2 adrenergic
c. β1 adrenergic
d. β2 adrenergic
e. Muscarinic
f. Nicotinic
g. It depends on the target tissue (effector) type
41. Which statement correctly describes what is rather unique about nerve g, the postganglionic fibers that innervate eccrine sweat glands, compared with virtually all other postganglionic sympathetic nerves?
a. Cocaine blocks release of its neurotransmitter
b. Is cholinergic
c. Is stimulated by preganglionic adrenergic nerves (nerve f)
d. Its released neurotransmitter acts on nicotinic receptors
e. Uses epinephrine as its neurotransmitter
42. Nerve g, the postganglionic nerve innervating eccrine sweat glands and arrector pili muscles, is activated by a normally generated action potential and subsequent release of neurotransmitter from nerve f. On which receptor type does the neurotransmitter released by nerve g act?
a. α1 adrenergic
b. α2 adrenergic
c. Muscarinic
d. Nicotinic
e. β1 adrenergic
f. β2 adrenergic
43. Assume that all the efferent autonomic pathways in the schematic are tonically active (a reasonable assumption), even if at low and quantitatively different levels. We add vecuronium (or any of several related drugs) to the system and, as expected, it blocks neurotransmitter activation of certain structures. Which nerve innervates those structures and normally would activate them in the absence of pancuronium or its related drugs?
a. Nerve a
b. Nerve b
c. Nerve c
d. Nerve d
e. Nerve e
f. Nerve f
g. Nerve g
h. Nerve h
44. Nearly every structure that is influenced by sympathetic nervous system activity has postganglionic sympathetic (adrenergic) nerves innervating it. Which one of the following structures is most definitely affected by sympathetic nervous system influences, and responds to epinephrine, but lacks innervation by postganglionic adrenergic fibers and so is not affected by norepinephrine released from adrenergic nerves?
a. Airway (eg, bronchiolar) smooth muscle
b. Arteriolar smooth muscle
c. Iris dilator muscles of the eyes
d. Sinoatrial cells (pacemaker) of the heart
e. Ventricular myocytes
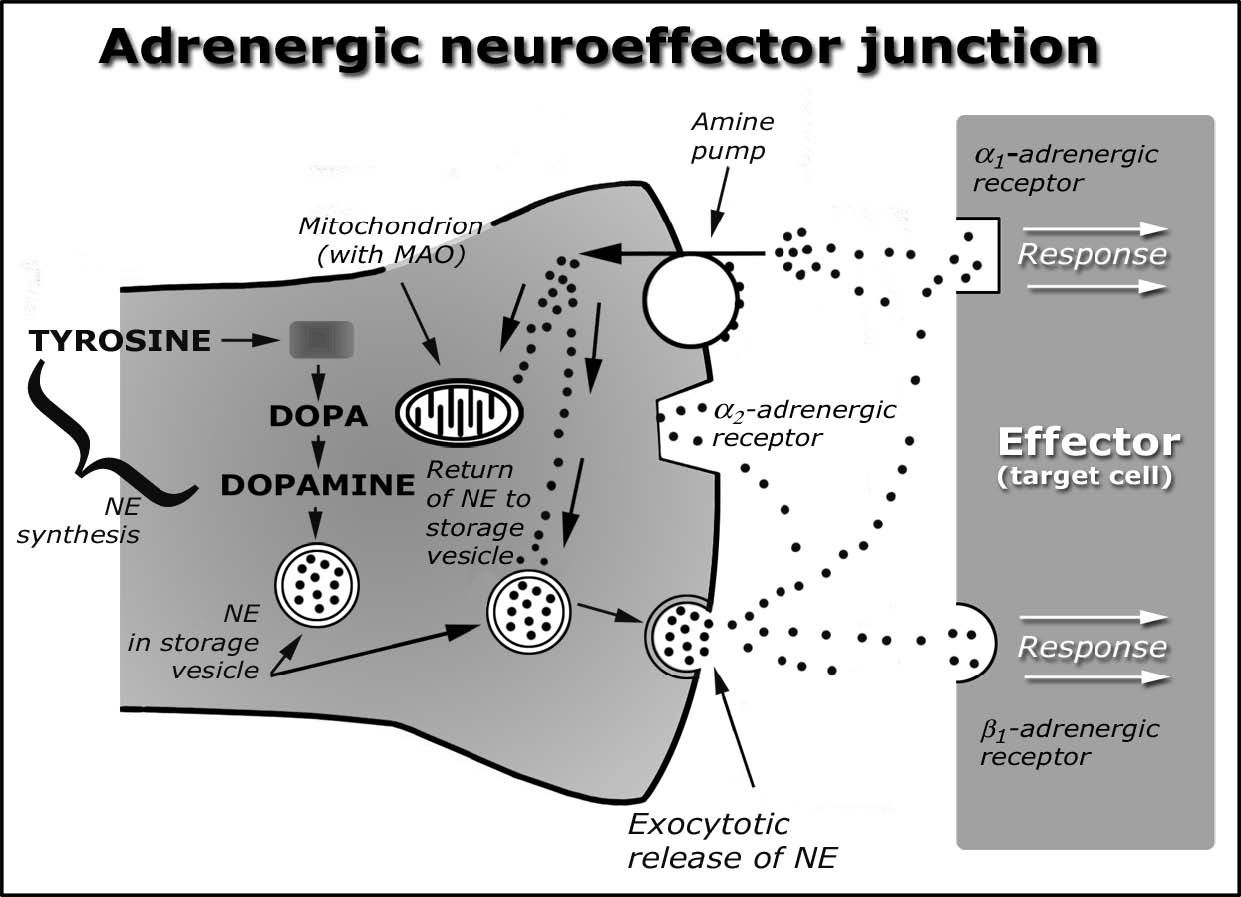
The figure below shows some of the main elements of norepinephrine (NE) synthesis, release, actions, and other steps in adrenergic neurotransmission. You do not need the diagram to answer this series of questions, but seeing it may aid your answering or reviewing. Note that the effector (target) cell on the far right has either an α-adrenergic receptor or a β-adrenergic receptor.
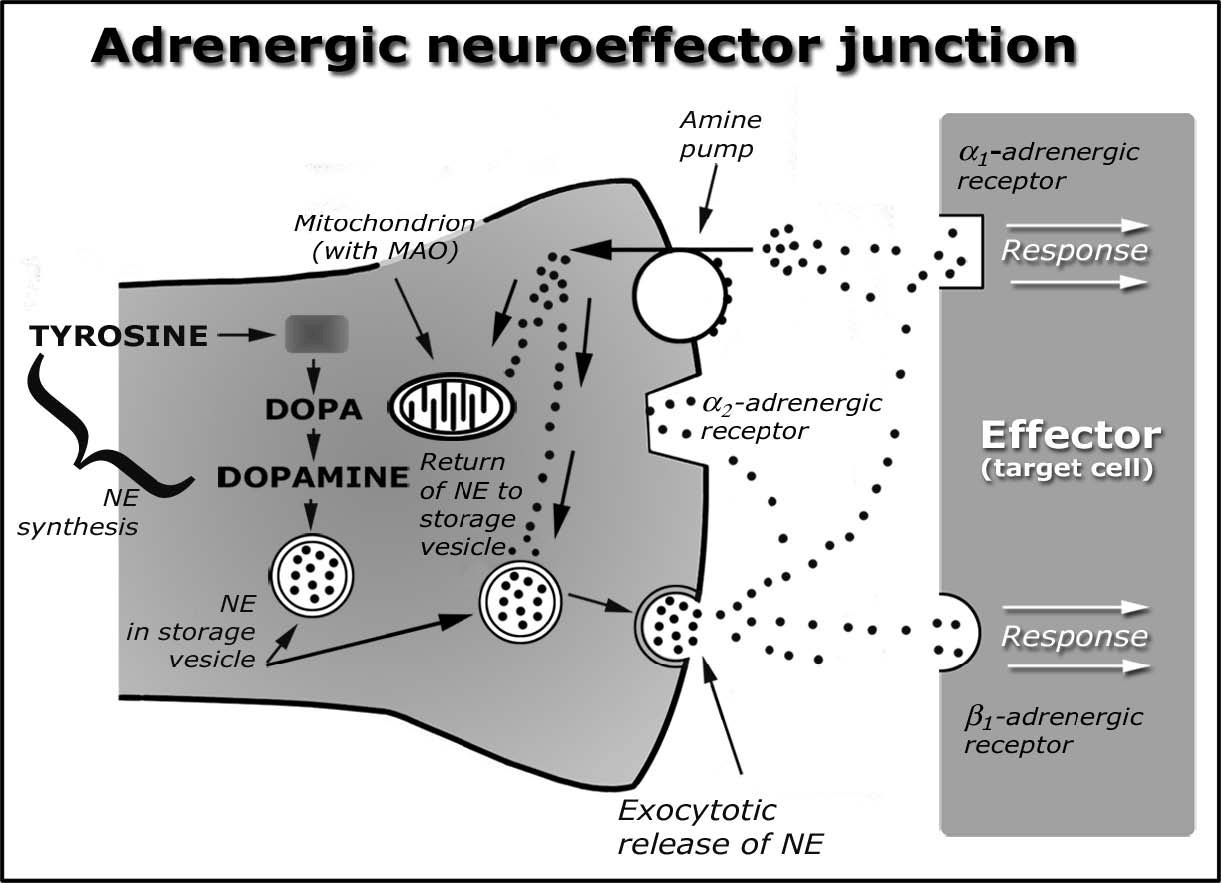
45. Mitochondria in the terminus of adrenergic nerve “endings” contain an abundance of monoamine oxidase (MAO). What best summarizes the biological role of the MAO in these adrenergic nerves?
a. Drives storage vesicles that contain norepinephrine to the nerve “ending” so that exocytotic norepinephrine release can occur in response to an action potential
b. Metabolically degrades NE that is free (not stored in vesicles) in the nerve terminal
c. Metabolizes dopamine to norepinephrine
d. Provides metabolic energy for nonexocytotic release of norepinephrine in response to amphetamines and other catecholamine-releasing drugs
e. Synthesizes ATP that is required to transport free intraneuronal norepinephrine into the storage granules/vesicles
46. Many studies have shown that a large fraction of norepinephrine (NE) in the normal resting adrenergic neuron is stored in membrane-bound vesicles or granules. We administer a drug that, over time, depletes this supply of neurotransmitter and decreases the intensity of responses to sympathetic nerve activation. In vitro studies reveal that the drug acts by inhibiting uptake of intraneuronal NE into the vesicles; it has no direct effect on catecholamine synthesis, release, or interactions with its receptors. Which drug fits this description best?
a. Pargyline
b. Prazosin
c. Propranolol
d. Reserpine
e. Tyramine
47. A substance abuser self-administers cocaine and experiences a variety of significant changes in cardiovascular function, in addition to the CNS-stimulating effects for which the drug was used. What statement describes the mechanism by which the cocaine caused its main peripheral and CNS effects?
a. Activates α2-adrenergic receptors leading to increased NE release
b. Blocks NE (and dopamine, in the CNS) reuptake via the amine pump
c. Directly activates postsynaptic α- and β-adrenergic receptors, leading to sym-pathomimetic (adrenomimetic) responses
d. Inhibits MAO, leading to increased intraneuronal NE levels
e. Prevents NE exocytosis
48. We administer a drug that is a selective antagonist at the presynaptic α-receptors (α2) in the peripheral nervous systems. It has no effect on α1 receptors, β receptors, or any other ligand receptors that are important in peripheral nervous system function. What is the main response that is likely to occur following administration of the α2 -blocker?
a. Activation of the amine pump, stimulation of norepinephrine reuptake
b. Inhibition of dopamine β-hydroxylase, the enzyme that converts intraneuronal dopamine to norepinephrine
c. Increased norepinephrine release in response to each action potential
d. Inhibition of norepinephrine exocytosis
e. Stimulation of intraneuronal monoamine oxidase activity
49. Not shown in the diagram is an enzyme that has the ability to metabolically inactivate NE that has diffused away from the synapse. It is also present in the liver (as is MAO) and in the intestinal walls. Among other things, the rapidity with which this enzyme catabolizes its substrates accounts for why norepinephrine, dopamine, and dobutamine have extraordinarily short half-lives, must be given intravenously in order to cause meaningful effects, have negligible effects when given by other parenteral routes, and are ineffective when given by mouth. An inhibitor of this drug is used therapeutically, but not for its autonomic effects. What is the name of this enzyme?
a. Aromatic L-amino acid decarboxylase
b. Catechol O-methyltransferase (COMT)
c. Dopamine β-hydroxylase
d. Phenylethanolamine N-methyltransferase
e. Tyrosine hydroxylase
50. We administer a therapeutic dose of a drug that selectively and competitively blocks the postsynaptic α-adrenergic (α1) receptors. It has no effects on presynaptic α-adrenergic receptors (α2) or β-adrenergic receptors found anywhere in the periphery, whether as an agonist or antagonist. What is the most likely drug?
a. Clonidine
b. Phentolamine
c. Phenoxybenzamine
d. Phenylephrine
e. Prazosin
51. Festoterodine is a relatively new drug that was heavily marketed to prescribers and directly to consumers. It is indicated for the treatment of an overactive urinary bladder, reducing the symptoms of urge incontinence, urinary urgency, and urinary frequency. It prevents physiologic activation of the bladder’s detrusor and simultaneously prevents relaxation of the sphincter. Side effects include constipation, dry mouth, blurred vision, photophobia, urinary retention, and slight increases in heart rate. Another advisory for the drug: “Heat stroke and fever due to decreased sweating in hot temperatures have been reported.” Festoterodine has no direct effects on blood vessels that might change blood pressure. Based on this information, what prototype drug is most like festoterodine?
a. Atropine
b. β-adrenergic blockers (eg, propranolol)
c. Isoproterenol
d. Neostigmine
e. Phentolamine
52. A morbidly obese person visits the local bariatric (weight loss) clinic seeking a pill that will help shed weight. The physician prescribes dextroamphetamine. In addition to causing its expected centrally mediated anorexigenic (appetite-suppressant) and cortical-stimulating effects it causes a host of peripheral adrenergic effects that, for some patients, can prove fatal. What best summarizes the main mechanism by which dextroamphetamine, or amphetamines in general, cause their peripheral autonomic effects?
a. Activates MAO
b. Blocks NE reuptake via the amine pump/transporter
c. Displaces, releases, intraneuronal NE
d. Enhances NE synthesis, leading to massive neurotransmitter overproduction
e. Stabilizes the adrenergic nerve ending by directly activating α2 receptors
53. We administer a pharmacologic dose of epinephrine and observe (among other responses) a direct increase of cardiac rate, contractility, and electrical impulse conduction rates. Which adrenergic receptor was responsible for these direct cardiac effects?
a. α1
b. α2
c. β1
d. β2
e. β3a
54. A patient with a history of narrow-angle (angle-closure) glaucoma experiences a sudden rise of intraocular pressure that is sufficiently severe. In addition to pain there is an imminent risk of permanent vision loss. They require immediate treatment, one element of which is administration of echothiophate. What enzyme is affected by this autonomic drug?
a. Tyrosine hydroxylase—stimulated
b. Acetylcholinesterase (AChE)—inhibited
c. Catechol-O-methyltransferase (COMT)—inhibited
d. Monoamine oxidase (MAO)—stimulated
e. DOPA decarboxylase—stimulated
55. A patient has essential hypertension, and lab tests would show that their circulating catecholamine and plasma renin levels are unusually high. The chosen therapeutic approach for this patient is to give a single drug that blocks both α- and β-adrenergic receptors, thereby reducing blood pressure by reducing both cardiac output and total peripheral resistance (systemic vascular resistance). What drug is most capable of doing that?
a. Labetalol
b. Metoprolol
c. Nadolol
d. Pindolol
e. Timolol
56. A man who has been “surfing the Web” in search of an aphrodisiac or some other agent to enhance “sexual prowess and performance” discovers yohimbine. He consumes the drug in excess and develops symptoms of toxicity that require your intervention. You consult your preferred drug reference and learn that yohimbine is a selective α2-adrenergic antagonist that acts mainly in the brain’s medullary “cardiovascular control center.” What would you expect as a response to this drug?
a. Bradycardia
b. Bronchoconstriction
c. Excessive secretions by exocrine glands (salivary, lacrimal, etc)
d. Reduced cardiac output from reduced left ventricular contractility
e. Rise of blood pressure
57. You plan to prescribe scopolamine, as a transdermal drug delivery system (skin patch), for a patient who will be leaving for an expensive cruise and is very susceptible to motion sickness. What comorbidity would weigh against prescribing the drug because it is most likely to pose adverse effects—or be truly contraindicated?
a. Angle-closure (narrow-angle) glaucoma
b. Bradycardia
c. History of allergic reactions to uncooked shellfish
d. Resting blood pressure of 112/70
e. Hypothyroidism, mild
f. Parkinson disease (early onset, not currently treated)
58. A child overdoses on a drug that affects both the autonomic and somatic nervous systems. As blood levels of the drug rise he experiences hypertension and tachycardia, accompanied by skeletal muscle tremor. Further elevations of blood levels of the drug cause all the expected signs and symptoms of autonomic ganglionic blockade, plus weakness and eventual paralysis of skeletal muscle. Which drug did the child most likely ingest?
a. Bethanechol
b. Nicotine
c. Pilocarpine
d. Propranolol (or another β-adrenergic blocker)
e. Scopolamine
59. Many clinical studies have shown that propranolol will lower blood pressure to varying degrees in nearly every patient with essential hypertension (ie, high BP of unknown etiology or identifiable causes, such as pheochromocytoma or vasopressor drug overdose). What is the most likely and physiologically most important mechanism for propranolol’s pressure-lowering effect?
a. Induced a baroreceptor reflex that reduces vasoconstriction usually caused by activation of the sympathetic nervous system
b. Inhibited catecholamine release from adrenergic nerves and the adrenal medulla (suprarenal medulla)
c. Reduced heart rate and left ventricular contractility
d. Reduced total peripheral resistance via direct vasodilator actions involving nitric oxide synthesis in endothelial cells
e. Stimulated renin release, ultimately leading to enhanced synthesis of vasodilator chemicals such as bradykinin
60. A 35-year-old man who weighs 150 pounds and is 5 feet 10 inches tall is transported to the emergency department in severe distress. He complains of episodes of severe, throbbing headaches, profuse diaphoresis, and palpitations. Eighteen months ago his physician told him he is healthy except for essential hypertension, but he refused medication and has not seen a health care provider for the last year and a half. He denies use of any drugs, whether prescription or over-the-counter, legal or otherwise.
Assessment reveals that he is tachycardic and has an irregular pulse (occasional premature ventricular beats are noted on his ECG). Heart rate at rest is approximately 130 beats/min, sometimes more. His resting blood pressure is 200/140 mm Hg. These cardiovascular findings are shown in the figure below.
The first year house officer who is caring for this patient knows that all the orally effective β-adrenergic blockers are approved for use to treat essential hypertension, and concludes that prompt lowering of blood pressure is essential for this patient. Therefore, he orders intravenous administration of propranolol (at the arrow, above), and a large dose of the drug since the symptoms seem severe. Unknown to the physician is the fact that the patient’s signs and symptoms are due to a pheochromocytoma (epinephrine-secreting tumor of the adrenal/suprarenal medulla).
What is the most likely ultimate outcome of administering this β-blocker (or any other β-blocker that lacks α-blocking or other vasodilator activity), supplemented with no other medication?
a. Heart failure, cardiogenic shock, death
b. Long-lasting normalization of heart rate, contractility, and blood pressure
c. Normalization of blood pressures but persistence of tachycardia
d. Restoration of normal sinus rate and rhythm, but no change of blood pressure from predrug levels
e. Sudden and significant rise of systolic blood pressure and heart rate
61. A patient with chronic obstructive pulmonary disease (COPD, eg, emphysema, chronic bronchitis) is receiving an orally inhaled muscarinic receptor-blocking drug to maintain bronchodilation. What drug belongs to that class?
a. Albuterol
b. Diphenhydramine
c. Ipratropium (or tiotropium)
d. Pilocarpine
e. Vecuronium
62. You give an “effective dose” of atropine to a person who was poisoned with an AChE inhibitor. What structure will continue to be overactivated by the excess ACh after the atropine is given?
a. Airway smooth muscle
b. S-A node of the heart
c. Salivary and lacrimal glands
d. Skeletal muscle
e. Vascular smooth muscle
63. The house officer considers prescribing nadolol for a 53-year-old patient. What preexisting condition (comorbidity) would most likely contraindicate safe use of this drug?
a. Angina pectoris, chronic-stable (effort-induced)
b. Asthma
c. Essential hypertension
d. Heart failure, mild
e. Sinus tachycardia
64. A variety of ophthalmic drugs, working by several main mechanisms of action, are useful for managing chronic open-angle glaucoma. Which one reduces intraocular pressure by decreasing the formation of aqueous humor, rather than by changing the size of the pupil(s)?
a. Echothiophate
b. Isoflurophate
c. Neostigmine
d. Pilocarpine
e. Timolol
65. It’s fair to say that epinephrine, norepinephrine, and acetylcholine play the most important roles as endogenous agonists for the various receptors under control of the peripheral nervous systems. However, dopamine also plays a small but important therapeutic role, particularly when administered IV at low doses. What other peripheral effects can dopamine cause at usual therapeutic doses?
a. Bronchodilation via relaxation of airway smooth muscles
b. Direct activation of pressure receptors (eg, baroreceptors) in response to blood pressure changes triggered by other agonists
c. Direct activation of the juxtaglomerular apparatus, release of aldosterone
d. Inhibition of epinephrine release from chromaffin cells (eg, cells of the adrenal/suprarenal medulla)
e. Regulation of renal blood flow via control of renal arterial tone
66. Guanadrel is an antihypertensive drug: it reduces arteriolar constriction, and in doing so lowers BP by reducing the amount of NE in peripheral adrenergic nerves. Lowered blood pressure is not accompanied by reflex tachycardia, and in fact a reduction of heart rate from predrug levels is the more common outcome. The main ocular effect of guanadrel is miosis. The widespread abolition of sympathetic influences throughout the body often causes diarrhea and urinary frequency. Based on this description, to which prototypic drug is guanadrel most similar in terms of its ultimate qualitative autonomic effects, and in terms of overall mechanism of action?
a. Acetylcholine
b. Atropine
c. Epinephrine
d. Isoproterenol
e. Norepinephrine
f. Propranolol
g. Reserpine
67. An “effective” dose of a drug is given and the following responses occur:
• Stimulates heart rate and, apparently, left ventricular stroke volume
• Dilates some blood vessels but constricts none
• Dilates the bronchi (relaxes airway smooth muscles)
• Raises blood glucose levels
• Neither dilates nor constricts the pupil of the eye
What drug is capable of causing all these responses?
a. Atropine
b. Epinephrine
c. Isoproterenol
d. Norepinephrine
e. Phenylephrine
68. It is common to include small amounts of epinephrine (EPI) in solutions of local anesthetics that will be administered by infiltration (injection around sensory nerve endings), as when a skin laceration needs suturing. What is the most likely reason for, or outcome of, including the EPI?
a. To antagonize the otherwise intense and common vasoconstrictor and hypertensive effects of the anesthetic
b. To counteract cardiac depression caused by the anesthetic
c. To prevent anaphylaxis in patients who are allergic to the anesthetic
d. To reduce the risk of toxicity caused by systemic absorption of the anesthetic
e. To shorten the duration of anesthetic action
69. In your third year of medical school, you are conducting a study on similarities and differences between two prototypic drugs, phentolamine and prazosin, as they affect cardiovascular responses. You selected two identical twins to ensure their pharmacogenetic make-up, and so their responses to drugs, is as nearly identical as possible. One twin will get the phentolamine, the other gets prazosin.
Their cardiovascular parameters at baseline (rest) are identical and normal, and everything else that might have an impact on their drug responses is normal and, well, identical. They aren’t taking any other drugs.
One twin gets an IV injection of phentolamine. His mean blood pressure falls 20 mm Hg in 20 seconds.
The other gets an IV injection of prazosin at an equally effective dose in terms of the blood pressure response. His mean BP falls by an identical amount, 20 mm Hg, over the same time period, 20 seconds.
Which is the most likely difference you will find in the responses of these two lads, one who got phentolamine and the other who got an equivalent pressure-lowering dose of prazosin?
a. Phentolamine will trigger a greater baroreceptor-mediated reflex increase of heart rate and contractility than the prazosin will.
b. Prazosin will lead to a bigger reflex positive inotropic and chronotropic response than phentolamine.
c. Prazosin will block all reflex cardiac responses because it also has strong β-blocking activity.
d. Prazosin will lead to a greater rise of cardiac output than phentolamine by selectively blocking norepinephrine-mediated vasodilation.
e. Phentolamine will reduce left ventricular afterload, prazosin will raise it.
70. A 48-year-old woman has a history of myasthenia gravis. She has been treated with an oral acetylcholinesterase (AChE) inhibitor for several years, and has done well until now. Today she presents in your clinic with muscle weakness and other signs and symptoms that could reflect either a cholinergic crisis (excess dosages of her maintenance drug) or a myasthenic crisis (insufficient treatment). You will use a rapidly acting parenteral acetylcholinesterase inhibitor to help make the differential diagnosis. Which drug would, therefore, be most appropriate to use?
a. Edrophonium
b. Malathion
c. Physostigmine
d. Pralidoxime
e. Pyridostigmine
71. A patient presents with an anaphylactic reaction following a wasp sting. What is the drug of choice for treating the multiple cardiovascular and pulmonary problems that, if not promptly corrected, could lead to the patient’s death?
a. Atropine
b. Diphenhydramine
c. Epinephrine
d. Isoproterenol
e. Norepinephrine
72. Cardiac output improves when dobutamine is given, by IV infusion, to a 60-year-old man with acute, symptomatic heart failure. By what adrenergic receptor-mediated actions, and through which ultimate effects of it, do therapeutic doses of dobutamine mainly raise cardiac output?
a. α-adrenergic agonist
b. α-adrenergic antagonist
c. β1-adrenergic agonist
d. β1-adrenergic antagonist
e. Mixed α and β agonist
f. Mixed α and β antagonist
73. We are using novel in vitro methods to investigate the fate and post-synaptic actions of norepinephrine, released upon an action potential generated in an adrenergic nerve. An action potential is generated and the postsynaptic effector briefly responds. Almost instantaneously the response is over. What process mainly accounted for the brevity of the response, and termination of the released NE’s actions?
a. Metabolism by enzyme(s) located near the postsynaptic receptor(s) and/or in the synaptic cleft
b. Reuptake into the nerve ending
c. Metabolism by catechol-O-methyltransferase (COMT)
d. Degradation by mitochondrial monoamine oxidase (MAO)
e. Conversion to a “false neurotransmitter” in the nerve ending
74. We are contemplating administration of a nonselective β-adrenergic blocker to a patient. In which of the following conditions is this considered generally acceptable, appropriate, and safe?
a. Angina, vasospastic (“variant”; Prinzmetal)
b. Asthma
c. Bradycardia
d. Diabetes mellitus, insulin-dependent and poorly controlled
e. Heart block (second degree or greater)
f. Hyperthyroidism, symptomatic and acute
g. Severe congestive heart failure
75. A patient presents in the Emergency Department in great distress and with the following signs and symptoms:
Which drug most likely caused these signs and symptoms?
a. AChE inhibitor
b. α-adrenergic blocker
c. Antimuscarinic
d. β-adrenergic blocker
e. Parasympathomimetic (muscarinic agonist)
f. Peripherally acting (neuronal) catecholamine depletor
76. Acebutolol and pindolol are classified as β-adrenergic blockers with intrinsic sympathomimetic activity (ISA). In a practical sense, what does ISA mean apropos the actions of these two drugs?
a. Are partial agonists (mixed agonist/antagonists)
b. Cause norepinephrine and epinephrine release
c. Induce catecholamine synthesis
d. Potentiate the actions of norepinephrine on α-adrenergic receptors
e. Useful when cardiac positive inotropic and chronotropic effects are wanted
77. A 10-year-old boy is diagnosed with Attention Deficit/Attention Deficit-Hyperactivity disorder (ADD/ADHD). Which drug is most likely to prove effective for relieving the boy’s main symptoms?
a. Dobutamine
b. Methylphenidate
c. Pancuronium
d. Prazosin
e. Scopolamine
f. Terbutaline
Questions 78 to 84
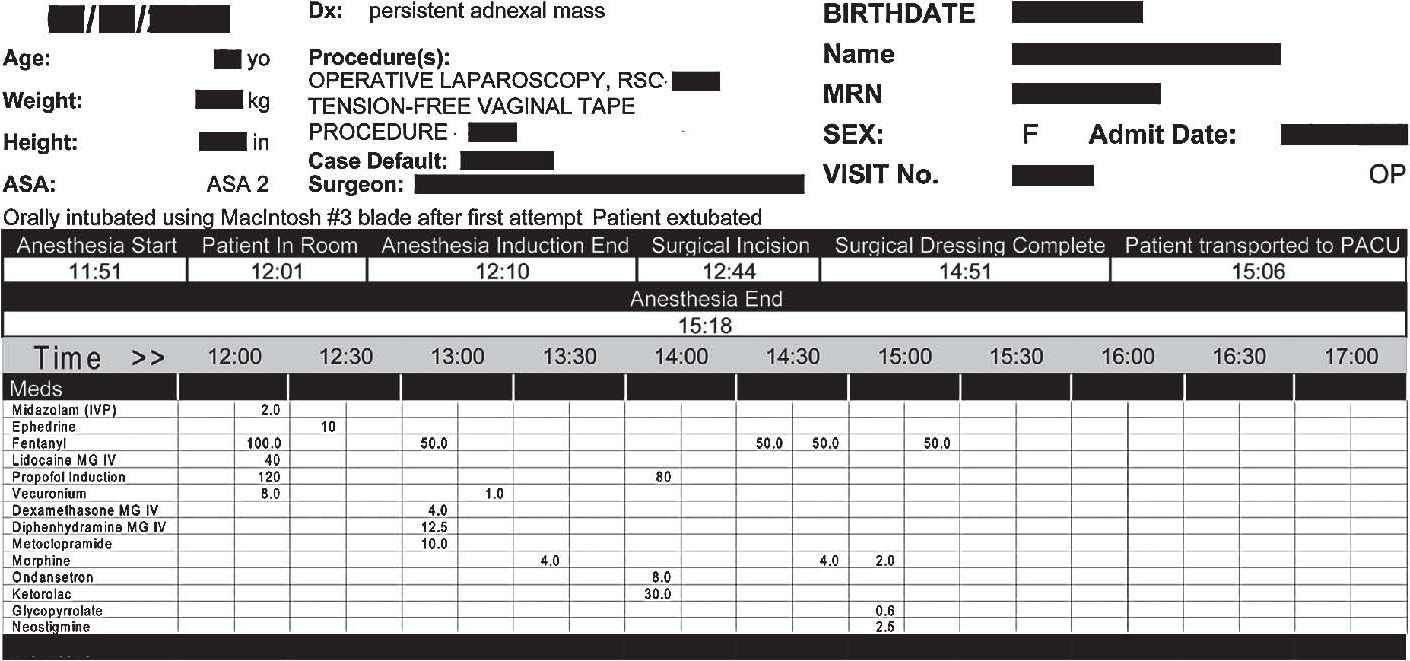
The table below shows the perioperative medication administration record (MAR) for an otherwise healthy 50-year-old woman. (To make things interesting—and write some additional questions—I’ll deviate from her actual MAR and ask a few questions about relevant but hypothetical scenarios.) She is a nonsmoker, consumes no more than four glasses of wine per week, and has no personal or familial risk factors for heart disease or diabetes. She is taking no other medications. This patient had two scheduled (nonemergent) laparoscopic abdominal surgeries done back-to-back in the OR. The first was to remove an adnexal (ovary and/or fallopian tube) mass that had been present for a couple of years and grew slowly and irregularly over a couple of years, and to get a pathology report to see whether it is cancerous. Her pathology affected one ovary. Once the ovary was removed a different surgeon performed a second procedure, through the same belly incisions, to alleviate some inconvenient urinary bladder problems.
Her MAR is very typical of what you would find for many otherwise healthy patients undergoing the same or similar surgeries. The first drug listed, midazolam, was given in the preop area right before she was transported to the OR (and I will address its use in the CNS questions; the abbreviation IVP next to midazolam means “IV push,” that is, a bolus injection). All the rest were given in the OR by a CRNA (certified registered nurse anesthetist).
Use the table’s data, or what you should be able to infer from it, to answer the next seven questions.
78. Ephedrine was the first drug administered after anesthesia premedication and induction with several parenteral drugs. What best describes ephedrine’s mechanism of action?
a. Directly, selectively, strongly stimulates α-adrenergic receptors in the peripheral vasculature
b. Enhances norepinephrine release by blocking presynaptic α-receptors
c. Increases norepinephrine synthesis
d. Inhibits norepinephrine’s intraneuronal metabolic inactivation
e. Releases intraneuronal norepinephrine into the synapse, also weakly but directly activates all adrenergic receptors
79. Ephedrine and drugs that act in similar ways or cause similar effects have a variety of therapeutic uses. Given the background information provided for this patient, and the timing of ephedrine administration on the medication administration record, what is the most likely reason why the ephedrine was given?
a. Cause bronchodilation so mechanical support of ventilation would be easier
b. Counteract CNS depression caused by the induction agents
c. Inhibit sinoatrial and atrioventricular nodal automaticity to terminate or prevent anesthesia-related cardiac arrhythmias
d. Lower heart rate that was raised excessively by the anesthetic drugs
e. Raise blood pressure that was lowered excessively by the induction agents
80. Assume, hypothetically, that the surgery had to be done emergently. The patient had been taking another drug—still in her circulation at usually effective concentrations—that weakened but did not completely eliminate all of ephedrine’s peripheral autonomic effects. Which drug(s) would be most likely to do that?
a. Atenolol (or metoprolol)
b. Cocaine or a tricyclic antidepressant (eg, imipramine)
c. Trimethaphan (or hexamethonium)
d. Pargyline (or a similar nonselective MAO inhibitor)
e. Propranolol
81. Shortly after the surgical wounds were closed and dressed, and right before the patient was transferred to the postanesthesia care unit (PACU), she received neostigmine. What was the reason for which it was given?
a. Raise and support blood pressure during recovery
b. Raise or otherwise control bradycardia upon recovery from anesthesia
c. Restore normal neurotransmission in the brain, since it had been suppressed by the induction and anesthetic agents
d. Reverse skeletal neuromuscular blockade/paralysis
e. Suppress urinary bladder function to reduce the risk of postoperative bladder incontinence
82. The patient got her dose of glycopyrrolate mere seconds before the neostigmine was injected. This is done routinely in thousands of surgeries in which the drugs used are identical or at least very similar to those used here. To which pharmacologic class does glycopyrrolate most likely belong?
a. α-Adrenergic agonist
b. Antimuscarinic (atropine-like)
c. Cholinesterase inhibitor
d. Muscarinic receptor agonist
e. Nicotinic receptor (skeletal muscle; NM) agonist
83. The patient in the case presented here was not facing any emergent or imminently life-threatening problems, so skeletal muscle paralysis and intubation were relatively straightforward procedures, not at all rushed. Now assume, hypothetically, that emergency intubation was required, and succinylcholine (SuCh) was used because of its very rapid onset of action. Assume further that a slow infusion of SuCh was used to maintain paralysis throughout the procedure; blood levels of the drug were kept well in the therapeutic range; no curare-like (nondepolarizing) blocker was used; and the patient had no genetic or other factors that would affect the drug’s pharmacokinetics or action. When the surgery is done, what drug would be given to reverse succinylcholine’s effects?
a. Atropine
b. Bethanechol
c. Neostigmine
d. Physostigmine
e. Nothing
84. Now assume this patient received bethanechol several hours after her abdominal surgery, after effects of all the drugs used intraoperatively, except for morphine and ketorolac (analgesics) had worn off. Her heart rate fell slightly and she experienced some wheezing. Which word or phrase most likely accounts for or describes these cardiac and pulmonary responses?
a. Expected side effects
b. Idiosyncrasy
c. Parasympathetic ganglionic activation
d. Reflex (baroreceptor) suppression of cardiac rate
e. Undiagnosed asthma
85. Until recently the drug ritodrine has been used to suppress uterine contractions in some women who are in premature labor. Side effects of the drug include rises of heart rate and increases in the force of contraction of the heart. High-output heart failure (caused by excessively increased cardiac output) and pulmonary edema have occurred, and in some cases the outcome has been fatal. Ritodrine also causes bronchodilation. It has no vasoconstrictor effects, nor any effects on the size of the pupil(s) of the eye(s). The description most closely fits the characteristics of what class of drugs?
a. α-Adrenergic agonist
b. Atropine-like/antimuscarinic drug
c. β-Adrenergic agonist
d. β-Adrenergic blocker
e. Muscarinic receptor agonist (parasympathomimetic)
86. A patient with a history of asthma experiences significant bronchoconstriction and urticaria, and drug-induced histamine release is a main contributor to these responses. Which drug is most likely to have caused these problems—not because it has any bronchoconstrictor or histamine agonist effects in its own right, but because it quite effectively releases histamine from mast cells?
a. Atropine
b. Morphine
c. Neostigmine
d. Pancuronium
e. Propranolol
87. During surgery the anesthesiologist administers trimethaphan, classified as an autonomic ganglionic blocker to an anesthetized patient. What would you expect in response to this drug?
a. Bradycardia mediated by activation of the baroreceptor reflex
b. Increased GI tract motility, possible spontaneous defecation
c. Increased salivary secretions
d. Miosis
e. Vasodilation
88. “First-generation” (older) histamine H1 blockers such as diphenhydramine, phenothiazine antipsychotic drugs (eg, chlorpromazine), and tri-cyclic antidepressants (eg, imipramine) have pharmacologic actions, side effects, toxicities, and contraindications that are very similar to those of which other drug?
a. Atropine
b. Bethanechol
c. Isoproterenol
d. Neostigmine
e. Propranolol
89. A 6-year-old is transported to the Emergency Department by a parent, who says the boy took a large amount of an allergy medication. The sole active ingredient in the product the parent mentions is diphenhydramine, and it is clear the child is experiencing toxicity from an overdose. The intern, fresh out of medical school, orders parenteral administration of neostigmine, and the medication order is not questioned. What adverse effect of the diphenhydramine will persist following neostigmine administration?
a. Bronchoconstriction and wheezing
b. Delirium, hallucinations, and other CNS manifestations of toxicity
c. Profuse secretions from lacrimal, mucus, and sweat glands
d. Skeletal muscle tremor or fasciculations
e. Tachycardia
90. In between your M1 and M2 years you are volunteering in a hospital in a very poor part of the world. Their drug selection is limited. A patient presents with acute cardiac failure, for which your preferred drug is dobutamine, given intravenously. However, there is none available. Which other drug, or combination of drugs, would be a suitable alternative, giving the pharmacologic equivalent of what you want the dobutamine to do? (All these drugs are available in parenteral formulations.)
a. Dopamine (at a very high dose)
b. Ephedrine
c. Ephedrine plus propranolol
d. Norepinephrine plus phentolamine
e. Phenylephrine plus atropine
91. In general, structures that are affected by sympathetic influences respond to both sympathetic neural activation and to the hormonal component, epinephrine released from the adrenal medulla. Which structure/function is unique in that it responds to epinephrine, but not norepinephrine, and has no direct sympathetic neural control?
a. Airway (tracheal, bronchiolar) smooth muscle: relaxation
b. Atrioventricular node: increased automaticity and conduction velocity
c. Coronary arteries: constriction
d. Iris of the eye: dilation (mydriasis)
e. Renal juxtaglomerular apparatus: renin release
92. Adrenergic nerves to the heart are activated, leading to a reflex increase of heart rate and cardiac contractility, in response to a sudden and significant fall of blood pressure. Those sympathetic nerves release norepinephrine (NE). What is the main physiologic mechanism by which the actions of the released NE are terminated?
a. Diffusion away from postsynaptic receptors
b. Hydrolysis by nonspecific deaminases
c. Metabolic inactivation by MAO
d. Metabolic inactivation by catechol-O-methyltransferase
e. Reuptake into the adrenergic nerve from which the NE was released
93. The figure below shows several responses measured in a subject (healthy; receiving no other drugs) at rest (before) and after receiving a dose of an unknown drug. Note: The blood pressures shown can be considered mean blood pressure; the fall caused by the unknown was mainly due to a fall of diastolic pressure.
Which drug most likely caused the observed responses?
a. Atropine
b. Isoproterenol
c. Neostigmine
d. Phenylephrine
e. Propranolol
94. A 59-year-old man has a history of emphysema from 40 years of cigarette smoking; hypercholesterolemia that is being managed with atorvastatin; and Stage 2 essential hypertension for which he is taking metolazone. He presents in clinic today with his main new complaints: nocturia, urinary frequency, and an inability to urinate forcefully and empty his bladder. Following a complete work-up, the physician arrives at a diagnosis of benign prostatic hypertrophy (BPH). We start daily therapy with tamsulosin. What is the most likely side effect the patient may experience from the tamsulosin, and about which he should be forewarned?
a. Bradycardia
b. Increased risk of statin-induced skeletal muscle pathology
c. Orthostatic hypotension
d. Photophobia and other painful responses to bright lights
e. Wheezing or other exacerbations of the emphysema
95. A patient walks out of the ophthalmologist’s office and into bright sunlight after a comprehensive eye exam, for which he received a topical ophthalmic drug. The drug has not only dilated his pupils, but also impaired his ability to focus his eyes up-close.
The drug this patient received was most likely classified as, or worked most similar to, which prototype?
a. Acetylcholine
b. Epinephrine
c. Homatropine
d. Isoproterenol
e. Pilocarpine
f. Propranolol
96. You’ve received approval from the Institutional Review Board to study the in vitro (tissue bath) responsiveness of isolated human arteriolar segments (obtained during surgery) to a variety of pharmacologic and other interventions. The tissue samples are 1 cm-long “cylinders” of otherwise-normal (but now denervated) arterioles obtained from the lower legs of patients undergoing amputation surgery.
The setup allows you to perfuse the vessels with a solution that will keep the tissue functionally and structurally intact for many hours; to monitor and change perfusion pressure (mm Hg; analogous to “blood pressure” in the intact organism) and perfusate flow (mL/min); and to assess the effects of various vasoactive drugs on the system.
You add ACh to the perfusate to give a concentration identical to the plasma concentration of ACh that causes “expected responses” in an intact human.
Under this experimental setup, adding ACh causes a rise of perfusion pressure and a decrease of flow, both of which basically reflect vasoconstriction.
What is the most likely explanation for these findings?
a. ACh released norepinephrine from the endothelium, which caused vasoconstriction
b. Atropine was added to the tissue bath before adding the ACh
c. Botulinum toxin was added to the bath before adding the ACh
d. The vascular endothelium has been damaged or removed (denuded)
e. This response is precisely what we’d expect with injection of ACh into the intact human
97. A 33-year-old woman becomes poisoned after receiving an injection of illicitly prepared and overly concentrated botulinum toxin. What is the main neurochemical mechanism by which this Clostridium toxin causes its effects?
a. Directly activates all muscarinic and nicotinic receptors
b. Inhibits ACh release from all cholinergic nerves
c. Prevents neuronal norepinephrine reuptake
d. Releases norepinephrine via a nonexocytotic process
e. Selectively and competitively blocks nicotinic receptors
98. A 43-year-old woman with diagnosed myasthenia gravis, and taking pyridostigmine daily, presents in the neurology clinic with profound skeletal muscle weakness. You are unsure whether she is experiencing a cholinergic crisis or a myasthenic crisis, so you administer a usually appropriate diagnostic dose of parenteral edrophonium. Assume the patient was actually experiencing a cholinergic crisis. What is the most likely response to the edrophonium?
a. Hypertensive crisis from peripheral vasoconstriction
b. Myocardial ischemia, and angina, from drug-induced tachycardia and coronary vasoconstriction
c. Premature ventricular contractions from increased ventricular automaticity
d. Prompt improvement of skeletal muscle tone and function
e. Ventilatory distress or failure
99. A patient takes a massive overdose of diphenhydramine, suffering not only significant CNS depression but also numerous and serious peripheral autonomic side effects. By what mechanism did diphenhydramine exert its untoward peripheral autonomic actions?
a. Activation of both β1 and β2 adrenoceptors
b. Blockade of α-adrenergic receptors
c. Competitive antagonism of ACh actions on muscarinic receptors
d. Massive, direct overactivation of ganglionic nicotinic receptors
e. Sudden release of epinephrine from the adrenal medulla (suprarenal medulla)
100. A patient with a recent drug poisoning is transported to the emergency department. The physician correctly orders administration of pralidoxime as part of the comprehensive emergency treatment plan. Which best describes who the patient was?
a. A 13-year-old boy who to took an overdose of methylphenidate for his ADD/ADHD.
b. A 43-year-old who took an overdose of neostigmine, prescribed for her myasthenia gravis, in a suicide attempt.
c. A 6-year-old who got into the family medicine cabinet and took 10 “adult doses” of her dad’s prazosin.
d. A farm/field worker accidentally doused with insecticide from an overflying crop-duster plane.
e. An asthma patient who accidentally gave himself an intravenous injection of epinephrine in an attempt to self-treat a developing anaphylactic reaction.
101. To facilitate a certain eye exam you want to cause mydriasis, but not alter normal control of accommodation. All of the following drugs are available as topical ophthalmic formulations. Which one will dilate the pupil without altering accommodation?
a. Atropine
b. Epinephrine
c. Homatropine
d. Isoproterenol
e. Pilocarpine
f. Timolol
102. A 26-year-old woman has rhinorrhea, excessive lacrimation, and ocular congestion from a bout with the common cold. Diphenhydramine provides symptomatic relief. What is the most likely mechanism by which this drug relieved her symptoms?
a. α-adrenergic activation (agonist, vasoconstrictor)
b. β-adrenergic blockade
c. Calcium channel blockade
d. Histamine (H2) receptor blockade
e. Muscarinic receptor blockade
103. You have treated dozens of patients with acute hypotension from various causes, including overdoses of antihypertensive drugs, all of which can cause hypotension. Your usual approach to restoring blood pressure, and one that has worked well every time before, is to inject x mg of phenylephrine intravenously. Today a patient with severe drug-induced hypotension presents in the Emergency Department. He has been taking this drug for many months. He is not volume-depleted, nor hemorrhaging. You give the phenylephrine at the same dose and by the same route as you always have. It causes no change of blood pressure. Which drug did the patient most likely take and overdose on?
a. Atenolol
b. Bethanechol
c. Prazosin
d. Propranolol
e. Reserpine
104. This is a strange day for you in the ED. Now you have to treat another normovolemic patient with acute drug-induced hypotension, and give the usually correct and effective dose of phenylephrine. This time the drug causes a vasopressor response that is far greater than you’ve ever encountered when giving the very same dose: systolic pressure rises dramatically, if not dangerously. What drug did the patient most likely take?
a. Atenolol
b. Bethanechol
c. Prazosin
d. Propranolol
e. Reserpine
105. A patient who will be new to your practice makes an appointment for their first visit. Your nurse asks them to bring in all their current prescribed medications and any OTC drugs they take regularly. They comply. One OTC drug is a popular brand-name product that contains doxylamine as its sole active ingredient. Which property or characteristic best describes this drug?
a. Likely to lower heart excessively
b. May be a cause of diarrhea that the patient says he often gets
c. Should not be used by patients with prostatic hypertrophy or angle-closure glaucoma
d. Tends to raise blood pressure through a typical catecholamine-like vasoconstrictor (α-adrenergic) mechanism
e. Used during the day, helps them keep awake and alert via a weak amphetamine-like action in the CNS
The Peripheral Nervous Systems: Autonomic and Somatic Nervous System Pharmacology
Answers
I’ve reproduced below the figure you saw in the questions section, but modified it to show the nerve types and locations, and the receptors, to save you a bit of page-flipping when you review your answers.
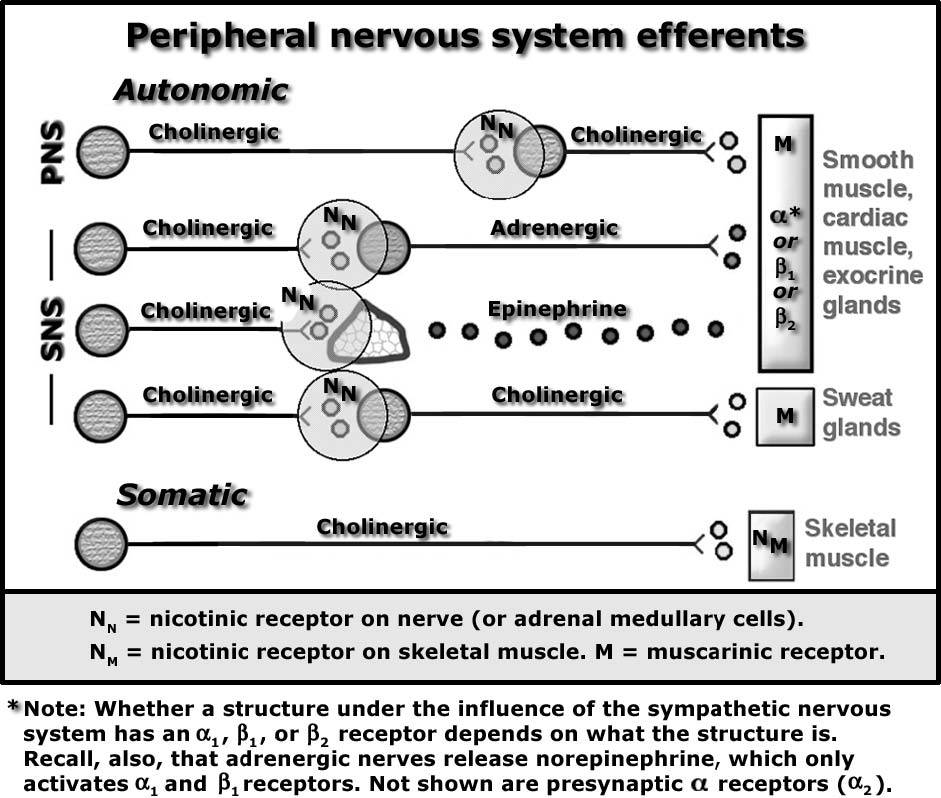
37. The answer is b. (Brunton, pp 171-177; Katzung, pp 80-87.) Here’s a simple rule: in the peripheral nervous systems—that is, the somatic nervous system and both branches of the autonomic nervous system—“the first nerve ‘out’ of the CNS (in this diagram, a, c, e, f, and h) is always cholinergic and the ACh released from those nerves always activates the nicotinic subtype of cholinergic receptor on the postsynaptic target cell(s).”
38. The answer is c. (Brunton, pp 171-177; Katzung, pp 80-87) Another rule, with one important exception: “all the efferents in the peripheral nervous systems are cholinergic except postganglionic sympathetics going to structures other than sweat glands” (and the arrector pili muscles too). There are eight nerves in the schematic. Seven of them—all except the majority of postganglionic sympathetics (nerve d)—are cholinergic (synthesize and release ACh as their neurotransmitter). The main postganglionic sympathetic fibers (except those innervating sweat glands) synthesize and release NE (not epinephrine; answer d) as their neurotransmitter, and so are adrenergic (or noradrenergic if you prefer) nerves. What else can you call nerve d? A postganglionic sympathetic nerve to certain smooth muscles, to cardiac muscle, and certain exocrine glands except sweat glands. (Be sure to see the explanation for Questions 38 and 40.)
Atropine (a) is incorrect. It selectively and competitively blocks the effects of ACh (and other muscarinic agonists) on muscarinic receptors. In the diagram above, those receptors are found on structures innervated by nerves b and g.
Answer b is incorrect. NE, nerve d’s neurotransmitter, is an effective agonist for α-adrenergic receptors (α1 and α2) and for β1 receptors. Bronchodilation caused by sympathetic activation requires activation of β2 receptors; NE cannot do that but EPI, released from the adrenal (suprarenal) medulla, certainly can. And once NE has been released from its neurons and activates its postsynaptic receptors, its actions are promptly terminated by reuptake (via an “amine pump” that can be blocked by cocaine or tricyclic antidepressants). Hydrolysis in the synaptic cleft (e) is the mechanism by which the actions of ACh, released from cholinergic nerves, is terminated.
39. The answer is d. (Brunton, pp 194-200; Katzung, pp 85-86.) The actions of norepinephrine (NE), released from adrenergic nerves, are terminated by neuronal reuptake. (Don’t forget that this reuptake process is inhibited by cocaine and tricyclic antidepressants, and the outcome is increased and more prolonged adrenergic effects of NE because NE lingers longer and accumulates in the synapse, exposed to its postsynaptic targets.) All the other nerves shown in the diagram are cholinergic; the actions of the ACh they release are terminated promptly by hydrolysis (via acetylcholinesterase).
40. The answer is g. (Brunton, pp 119, 196-198, 201, 400-401; Katzung, pp 84-87.) The neurotransmitter released from nerve d, the postganglionic sympathetic fibers (to structures other than sweat glands and arrector pili muscles), is norepinephrine. NE can activate α-adrenergic receptors (both α1 and α2), and β1 receptors (not β2). Of course, different structures have different subtypes of these receptors: structures such as arterioles and the iris dilator muscle have α1 receptors; β1 receptors are found in the heart and in the juxtaglomerular apparatus (kidneys; they help regulate renin release there), while β2 receptors (not activated by NE) are found on various smooth muscles, mainly in the airways. So, the only correct response to the question “which receptors are activated?” really depends on which structure is being innervated. As a final note, NE cannot activate cholinergic receptors, and so answers e and f are definitely incorrect.
41. The answer is b. (Brunton, pp 173-180; Katzung, pp 80f, 90t, 120.) The postganglionic sympathetic fibers innervating sweat glands and arrector pili muscles are cholinergic. That is the exception to the rule that “all postganglionic sympathetic fibers are adrenergic.” How do you know it’s cholinergic? A variety of biochemical and histochemical methods can prove that ACh is the neurotransmitter. They also show that there is abundant acetylcholinesterase (AChE), which hydrolyzes ACh, in the synaptic cleft. But we’re going to make the assessment pharmacologically: We can prevent release of neurotransmitter from nerve g with botulinum toxin, which affects only (and all) cholinergic nerves; and we can prevent the response of the sweat glands innervated by nerve g with atropine, the prototype muscarinic receptor antagonist—a drug that has no effects on nicotinic (or other) receptors (eg, answer d) at usual doses. Likewise, nicotinic receptor blockers (or nicotine itself) have no effect at this site—another reason why answer d is incorrect. And how you do know it’s part of the SNS? Sweat glands are activated (secretions are increased) and arrector pili muscles contract (the hair on our skin “stands on end”) when the entire SNS is activated, such as in the “fight or flight response;” and if you trace the origins of the preganglionic nerves that activate the postganglionic ones, they emanate from the same regions of the spinal cord from which all other sympathetic preganglionic fibers arise—the thoracic and lumbar regions.
Cocaine (a) is incorrect. It, and tricyclic antidepressants (eg, amitriptyline, imipramine, etc), block neuronal reuptake of NE. That is, its site of action is at the neuroeffector junction of postganglionic sympathetic neurons (nerve d)—all of them except those that innervate most sweat glands and arrector pili muscles, of course.
42. The answer is c. (Brunton, pp 173-180; Katzung, pp 80f, 90t.) The nerve is cholinergic, so the neurotransmitter it acts on, postsynaptically, must be either nicotinic or muscarinic. Nicotinic receptors are found on cell bodies of all postganglionic nerves (in both SNS and PNS; NN receptors), on the adrenal medulla (also NN), and on skeletal muscle (somatic nervous system, NM)—at the “first synapses out of the CNS.” Cholinergic receptors at all other sites are muscarinic, “defined” by the fact that those receptors are competitively blocked by atropine. Be sure to see the explanation for Question 37, above.
43. The answer is h. (Brunton, pp 177, 258-262; Katzung, pp 80f, 466-479, 474t.) Vecuronium and several related drugs (all of which have “curonium” or, at least, “cur” in their generic names) are nondepolarizing skeletal neuromuscular blockers (quite different, mechanistically, from succinylcho-line, the depolarizing blocker). They specifically and competitively block activation of nicotinic receptors (NM) on skeletal muscle by ACh, thereby preventing skeletal muscle depolarization and subsequent contraction; and have no effect on muscarinic receptors or any of the adrenergic receptor subtypes. Remember something about the natives of the Amazon obtaining a poisonous substance from the skin of certain species of frogs, putting it on the tips of their darts, and using that to kill their dinner with a blow-gun? That was curare, d-tubocurarine, the very old prototype nondepolarizing skeletal neuromuscular blocker, as we’ve come to know it.
44. The answer is a. (Brunton, pp 173f, 194-200; Katzung, pp 80f, 84-87.) The neurotransmitter of postganglionic sympathetic nerves is norepinephrine (unless the target cells are sweat glands or arrector pili muscles, in which case the final neurotransmitter is acetylcholine). Norepinephrine is a “good” agonist for α- and β1-adrenergic receptors, but not for β2. Airway smooth muscle cells are not innervated by the sympathetic nervous system. In terms of sympathetic influences, bronchodilation (airway smooth muscle relaxation) is caused only by epinephrine released from the adrenal (suprarenal) medulla.
Here again is the diagram to which Questions 45 to 49 referred.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree