Mixed Cellularity Hodgkin Lymphoma
C. Cameron Yin, MD, PhD
Key Facts
Terminology
Subtype of classical Hodgkin lymphoma (CHL) with diffuse or interfollicular pattern, without nodular fibrosis
Etiology/Pathogenesis
Epstein-Barr virus (EBV) appears to play pathogenic role in EBV(+) cases
HIV infection predisposes to development of EBV-associated CHL, mainly mixed cellularity CHL
Considered preapoptotic germinal center B cell
Clinical Issues
Accounts for 20-25% of CHL
Most patients present with stages II or III disease
Clinical and laboratory parameters are more relevant to prognosis and to determine mode of therapy
Microscopic Pathology
Complete or partial effacement of nodal architecture
Diagnostic Hodgkin and Reed-Sternberg (HRS) cells are readily identifiable
Ancillary Tests
CD30(+) in 100%; CD15(+) in ˜ 80% of cases
Epstein-Barr virus (EBV) latency type II infection
Monoclonal Ig gene rearrangements in HRS cells using single-cell analysis
Top Differential Diagnoses
Peripheral T-cell lymphoma
T-cell/histiocyte-rich large B-cell lymphoma
Lymphocyte-depleted Hodgkin lymphoma
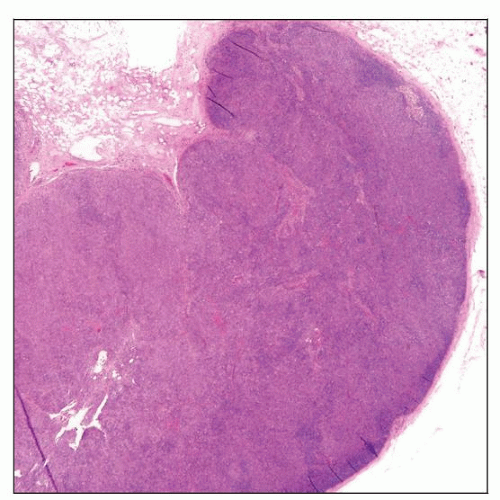 Mixed cellularity Hodgkin lymphoma (MCHL) involving lymph node. A low-power view shows diffuse effacement of the lymph node architecture. |
TERMINOLOGY
Abbreviations
Mixed cellularity Hodgkin lymphoma (MCHL)
Synonyms
Mixed cellularity classical Hodgkin lymphoma
Mixed cellularity Hodgkin disease
Definitions
Classical Hodgkin lymphoma (CHL) is a lymphoid neoplasm composed of Hodgkin and Reed-Sternberg (HRS) cells in a variable inflammatory background
Mixed cellularity is a type of CHL composed of classic HRS cells in a heterogeneous inflammatory cell background
MCHL has a diffuse or interfollicular pattern without nodules or fibrosis
ETIOLOGY/PATHOGENESIS
Infectious Agents
Epstein-Barr virus (EBV) is present in HRS cells in ˜ 75% of cases and has pathogenic role
HIV infection predisposes to development of EBV-associated CHL and often MCHL
Pathogenesis
HRS cells arise from late germinal center or early post-germinal center B cells that
Have undergone immunoglobulin gene (Ig) rearrangements with somatic mutations
Have undergone crippling Ig mutations in a subset of cases
Lack B-cell antigen receptors
HRS cells lose much of the normal B-cell immunophenotype due to
Severe impairment of transcription factor network that regulates B-cell gene expression
Low or undetectable levels of transcription factors: OCT2, BOB1, PU.1, and early B-cell factor (EBF)
Leads to low level of Ig transcripts in HRS cells
Made worse by epigenetic silencing (promoter hypermethylation) of Ig transcription
Impaired function of early B-cell development transcription factors: pax-5, E2A, and EBF
Overall, these abnormalities physiologically should lead to apoptosis
Development of antiapoptotic mechanisms to achieve survival
Dysregulation of many signaling pathways
Expression of EBNA1 and latent membrane proteins LMP1 and LMP2a
Role of microenvironment
Reactive cellular infiltrate is induced, in part, by HRS cells
Protects HRS cells from apoptosis
HRS cells produce a variety of cytokines, chemokines, and growth factors
CLINICAL ISSUES
Epidemiology
Incidence
Accounts for 20-25% of CHL cases in developed countries
Most common type of CHL in underdeveloped countries
Age
Median: 38 years
Gender
Male to female ratio is 2:1
Site
Cervical and supraclavicular lymph nodes
Mediastinal involvement is uncommon
Spleen (˜ 30%), bone marrow (˜ 10%), and liver (˜ 3%)
Presentation
B symptoms are common
Patients usually present with peripheral lymphadenopathy
Abdominal lymph nodes common; often with splenic involvement
Most patients present with stage II or III disease
Treatment
Current chemotherapy &/or radiation can cure disease in many patients
Chemotherapy with or without radiation
ABVD: Adriamycin (doxorubicin), bleomycin, vinblastine, and dacarbazine
Prognosis
Clinical and laboratory parameters are relevant to predicting prognosis and determining mode of therapy
Recent study suggests that number of histiocytes in background predicts prognosis
IMAGE FINDINGS
General Features
Lymphadenopathy
MICROSCOPIC PATHOLOGY
Histologic Features
Complete or partial effacement of lymph node architecture
Interfollicular pattern can occur
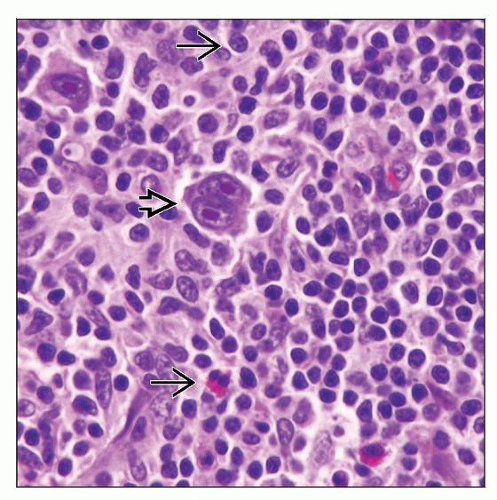
HRS cells
Readily identifiable with classic features
Reed-Sternberg cells are bilobed with large eosinophilic nucleoli and perinuclear halo
Hodgkin cells are mononuclear cells with large eosinophilic nucleolus and perinuclear halo
Background infiltrate
Variable mixture of small lymphocytes, plasma cells, histiocytes, eosinophils, &/or neutrophils
Histiocytes can be singly scattered or present as illdefined or epithelioid granulomas
Occasional foci of necrosis
Mild to moderate interstitial fibrosis may be present
No nodular collagen bands; no thickening of lymph node capsule
Cytologic Features
HRS cells in inflammatory background can be appreciated in fine needle aspiration smears
Immunophenotype can be assessed in cell block
Difficult to determine type as MCHL versus other types of CHL
ANCILLARY TESTS
Immunohistochemistry
CD30(+) > 95%; CD15(+) in ˜ 70-80% of cases
Characteristic membranous pattern with accentuation in Golgi area
pax-5(dim +) ˜ 90%, CD20 (variable +) ˜ 20%, CD79a(+) ˜ 10-20%
Ki-67(+), p53(+), MUM1(+)
CCL17(TARC)(+), fascin(+/-), Bcl-2(+/-)
OCT2(-/+), BOB1(-/+), PU.1(-)
CD45/LCA(-), EMA(-), Ig(-), clusterin(-)
EBV(+) latency type II pattern in ˜ 75% of cases
T-cell antigens can be aberrantly expressed by HRS cells in small subset of cases
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree