2 Mitral regurgitation
Salient features
History
• Asymptomatic or mild symptoms: often
• Shortness of breath (from pulmonary congestion)
• Fatigue (from low cardiac output)
• Palpitation (from atrial fibrillation or LV dysfunction)
• Fluid retention (in late-stage disease)
• Obtain a history of myocardial infarction, rheumatic fever, connective tissue disorder, infective endocarditis.
Examination
• Peripheral pulse may be normal or jerky (i.e. rapid upstroke with a short duration).
• Apex beat will be displaced downwards and outwards and will be forceful in character.
• First heart sound will be soft.
• Third heart sound is common (left ventricular gallop sound).
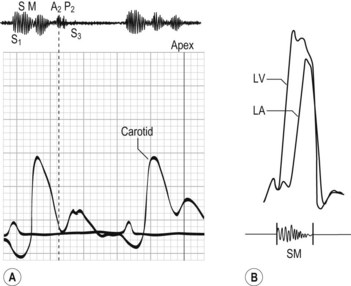
• Pansystolic murmur (Hope murmur) (Fig. 2.1) conducted to the axilla, best detected with the diaphragm and on expiration. (Note: It is important to be sure that there is no associated tricuspid regurgitation.)
• Loud pulmonary second sound and left parasternal heave when there is associated pulmonary hypertension.
Questions
How would you investigate this patient?
• ECG: look for broad bifid P waves (P mitrale), left ventricular hypertrophy, atrial fibrillation. When coronary artery disease is the cause, there is often evidence of inferior or posterior wall myocardial infarction.
• Radiography can assess pulmonary congestion, large heart, left atrial enlargement and pulmonary artery enlargement (if severe and long-standing).
• Echocardiography determines the anatomy of the mitral valve apparatus, left atrial and left ventricular size and function (typical features include large left atrium, large LV, increased fractional shortening, regurgitant jet on colour Doppler, leaflet prolapse, floppy valve or flail leaflet). The echocardiogram provides baselines estimation of LV and left atrial volume, an estimation of left ventricular ejection fraction, and approximation of the severity of regurgitation. It can be helpful to determine the anatomic cause of mitral regurgitation. In the presence of even mild tricuspid regurgitation, an estimate of pulmonary artery pressure can be obtained.
• Transoesophageal echocardiogram is useful when transthoracic echocardiography provides non-diagnostic images. It may give better visualization of mitral valve prolapse. It is useful intraoperatively to establish the anatomic basis for mitral regurgitation and to guide repair.
• Cardiac catheterization is useful to determine coexistent coronary artery or aortic valve disease. Large ‘v’ waves are seen in the wedge tracing. Left ventriculogram and haemodynamic measurements are indicated when non-invasive tests are inconclusive regarding the severity of mitral regurgitation, LV function, or the need for surgery.
How would you differentiate between mitral regurgitation and tricuspid regurgitation?
| Mitral regurgitation | Tricuspid regurgitation | |
|---|---|---|
| Pulse | Jerky or normal | Normal |
| Jugular venous pressure | Prominent ‘v’ wave | |
| Palpation | Left ventricular heave | Left parasternal heave |
| Auscultation | Pansystolic murmur | Pansystolic murmur |
| Intensity increases with expiration | Intensity increases with inspiration | |
| Radiates to the axilla | ||
| Other signs | Hepatic pulsations |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree