Myopericytoma
Thomas Mentzel, MD
Key Facts
Terminology
Benign perivascular neoplasm composed of perivascular myoid tumor cells (myopericytes)
Myopericytoma forms morphologic spectrum with angioleiomyoma, myofibroma, glomus tumor, and so-called hemangiopericytoma
Clinical Issues
Arises most commonly in mid-adulthood
Arises most commonly in dermal/subcutaneous tissues
Distal extremities are most frequently involved
Usually solitary lesions
Most lesions do not recur
Microscopic Pathology
Numerous thin-walled blood vessels
Perivascular multilayered concentric growth
Plump spindled &/or round myoid tumor cells
Round, plump, spindled nuclei
No prominent atypia
Homogeneous expression of actins and HCAD
Desmin, S100 protein, CD, and epithelial markers are usually negative
May show focal areas similar to glomus tumor, angioleiomyoma, or myofibroma
Variable morphologic features
Classic solid variant
Hemangiopericytoma-like variant
Angioleiomyoma-like variant
Intravascular variant
Malignant variant
 Clinical photograph shows a raised nodular lesion mimicking a vascular neoplasm arising on the lower leg of an adult male patient. |
TERMINOLOGY
Synonyms
Hemangiopericytoma
Definitions
Benign perivascular neoplasm composed of perivascular myoid tumor cells (myopericytes)
Myopericytoma forms morphologic spectrum with angioleiomyoma, myofibroma, and glomus tumor
CLINICAL ISSUES
Epidemiology
Incidence
Rare
Age
Arises most commonly in mid-adulthood
Children are rarely affected
Site
Arises most commonly in dermal/subcutaneous tissues
Arises rarely in deep soft tissues
Distal extremities are most frequently involved
Proximal extremities, such as neck and trunk, more rarely involved
Rare malignant examples usually arise in deep soft tissues
Presentation
Painless mass
Usually solitary lesions
Multiple lesions are very rare
Slow-growing
Subcutaneous mass
Natural History
Often longstanding neoplasms
No increased number of local recurrences
Treatment
Surgical approaches
Complete excision
Prognosis
Most lesions do not recur
Local recurrences are related to poor circumscription
Very rare malignant myopericytomas characterized by poor clinical outcome
MACROSCOPIC FEATURES
General Features
Nodular indurated lesions
Variable number of vessels
MICROSCOPIC PATHOLOGY
Histologic Features
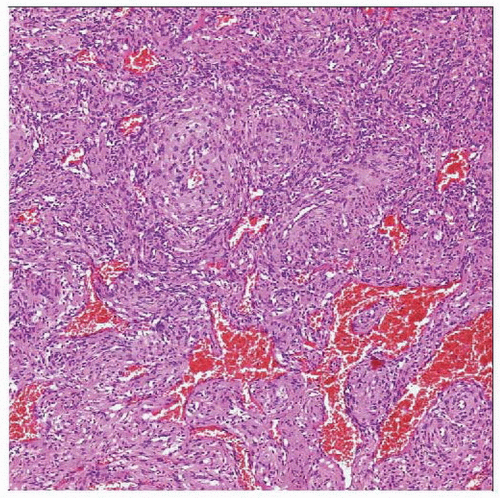
Numerous thin-walled blood vessels
Perivascular multilayered concentric growth
Plump spindled &/or round myoid tumor cells
Tumor cells with eosinophilic or amphophilic cytoplasm
Round, plump, spindled nuclei
Mitoses are rare
May show focal areas similar to glomus tumor, angioleiomyoma, or myofibroma
Areas of infarction and hemorrhage especially in deepseated neoplasms
Degenerative atypia may be present in longstanding neoplasms
Prominent degenerative stromal changes in longstanding neoplasms
May show prominent myxoid stromal changes
Variable morphologic features
Classic solid variant
Narrow, closely packed vessels
Vessels are concentrically surrounded by spindled &/or round tumor cells
Hemangiopericytoma-like variant
Dilated, branching, thin-walled vessels
Perivascular growth of myoid tumor cells
Angioleiomyoma-like variant
Perivascular growth of elongated spindled cells
Intravascular variant
Intravascular or intramural growth
Closely packed, thin-walled vessels
Vessels are concentrically surrounded by myoid tumor cells
Malignant variant
Infiltrative growth
Prominent cytologic atypia
Numerous mitoses
Areas of tumor necrosis
Rare hypocellular fibroma-like variant
Rare immature cellular variant
Predominant Pattern/Injury Type
Circumscribed
Hemangiopericytic
Predominant Cell/Compartment Type
Mesenchymal
Myoid tumor cells
ANCILLARY TESTS
Cytogenetics
Characteristic t(7;12)(p21-22;q13-15)
ACTB-GLI fusion
DIFFERENTIAL DIAGNOSIS
Myofibroma
Biphasic growth
Undifferentiated mesenchymal tumor cells associated with numerous thin-walled vessels showing hemangiopericytoma-like growth
Mature, spindled, eosinophilic tumor cells
Often multinodular growth
Myxohyaline stromal changes
HCAD(-): Rarely focal positivity
Angioleiomyoma
Thick-walled vessels
Predominance of spindled eosinophilic tumor cells
Usually desmin(+)