Patient Stories
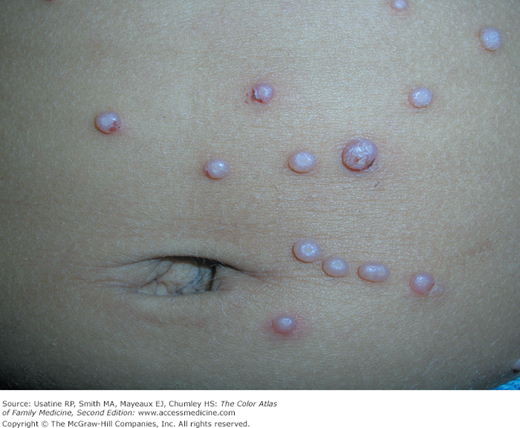
An 8-year-old girl is brought to the office because of an outbreak of bumps on her face for the past 3 months (Figure 130-1). Occasionally she scratches them, but she is otherwise asymptomatic. The mother and child are unhappy with the appearance of the molluscum contagiosum and chose to try topical imiquimod 5% cream. Fortunately, her health insurance covered this expensive treatment. A topical treatment was chosen to avoid the risk of hypopigmentation that can occur in dark-skinned individuals with cryotherapy.
An 11-year-old girl was also seen with molluscum on her face. The child and her mother decided to try cryotherapy as her treatment. She very bravely tolerated the treatment with liquid nitrogen in a Cryogun (Figure 130-2). The molluscum disappeared without scarring or hypopigmentation after two treatments.
Introduction
Epidemiology
- Molluscum contagiosum infection has been reported worldwide. An Australian seroepidemiology study found a seropositivity rate of 23%.1
- Up to 5% of children in the United States have clinical evidence of molluscum contagiosum infection.2 It is a common, nonsexually transmitted condition in children (Figures 130-1, 130-2, 130-3, 130-4).
- The number of cases in U.S. adults increased in the 1980s, probably as a result of the HIV/AIDS epidemic. Since the introduction of highly active antiretroviral therapy (HAART), the number of molluscum contagiosum cases in HIV/AIDS patients has decreased substantially.3 However, the prevalence of molluscum contagiosum in patients who are HIV-positive may still be as high as 5% to 18% (Figures 130-5 and 130-6).4,5
- In adults, molluscum occurs most commonly in the genital region (Figure 130-7). In this case, it is considered a sexually transmitted disease. Subclinical cases may occur and may be more common in the general community than is generally recognized.
Etiology and Pathophysiology
- Molluscum contagiosum is a benign condition that is often transmitted through close contact in children and through sexual contact in adults.
- It is a large DNA virus of the Poxviridae family of poxvirus. It is related to the orthopoxviruses (variola, vaccinia, smallpox, and monkeypox viruses).
- Molluscum replicates in the cytoplasm of epithelial cells. It causes a chronic localized skin infection consisting of dome-shaped pearly papules on the skin. Like most of the viruses in the poxvirus family, molluscum is spread by direct skin-to-skin contact. It can also spread by autoinoculation when scratching, touching, or treating lesions.
- Any one single lesion is usually present for approximately 2 months, but autoinoculation often causes continuous crops of lesions.
Risk Factors
- Common childhood disease.
- Molluscum contagiosum may be more common in patients with atopic dermatitis (Figure 130-8).2
- The disease also may be spread by participation in contact sports.2
- It is also associated with immunodeficient states such as in HIV infection (Figures 130-5 and 130-6) and with immunosuppressive drug treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree