•
Areas with prominent myxoid change
•
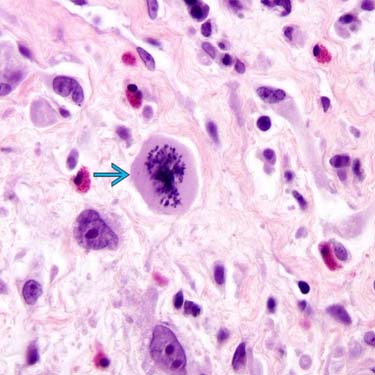
Scattered enlarged atypical tumor cells, some with macronucleoli
Cells with macronucleoli resemble Reed-Sternberg cells
•
Fibroblasts often vacuolated (pseudolipoblasts)
•
Lesional cells are fibroblasts ultrastructurally
•
Variable expression of CD34, CD68, EGFR, CD163, CD117, EMA
•
Negative CD15, CD30, CD45 in cells with macronucleoli
•
Rearrangements of
TGFBR3 &/or
MGEA5 reported, but their presence in these tumors is subject of debate
•
Extranodal Hodgkin disease
•
Pigmented villonodular tenosynovitis
•
Hemosiderotic fibrohistiocytic lipomatous lesion
•
Acral myxoinflammatory fibroblastic sarcoma (MIFS)
•
Inflammatory myxohyaline tumor of distal extremities (with virocyte or Reed-Sternberg-like cells)
•
Low-grade fibroblastic sarcoma characterized by typical acral presentation and inflammatory background, often rich in eosinophils
•
Slow-growing infiltrative mass usually affecting distal extremities (hands and feet) of adults
Subset of lesions presents in axial rather than acral sites
•
Lesions are often present for years before patients seek medical attention
•
Often clinically mistaken for pigmented villonodular tenosynovitis
•
Recurrences are common, especially in examples with prominent atypical nuclei, but metastases are rare
Metastases in only ~ 1% of cases
•
Can involve both superficial and deep soft tissues
•
Most lesions measure 3-4 cm
•
Poorly marginated tumor with fibrosis, hyalinization, myxoid stroma, and inflammatory components
Various lesions have different proportions of each component
•
Variable background of lymphoplasmacytic cells, eosinophils, neutrophils, and histiocytes
•
Lesional cells are fibroblasts ultrastructurally
•
Scattered enlarged atypical fibroblasts, some with macronucleoli
Cells with macronucleoli resemble Reed-Sternberg cells
•
Areas with prominent myxoid change
Fibroblasts often vacuolated (“pseudolipoblasts”)
These areas resemble myxofibrosarcoma (malignant fibrous histiocytoma)
•
Low mitotic rate
Low proliferative index by Ki-67
Atypical mitoses may be encountered
•
Variable expression of CD34, CD68, EGFR, CD163, CD117, EMA
•
Negative CD15, CD30, CD45 in cells with macronucleoli
•
No demonstration of various viral agents
Cases have been tested for Epstein Barr virus and for cytomegalovirus (CMV) and herpes simplex virus (HSV)
•
Rearrangements of
TGFBR3 &/or
MGEA5 have been reported
Same rearrangements have been reported in hemosiderotic fibrolipomatous tumor (HFLT), pleomorphic hyalinizing angiectatic tumor
Same rearrangements have been reported in rare tumors allegedly showing features of both HFLT and MIFS termed hybrid HFLT-MIFS
Initially myxoinflammatory fibroblastic sarcoma was associated with t(1;10)
Subject of controversy in literature
•
Probably MIFS in fact lacks rearrangements of
TGFBR3 &/or
MGEA5 when strict morphologic criteria are used
•
Additional studies will be needed to clarify genetics of these tumors
•
Patients usually have history of nodal disease
•
Usually no myxoid areas
•
Background mostly lymphoid cells; neutrophils not common
•
Reed-Sternberg cells label with CD15 and CD30 and are lymphoid rather than fibroblastic
•
Managed as per lymphomas


 is present throughout the neoplasm.
is present throughout the neoplasm.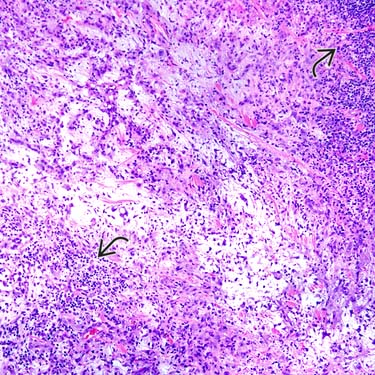
 .
.
 in these tumors is unusual for a translocation sarcoma, but rearrangements TGFBR3 &/or MGEA5 have been reported in some cases.
in these tumors is unusual for a translocation sarcoma, but rearrangements TGFBR3 &/or MGEA5 have been reported in some cases. Same rearrangements have been reported in hemosiderotic fibrolipomatous tumor (HFLT), pleomorphic hyalinizing angiectatic tumor
Same rearrangements have been reported in hemosiderotic fibrolipomatous tumor (HFLT), pleomorphic hyalinizing angiectatic tumor Same rearrangements have been reported in rare tumors allegedly showing features of both HFLT and MIFS termed hybrid HFLT-MIFS
Same rearrangements have been reported in rare tumors allegedly showing features of both HFLT and MIFS termed hybrid HFLT-MIFS Same rearrangements have been reported in hemosiderotic fibrolipomatous tumor (HFLT), pleomorphic hyalinizing angiectatic tumor
Same rearrangements have been reported in hemosiderotic fibrolipomatous tumor (HFLT), pleomorphic hyalinizing angiectatic tumor Same rearrangements have been reported in rare tumors allegedly showing features of both HFLT and MIFS termed hybrid HFLT-MIFS
Same rearrangements have been reported in rare tumors allegedly showing features of both HFLT and MIFS termed hybrid HFLT-MIFS


















