Mycosis Fungoides
Sa A. Wang, MD
Key Facts
Terminology
Primary cutaneous T-cell lymphoma characterized by
Epidermotropism
Clinical course showing stepwise evolution of patches, plaques, and tumors
Clinical Issues
Overall indolent clinical course
Clinical stage is most important predictor of prognosis
Microscopic Pathology
Skin biopsy findings are nondiagnostic in premycotic and some early patch stage lesions
Superficial band-like or lichenoid infiltrate in patch and thin plaque stage
Dense, subepidermal band-like infiltrate in thick plaque stage
Prominent dermal infiltrate in tumor stage
Large cell transformation: Large tumor cells are > 25%
Ancillary Tests
Immunophenotype
CD3(+), CD5(+), TCR-αβ/βF1(+)
CD4(+), CD8(-), CD7(-), CD26(-)
Top Differential Diagnoses
Drug reaction, inflammatory dermatoses
Primary cutaneous CD30(+) T-cell lymphoproliferative disorders
Primary cutaneous γ/δ T-cell lymphoma
Rare variants of T-cell lymphoma involving skin
 The plaque stage of mycosis fungoides shows the presence of multiple red plaques on much of the body surface of this patient. |
TERMINOLOGY
Abbreviations
Mycosis fungoides (MF)
Definitions
Primary cutaneous T-cell lymphoma characterized by
Epidermotropism
Clinical course showing stepwise evolution of patches, plaques, and tumors
ETIOLOGY/PATHOGENESIS
Unknown
Chronic antigenic stimulation, possibly due to infectious agent, may play role
Genetic abnormalities are likely to be involved
CLINICAL ISSUES
Epidemiology
Incidence
0.6/100,000 people per year
50% of all cases of primary cutaneous lymphoma
Age
Adults, 5th-6th decade
Can be seen in patients < 35 years
Gender
M:F = 2:1
Ethnicity
Incidence is 1.7x higher in African-Americans than in whites
Presentation
Premycotic period
Nonspecific skin lesions; often slight scaling, pruritus
Lesions can wax and wane for years; may never progress to MF
Skin biopsy findings are nondiagnostic
Stepwise evolution of disease with appearance of patches, plaques, and tumors
Patches
Mostly on trunk but can arise anywhere on body including palms and toes
Can be associated with alopecia
Plaques
Palpable lesions raised above skin surface
Can be associated with patch lesions
Tumors
Usually manifest as skin nodule(s)
Can coexist with patches and plaques
MF variants
Pagetoid reticulosis
Also referred to as Woringer-Kolopp disease
Solitary, slow-growing, psoriasiform, crusty or hyperkeratotic patches or plaques
Often arises on distal limb
Folliculotropic (pilotropic) MF
Often involves head and neck area
Follicular papules (often grouped), alopecia, and acneiform lesions
Clinically more aggressive than other MF types; responds less well to skin-directed therapy
Syringotropic MF
Solitary, well-circumscribed, red-brown plaque, often associated with alopecia
Skin-directed therapy may be inadequate (similar to folliculotropic MF)
Granulomatous slack skin
Circumscribed areas of pendulous folds of lax skin in major folds (axillae, groin)
May coexist with classical MF lesions or classical Hodgkin lymphoma
Laboratory Tests
Morphologic assessment of peripheral blood for Sézary cells
Insensitive
Flow cytometry immunophenotypic analysis
Aberrant T-cell immunophenotypes support involvement by MF
Assessment of T-cell clonality by PCR
Serum lactate dehydrogenase &/or β-2-microglobulin
High levels associated with poorer prognosis
Natural History
Over time, some patients develop visceral involvement by MF
Most common sites: Lungs, liver, spleen
Treatment
Early-stage disease (stages I and IIA) requires direct skin therapy
Topical chemotherapy with nitrogen mustard or carmustine
Topical corticosteroids and retinoids
Phototherapy; local radiation (x-ray or electron beam)
Advanced-stage disease (stages IIB-IV)
Extracorporeal photopheresis
Single-agent chemotherapy
Methotrexate, pegylated liposomal doxorubicin (Doxil), purine analogs (fludarabine, 2-deoxycoformycin), others
Combination chemotherapy: Many regimens have been used
Cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP)
Cyclophosphamide, vincristine, and prednisone (CVP)
CVP with methotrexate (COMP)
Hematopoietic cell transplantation
Prognosis
Indolent clinical course overall
Disease prognosis depends on clinical stage
Clinical significance of T-cell receptor (TCR) gene rearrangements in MF staging is controversial
Monoclonal TCR gene rearrangement in blood is extremely common in early-stage disease
Not synonymous with blood involvement by MF in absence of morphologic or immunophenotypic evidence of disease
Monoclonal TCR gene rearrangement in lymph nodes is common finding
Not prognostically significant in multivariate analysis
MACROSCOPIC FEATURES
General Features
Patches
Circumscribed lesions with discoloration of variable size, color, and shape
Little scaling, not palpable
Plaques
Palpable infiltrate of variable stage (thin and thick)
Tumors
Often exophytic and ulcerated (hence term “fungoides”)
MICROSCOPIC PATHOLOGY
Histologic Features of Skin
Premycotic stage (parapsoriasis)
Skin biopsy findings are nondiagnostic
Lymphocytic infiltrate
Mainly in upper dermis, not in subepidermal zone
No epidermotropism
Patch and early (thin) plaque stage
Superficial band-like or lichenoid infiltrate by lymphocytes and histiocytes
Atypical lymphocytes infiltrate basal layer, especially tips of rete ridges
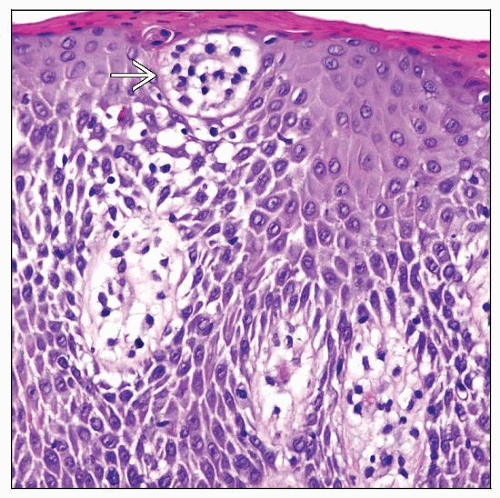
Epidermotropism with single-cell infiltrate
Neoplastic lymphocytes are small, slightly cerebriform, some with halos
Other changes
Mild acanthosis, hyperkeratosis; basal layer damage
Edema and fibrosis, increased postcapillary venules
In some early lesions, skin biopsy findings are nondiagnostic
Thick plaque stage
Dense, subepidermal, band-like infiltrate with many cerebriform lymphocytes
Epidermotropism is more prominent with
Intraepidermal clusters and Pautrier microabscesses
Confluent Pautrier microabscesses that can result in subcorneal and subepidermal bullae
Tumor stage
Dermal infiltrate becomes more diffuse and prominent
Tumor cells range in size from small to large
Epidermotropism may be lost
Large cell transformation
Often occurs in tumor stage
Large tumor cells ≥ 25%
CD30 can be (+); high proliferation rate (Ki-67)
MF variants
Pagetoid reticulosis
Intraepidermal proliferation of neoplastic T cells
Sponge-like disaggregation of epidermis
Atypical cells have medium-sized or large, sometimes hyperchromatic and cerebriform nuclei
CD4(+), CD8(-), or CD4(-), CD8(+)
Often CD30(+); Ki-67 > 30%
Folliculotropic MF (pilotropic MF)
Atypical lymphocyte infiltrating epithelium of hair follicles
Infiltrate spares epidermis
Often associated with mucinosis (mucinous degeneration)
Syringotropic MF
Hyperplastic eccrine ducts and glands infiltrated by atypical lymphocytes
Often abundant eosinophils present
Granulomatous slack skin
Dense granulomatous dermal infiltrate containing atypical T cells, macrophages, and often many multinucleated giant cells
Infiltrate often shows destruction of elastic tissue; ± epidermotropism
CD4(+), CD8(-)
Histologic Features of Lymph Nodes
Best to biopsy lymph nodes draining area of involved skin or lymph node with highest standardized uptake value on FDG PET scan
Early involvement by MF (N1 and N2)
Lymph node architecture is well maintained
Dermatopathic changes common
Cerebriform lymphocytes are either absent, singly scattered, or in small clusters or aggregates
Often difficult to identify morphologically
Ancillary testing is important to demonstrate involvement by MF
Flow cytometric immunophenotyping
Assessment for TCR gene rearrangement
Extensive involvement by MF (N3)
Overt involvement or complete effacement of architecture
May show large cell transformation
Cytologic Features
Small- to medium-sized lymphocytes
Cerebriform nuclear contours and hyperchromatic nuclei
ANCILLARY TESTS
Immunohistochemistry
CD2(+), CD3(+), CD5(+), βF1(+)
Often shows CD7 loss (all disease stages)
CD4(+), CD8(-)
Rare cases can be CD4(-), CD8(+)
CD45/LCA(+), CLA(+), CD52(+), CD25(-/+)
CD30(+/-), usually expressed by large cells
Ig(-), B-cell antigens(-)
Flow Cytometry
Can be performed on skin, peripheral blood, lymph nodes, and other tissue specimens
Flow panel should include
CD2, CD3, CD4, CD5, CD7
CD8, CD25, CD26, TCR-αβ, TCR-γδ
CD4:CD8 ratio is often increased
Typical immunophenotype: CD3(+), CD4(+), CD8(-), CD5(+), TCR-αβ(+)
Frequent immunophenotypic aberrancies
CD26(-), loss of/decreased CD7
Dim expression of CD2, CD3, CD4, or CD5
Clonality assessment by Vβ analysis
Can identify clonality and quantify clonal T cells
Can be used to follow treatment response
Cytogenetics
Complex karyotypes occur in subset of patients
Most common in patients with advanced-stage disease
Molecular Genetics
Monoclonal TCR gene rearrangements
No evidence of monoclonal Ig gene rearrangements
Inactivation of P16/CDKN2A or PTEN in subsets of cases
Gene Expression Profiling
Deregulation of genes involved in tumor necrosis factor (TNF) signaling pathway
DIFFERENTIAL DIAGNOSIS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree